Abstract
Purpose
P-glycoprotein (Pgp), an ATP-dependent transport protein, confers multidrug resistance in cancer cells. Tariquidar binds and inhibits Pgp. To assess the toxicity, pharmacokinetics (PK), and pharmacodynamics of tariquidar, we conducted a phase I trial of tariquidar in combination with doxorubicin, docetaxel, or vinorelbine in children and adolescents with recurrent or refractory solid tumors.
Methods
Patients less than 19 years of age with refractory or recurrent solid tumors were eligible. Tariquidar (1, 1.5, or 2 mg/kg) was administered alone and in combination with doxorubicin, docetaxel, or vinorelbine. PK of tariquidar and cytotoxic drugs was performed. Pgp function was assessed by a rhodamine efflux assay and 99mTc-sestamibi scintigraphy. Tumor Pgp expression was assessed by immunohistochemistry. Response was assessed using Response Evaluation Criteria in Solid Tumors.
Results
Twenty-nine subjects were enrolled. No tariquidar-related dose-limiting toxicity (DLT) was observed. DLT related to cytotoxic drugs occurred in 12 % of subjects receiving tariquidar 2 mg/kg. When administered in combination with tariquidar, the clearance of docetaxel and vinorelbine was reduced compared to prior studies. Inhibition of rhodamine efflux was dose dependent. After tariquidar administration, 99mTc-sestamibi accumulation in tumor increased by 22 %. Objective responses (1 complete, 2 partial) were observed. There was no association between tumor Pgp expression and response.
Conclusion
A tolerable and biologically active dose of tariquidar was established in children and adolescents. This trial demonstrates that modulators of resistance can be evaluated in combination with chemotherapy, and pharmacokinetic and pharmacodynamic endpoints can be useful in determination of recommended dose in children and adolescents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
P-glycoprotein (Pgp, ABC-B1), a plasma membrane glycoprotein, functions as an ATP-dependent drug efflux pump. Pgp expression in tumor cells confers multidrug resistance by preventing the intracellular accumulation of chemotherapeutic agents including anthracyclines, taxanes, vinca alkaloids, and epipodophyllotoxins. Inhibition of Pgp may reverse resistance by increasing tumor intracellular drug accumulation and exposure [18, 22].
Pgp is expressed in childhood cancers, including leukemia, rhabdomyosarcoma, osteosarcoma, retinoblastoma, Ewing sarcoma, and neuroblastoma. In central nervous system tumors, Pgp is expressed in tumor, in tumor blood vessels, and in the epithelium of the choroid plexus [29]. The role of Pgp in treatment outcome is controversial [1, 4, 5, 10]. In retrospective studies of rhabdomyosarcoma, osteosarcoma, retinoblastoma and neuroblastoma, tumor Pgp expression at diagnosis was associated with poor prognosis and undetectable expression correlated with durable remission [11]. However, associations with outcome have not been confirmed in prospective trials [35].
Tariquidar (molecular weight 646.7) inhibits the ATPase activity of the Pgp drug efflux pump. In vitro, tariquidar reverses intrinsic and acquired resistance to doxorubicin, vincristine, and paclitaxel with potency 10-fold greater than first-generation Pgp inhibitors including valspodar [23]. Tariquidar [17, 21] and structural analogs [26] also inhibit Breast Cancer Resistance Protein (BCRP/ABCG2). In adults, tariquidar was well tolerated. At the recommended dose (2 mg/kg IV over 30 min), maximum inhibition of Pgp measured by rhodamine uptake in CD56+ lymphocytes was observed and maintained for 24 h. The peak serum concentration (C max) was 2.3 µM, and area under the concentration time curve (AUC0–48) was 12.6 µM h, clearance was 160 mL/min/m2, and half-life was 26 h [7, 32].
In adults with refractory solid tumors, tariquidar was administered in combination with vinorelbine. In this combination, the maximum tolerated dose (MTD) of vinorelbine was 20 mg/m2, and the dose-limiting toxicities (DLT) were neutropenia, hypotension, and infection. Non-hematological toxicities were gastrointestinal (abdominal pain, anorexia, constipation, ileus, nausea, vomiting, and diarrhea) and fatigue. One patient with breast cancer had a minor response, and a second with renal cell cancer had a partial response [2]. In a phase II study in women with breast carcinoma, tariquidar was added to the ongoing taxane- or anthracycline-based regimens. One patient experienced severe toxicity. One woman who received tariquidar in combination with docetaxel and trastuzumab had a partial response [28]. Two phase III trials of tariquidar were initiated in patients with non-small cell lung cancer. Tariquidar or placebo was administered in combination with paclitaxel/carboplatin or in combination with vinorelbine. Both studies were closed due to chemotherapy-related toxicity in the tariquidar arm.
Clinical development of first-generation Pgp inhibitors was hampered by pharmacokinetic interactions with cytotoxic chemotherapy [9, 15]. In early clinical trials in adults, minor pharmacokinetic interactions were noted for tariquidar in combination with doxorubicin and paclitaxel, with systemic exposure increasing 26 and 44 %, respectively. No change in vinorelbine pharmacokinetics was observed. Due to the large inter-patient variability in the pharmacokinetics of these cytotoxic agents alone, the changes were not considered clinically significant [2, 20, 28].
In addition to over-expression in drug-resistant cancer cells, Pgp is present in normal tissues including renal proximal tubules, capillary endothelial cells in the blood–brain barrier, bile canaliculi, bone marrow stem cells, and peripheral blood mononuclear cells (CD56+ PBMC) [6, 13, 14, 24]. Substrates for Pgp are structurally and chemically diverse [25, 36]. In addition to chemotherapeutic agents, Pgp substrates include the fluorescent dye rhodamine and sestamibi. Rhodamine efflux from CD 56+ PBMCs by flow cytometry has been used to assess Pgp function in a number of clinical trials [2, 20, 30, 32]. 99mTc-sestamibi scintigraphy, traditionally used to evaluate cardiac function, has been used to assess Pgp function in tumors and normal tissues of patients receiving tariquidar by comparing time activity curves (TAC) in tumor, liver (positive control), lung (negative control), and heart [3]. Cardiac muscle does not express Pgp; therefore, accumulation and retention of 99mTc-sestamibi are not altered by Pgp antagonists, and the heart can be used to normalize TAC between scans. In tissue expressing Pgp, such as normal liver, intestine, or some tumors, the retention of 99mTc-sestamibi increases in the presence of Pgp antagonists [27].
Intrinsic and acquired drug resistance is a significant issue in pediatric solid tumors. Tariquidar is a potent and specific inhibitor of Pgp and has been tolerated in combination with chemotherapy in adults. We conducted a phase I trial of tariquidar in combination with doxorubicin, docetaxel, or vinorelbine in children and adolescents with recurrent or refractory solid tumors. The primary objective was to determine the maximum tolerated or recommended dose and toxicity profile of tariquidar in this population. Secondary objectives were to study the pharmacokinetics of tariquidar alone and in combination with chemotherapy. Pgp function was assessed using the rhodamine efflux flow cytometry assay in PBMC and by functional imaging using 99mTc-sestamibi scintigraphy and immunohistochemical staining of archival tumor samples to examine Pgp expression in tumors.
Methods
Eligibility
Children and adolescents >2 years and less than 19 years of age were eligible if they had a solid tumor that was recurrent or refractory to standard treatment. Subjects must have recovered from the toxic effects of prior therapy and have an ECOG performance status of ≤2. Prior to enrollment, subjects must have met criteria for time intervals from prior anticancer and supportive therapy (Supplemental Table 1). Children and adolescents with brain tumors receiving corticosteroids had to be on a stable or decreasing corticosteroid dose. All subjects were required to have an absolute neutrophil count ≥1500/µL, hemoglobin >8 gm/dL, and platelet count ≥100,000/µL, normal electrocardiogram, bilirubin ≤1.5 × upper limit of normal, alanine aminotransferase (ALT) <2.5 × the upper limit of normal, and a normal age-adjusted serum creatinine or a creatinine clearance ≥60 mL/min/1.73 m2.
For participants who received tariquidar in combination with doxorubicin, normal left ventricular ejection fraction was required and the prior cumulative anthracycline dose was restricted. In participants who received prior anthracycline as a bolus injection without a cardioprotectant (e.g., dexrazoxane) or if the subject had mediastinal radiation, the lifetime cumulative dose of anthracycline could not exceed 300 mg/m2 at enrollment. For participants who received prior anthracycline as a continuous infusion or with a cardioprotectant and no mediastinal radiation, the cumulative lifetime dose of anthracycline could not exceed 400 mg/m2 at enrollment.
Patients receiving other investigational agents were excluded, as were pregnant or breast-feeding females and patients with clinically significant unrelated systemic illness that would compromise data analysis or interpretation.
This trial was conducted under an investigator IND at the Pediatric Oncology Branch of the NCI and approved by the NCI Institutional Review Board. The use of radiation for research was approved by the NIH Radiation Safety Committee. The trial was registered with clinicaltrials.gov (NCT00011414). All subjects or their legal guardians provided informed consent, and participants provided verbal assent for protocol therapy and research tests.
Treatment regimen and dose escalation
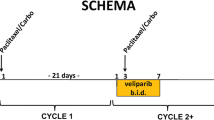
Tariquidar (Xenova, LP) was administered intravenously (IV) over 30 min. The starting dose was 1 mg/kg/dose with escalation to 1.5 and 2 mg/kg in subsequent cohorts. During cycle 1, tariquidar was administered as a single agent, and then at least 48 h later, tariquidar was administered 60 min prior to chemotherapy (Fig. 1). For each participant, the chemotherapy regimen was chosen based on the histology of the tumor and their prior therapy. On subsequent cycles, tariquidar was administered in combination with chemotherapy. All participants received filgrastim (5 mcg/kg subcutaneously) beginning 48 h after chemotherapy. Participants receiving doxorubicin received dexrazoxane. For subjects enrolled at the 1 or 1.5 mg/kg dose level, intra-subject dose escalation was permitted if the participant successfully completed two cycles at the enrollment dose, had at least stable disease, and did not experience dose-limiting toxicity attributable to tariquidar. Treatment cycles were 21 days in duration, but could be extended to 28 days to allow for participants to recover from toxicity. For participants who had stable disease or a response and did not experience toxicity that required discontinuation of protocol therapy, there was no limit on the number of cycles of therapy that could be administered. However, if a subject receiving doxorubicin reached a maximum lifetime cumulative anthracycline dose (500 mg/m2) but was otherwise eligible to continue protocol therapy, the subject could switch their cytotoxic agent to docetaxel or vinorelbine for subsequent cycles.
Cohorts of 3–6 subjects were treated at each tariquidar dose level. When a minimum of three subjects who were evaluable for toxicity completed one cycle of therapy at a dose level without evidence of dose-limiting toxicity, subsequent participants were enrolled at the next higher dose level. At the recommended dose of tariquidar, the study was expanded to treat up to six participants with each chemotherapeutic agent.
Monitoring for treatment-related toxicity included weekly physical examination, serum chemistries, and twice weekly complete blood counts. For participants receiving doxorubicin, echocardiogram was performed at baseline and then prior to each doxorubicin-containing cycle. Disease assessment was performed at baseline, prior to cycle 2, and then prior to every other cycle. After cycle 14, disease assessments were done after every fourth cycle.
Definition of dose-limiting toxicity (DLT) and maximum tolerated dose (MTD)
In children, the acute toxicity profile of doxorubicin, vinorelbine, and docetaxel are well documented [8, 16, 19, 31]. Known toxicities of these anticancer agents do not overlap with tariquidar toxicity observed in adults. Toxicities attributable to cytotoxic agents that were within the expected severity range were not considered dose limiting. Hematological toxicity was attributed to the anticancer agent.
Clinical and laboratory adverse events were graded according to the NCI Common Toxicity Criteria version 2 (http://ctep.info.nih.gov). Hematological dose-limiting toxicity (H-DLT) was defined as grade 4 neutropenia (<500/µL) of 5 or more days duration or grade 4 thrombocytopenia (<10,000/µL) occurring on 2 or more days of the cycle. Platelet transfusion administered for a platelet count less than 20,000/µL but greater than 10,000/µL was considered grade 4 thrombocytopenia. In addition, failure to recover a neutrophil or platelet count to greater than or equal to 1500 or 100,000/µL, respectively, by day 28 of the treatment cycle was considered H-DLT. Non-hematological DLT included any grade 3 or 4 non-hematological toxicity or failure to recover to grade ≤1 toxicity or to baseline by day 28 of the treatment cycle.
The maximum tolerated dose (MTD) of tariquidar was determined from DLT occurring during cycle 1. The MTD was the dose level immediately below the dose level at which ≥2 patients in a cohort (dose level) of 2–6 patients experienced a DLT. The dose was not escalated above the recommended dose in adults (equivalent to 2 mg/kg). In the expanded cohort of subjects treated at the MTD or recommended dose of tariquidar, if less than 20 % experienced a DLT, the tariquidar dose would be considered tolerable in combination with chemotherapy.
Participants who experienced tariquidar-related DLT were offered up to two dose reductions during subsequent cycles if they had benefited from the prior protocol treatment. The doxorubicin, vinorelbine, or docetaxel dose was reduced by 30 % on subsequent treatments cycles for dose-limiting hematological toxicity or any grade ≥3 non-hematological toxicity except for grade 3 nausea or vomiting. In addition, vinorelbine was discontinued in participants who experienced grade ≥2 neuropathy or constipation that did not diminish to grade ≤1 by day 28 of a treatment cycle. Docetaxel was discontinued in participants who experienced anaphylaxis or grade ≥2 neuropathy or peripheral edema that did not resolve to grade ≤1 by cycle day 28.
Pharmacokinetic and pharmacodynamic studies
Pharmacokinetic evaluation of tariquidar alone (day 1) and in combination with doxorubicin, docetaxel, or vinorelbine (day 3) was conducted. Serial whole blood samples were collected from a site distant from the drug infusion. Samples were placed on ice and centrifuged within 2 h of collection. Plasma was stored at −70 °C until analysis.
The plasma concentrations of tariquidar and cytotoxic drugs were measured using sensitive and specific methods (Supplementary data Table 2). Pharmacokinetic data were analyzed using non-compartmental methods. To determine whether tariquidar had a pharmacokinetic interaction with cytotoxic agents, the mean clearance of each cytotoxic agent was compared to published results in children [8, 12, 16, 19, 31, 33].
The rhodamine assay in CD56+ PBMCs was used as a surrogate measure of Pgp function [34]. Peripheral blood (6 mL) was obtained prior to and 24 h after administration of the first dose of tariquidar during cycle 1. Inhibition of rhodamine efflux was measured as previously described [30]. Flow cytometry analysis (FACSCalibur with CellQuest software; Becton–Dickinson, San Jose, CA) was performed using a live lymphocyte gate; 10,000 events per replicate were collected. The geometric mean fluorescence intensity (MFI) of intracellular rhodamine 123 in CD56+ lymphocytes was measured in the participant’s sample at baseline (no tariquidar) and 24 h after systemic tariquidar administration and control (participant’s baseline sample incubated ex vivo with 3 µM tariquidar). Percent inhibition of rhodamine efflux was calculated as the ratio of the MFI 24 h after systemic tariquidar administration: MFI of control (participant’s baseline sample incubated ex vivo with 3 µM tariquidar).
To describe the relationship of tariquidar dose to Pgp inhibition, the percent inhibition of rhodamine efflux was plotted as a function of dose and the data fit to maximum effect model (MLAB, Civilized Software, Bethesda, MD) using the equation:
where E max is the maximum effect, Dose50 is the dose producing 50 % E max, h is the slope of the sigmoid curve (the Hill Constant), and E min is the measured baseline effect.
99mTc-sestamibi scintigraphy, functional imaging to assess Pgp inhibition in normal tissue and tumor [3], was performed at baseline and 48 h after the first dose of tariquidar. 99mTc-sestamibi (0.29 mCi/kg, maximum 20 mCi) was administered and images acquired on a dual-headed camera (ADAC Laboratories, Milpitas, CA) using low-energy/high-resolution collimators at the 140 keV photopeak of 99mTc. Time activity curves (TAC) were generated in tumors, normal lung, liver, and heart and used to calculate the area under the concentration x time curve (AUC) for 0- to 3-h interval. The percent change in tissue:heart 99mTc-sestamibi AUC0–3h was calculated for each tissue (lung, liver, or tumor) as follows:
P-glycoprotein expression was assessed using immunohistochemistry with JSB-1 (Signet Laboratories, Cambridge MA) in paraffin-embedded formalin-fixed tumor from previous surgical resections or diagnostic biopsies. Cell lines known to be strongly positive (MCF7ADR) and negative (MCF7) for Pgp expression were used as controls. Tumor cells with membrane staining were scored by intensity as 0–3+.
Results
Twenty-nine subjects with median (range) age of 13 (2–18) years, 16 females and 13 males, were enrolled. Twenty-two subjects were Caucasian; 7 were black; 6 were Hispanic; 23 were non-Hispanic. The median (range) number of prior chemotherapy regimens was 3 (1–6); fifteen subjects received prior radiation. Subject characteristics are presented in Table 1. Three participants were not evaluable for toxicity due to rapid tumor progression during cycle 1. One participant who received two cycles of tariquidar in combination with doxorubicin prior to reaching the protocol-specified cumulative lifetime dose of doxorubicin (500 mg/m2), therefore, was switched to docetaxel in combination with tariquidar and remained on study for seven additional cycles. Median number of cycles of protocol therapy administered was 1 (range 1–31).
No DLT related to tariquidar was observed. Tariquidar-related toxicities observed during cycle 1 were grade 1 pruritus (n = 1) at dose level 2 and grade 1 nausea (n = 1), grade 1 dysgeusia (n = 3), grade 2 hypotension (n = 2), and grade 2 peripheral edema (n = 1) at dose level 3. No maximum tolerated dose was achieved. One participant met the criteria for intra-subject dose escalation, his tariquidar dose was increased from 1 mg/kg to 1.5 mg/kg, and he tolerated the increased dose without toxicity.
Serious toxicities related to each of the anticancer drugs during cycle 1 are presented in Table 2. Overall, DLT related to cytotoxic agents administered in combination with tariquidar (2 mg/kg) was 12 % (2/17); 20 % (1/5) for vinorelbine; 17 % (1/6) for doxorubicin; and 0 % (0/6) for docetaxel. Unexpected thrombocytopenia was observed in three participants receiving docetaxel in combination with tariquidar [8]. During cycle 2, subject 009 received tariquidar (1.5 mg/kg) in combination with vinorelbine and experience delayed neutrophil recovery, and the vinorelbine dose was reduced by 30 % (14 mg/m2). This subject received tariquidar in combination with vinorelbine for 30 additional cycles without recurrent or cumulative toxicity.
Pharmacokinetic and pharmacodynamic studies
Plasma pharmacokinetic parameters for tariquidar alone (day 1) and tariquidar in combination with anticancer agents (day 3) are presented in Table 3 along with the parameters for the chemotherapeutics agents administered with tariquidar. Pharmacokinetic parameters were highly variable. At all dose levels, the tariquidar Cmax when administered in combination with chemotherapy exceeded 2 µM. Overall, the clearance of docetaxel and vinorelbine was reduced compared to previously published results (Table 3).
Assessment of PgP function using rhodamine retention in CD56+ lymphocytes was completed prior to and 24 h after the first dose of tariquidar in all patients. Data from five patients were excluded due to inadequate recovery of live lymphocytes. The median (range) percent inhibition of rhodamine efflux was 22.5 (range 12.2–35.5), 54 (range 47–61), 63.5 (range 52–74), and 77 (range 66.2–86) at the control, 1, 1.5, and 2 mg/kg dose levels, respectively. A dose-dependent inhibition in rhodamine efflux was observed (Fig. 2). The maximum effect model fit to the data predicts a plateau of 80 % inhibition of Pgp function in CD56+ lymphocytes 24 h after administration of 2 mg/kg of tariquidar.
Rhodamine assay using flow cytometry to measure the intracellular rhodamine fluorescence in CD56+ staining cells. Dot plots of a patient’s cells at a baseline, b 24 h after systemic administration of 2 mg/kg of tariquidar, and c control (patient’s blood exposed ex vivo to 3 µM tariquidar for 1 h) are presented. CD56+ cells are in the upper portion of the graph (positive in FL2), and the intracellular rhodamine content is plotted on the FL1 axis. A histogram d of the mean fluorescent intensity of intracellular rhodamine (FL1) is presented at a baseline, b 24 h after systemic administration of tariquidar, and c control. For each patient, percent inhibition as a function of tariquidar dose is plotted and a maximum effect model of drug effect is fit to the data (e). Percent inhibition of Pgp in the rhodamine assay is dose dependent. At the 2 mg/kg dose level, the median percent inhibition was 77 %. The maximum effect model predicts maximal inhibition of 80 %
Six patients completed paired 99mTc-sestamibi scans, and two patients had tumors that were evaluable by 99mTc-sestamibi scintigraphy. In six patients, the median (range) percent change in 99mTc-sestamibi accumulation in lung was 15 % (3–22 %) and liver was 162 % (68–305 %). For patients with tumor evaluable by 99mTc-sestamibi scintigraphy, the percent change in tumor was 140 % in the hepatic metastasis (n = 1), 18 % in soft tissue metastatic sites (n = 2), and 28 % (14–40 %) in pulmonary nodules (n = 5). The enhanced uptake of tracer in the hepatic metastasis after tariquidar may in part be related to the increased uptake in normal liver tissue anterior and posterior to the metastatic lesion and may not reflect the actual change in the tumor uptake and retention.
Tumor Pgp expression determined by immunohistochemical staining using JSB-1 is presented in Table 1. Archival tumor specimens were available from 18 subjects. There was no association between Pgp-positive immunohistochemical staining of tumor and radiographic response.
Response
A 2-year-old with pancreatoblastoma and recurrent hepatic metastasis achieved a complete radiographic response by Response Evaluation Criteria in Solid Tumors (RECIST) after 16 cycles of tariquidar in combination with vinorelbine (Fig. 3). She continued on protocol therapy for 31 cycles and remains in continuous complete remission more than 5 years after completing therapy. This subject’s tumor had the highest tumor expression of Pgp (Table 1). Two patients experienced partial responses. A 14-year-old female with rhabdomyosarcoma with metastatic recurrence to her breast experienced a partial response after four cycles of doxorubicin in combination with tariquidar. She declined further protocol therapy and received local radiation therapy to achieve a complete response. She refused adjuvant chemotherapy, her disease recurred, and she died of complications of recurrent rhabdomyosarcoma. A 7-year-old male with metastatic adrenocortical carcinoma experienced a partial response during two cycles of therapy with tariquidar in combination with doxorubicin. Due to his cumulative dose of doxorubicin, his therapy was switched to docetaxel in combination with tariquidar and after seven additional cycles was removed from protocol therapy due to progressive disease.
Subject 009, a 2-year-old female with recurrent pancreatoblastoma, had recurrent tumor in liver (abdominal CT baseline, a), and a complete radiographic and clinical response was confirmed after 16 cycles of tariquidar in combination with vinorelbine (b). c Immunohistochemistry staining for Pgp at initial diagnosis and at relapse prior to enrollment on this study (d) in this subject. This subject completed 31 cycles of therapy without cumulative toxicity and remains free of disease more than 5 year after completion of therapy
Discussion
In children and adolescents, toxicities related to tariquidar were mild and included transient hypotension, taste disturbance, and nausea. No dose-limiting toxicities were observed when tariquidar was administered alone. The pharmacokinetics of tariquidar were highly variable. At all dose levels, the Cmax of tariquidar exceeded the concentration required for maximal inhibition of Pgp in CD56+ lymphocytes in prior studies. The inhibition of rhodamine efflux from CD56+ lymphocytes 24 h after systemic administration of tariquidar was dose dependent. At the 2 mg/kg dose level, the median percent inhibition was 77 %. Using a maximum effect model of drug effect fit to the data, we predict maximal inhibition of rhodamine efflux is 80 %. Therefore, based on this surrogate assay, increasing the dose of tariquidar above 2 mg/kg is unlikely to increase Pgp inhibition. Using functional imaging to assess Pgp function, we observed that 99mTc-sestamibi accumulation in the liver, which expresses Pgp, and in some tumors increased after tariquidar administration. Whereas 2 mg/kg was well tolerated and biologically active by our surrogate biomarker endpoint, we conclude that the recommended dose of tariquidar in children is 2 mg/kg IV over 30 min.
In children, the clearance of docetaxel and vinorelbine administered with tariquidar was less than previously reported. Reduced total body clearance resulting in increased drug exposure (AUC) could contribute to the unexpected toxicity of docetaxel and vinorelbine when administered in combination with tariquidar. Of the nine participants who received tariquidar in combination with docetaxel, three (33 %) experienced grade 3 thrombocytopenia (platelet count ≥10,000, <50,000/µL). In a prior dose finding study of single-agent docetaxel (150–235 mg/m2) in children and adolescents with refractory solid tumors, platelet counts less than 50,000/µL were not observed [8, 31]. In addition, gastrointestinal toxicity (grade 3 nausea, vomiting, and constipation) associated with vinorelbine in combination with tariquidar may be more prevalent than previously reported for vinorelbine alone [19].
A limitation of the functional imaging studies performed in this trial was the use of planar imaging. The results confounded by activity overlying and underlying foci of disease, and by attenuation of photons by overlying and underlying normal tissues decreases sensitivity, particularly for low-intensity lesions. Thus, the percent change in sestamibi uptake in the liver metastases in this study likely reflects increased uptake in overlying and underlying normal liver tissue. These limitations could be significantly mitigated through the use of SPECT CT or 94mTc-sestamibi PET CT. The limitations of immunohistochemical staining for Pgp included the use of archival tissue and the very high expression of Pgp of our positive control cells, MCF7 ADR. Therefore, we may have underestimated the Pgp expression in tumors in children and adolescents participating in this study.
In this trial, we identified a tolerable and biologically active dose of a specific Pgp inhibitor, tariquidar, in children and adolescents. We did not identify an association between tumor Pgp expression by immunohistochemistry and clinical response. The prognostic significance of Pgp in childhood cancers remains controversial, and the availability of tariquidar for additional clinical trials is limited. However, this trial demonstrates that modulators of resistance can be evaluated in combination with chemotherapy and that pharmacokinetic and pharmacodynamic correlates can be useful in establishing the optimal dose.
References
Abraham EH, Prat AG, Gerweck L, Seneveratne T, Arceci RJ, Kramer R, Guidotti G, Cantiello HF (1993) The multidrug resistance (mdr1) gene product functions as an ATP channel. Proc Natl Acad Sci U S A 90:312–316
Abraham J, Edgerly M, Wilson R, Chen C, Rutt A, Bakke S, Robey R, Dwyer A, Goldspiel B, Balis F, Van Tellingen O, Bates SE, Fojo T (2009) A phase I study of the P-glycoprotein antagonist tariquidar in combination with vinorelbine. Clin Cancer Res 15:3574–3582
Agrawal M, Abraham J, Balis FM, Edgerly M, Stein WD, Bates S, Fojo T, Chen CC (2003) Increased 99mTc-sestamibi accumulation in normal liver and drug-resistant tumors after the administration of the glycoprotein inhibitor, XR9576. Clin Cancer Res 9:650–656
Arceci RJ (1993) Clinical significance of P-glycoprotein in multidrug resistance malignancies. Blood 81:2215–2222
Arceci RJ (2000) Can multidrug resistance mechanisms be modified? Br J Haematol 110:285–291
Bauer M, Karch R, Zeitlinger M, Stanek J, Philippe C, Wadsak W, Mitterhauser M, Jager W, Haslacher H, Muller M, Langer O (2013) Interaction of 11C-tariquidar and 11C-elacridar with P-glycoprotein and breast cancer resistance protein at the human blood–brain barrier. J Nucl Med 54:1181–1187
Bauer M, Zeitlinger M, Todorut D, Bohmdorfer M, Muller M, Langer O, Jager W (2013) Pharmacokinetics of single ascending doses of the P-glycoprotein inhibitor tariquidar in healthy subjects. Pharmacology 91:12–19
Blaney SM, Seibel NL, O’Brien M, Reaman GH, Berg SL, Adamson PC, Poplack DG, Krailo MD, Mosher R, Balis FM (1997) Phase I trial of docetaxel administered as a 1-hour infusion in children with refractory solid tumors: a collaborative pediatric branch, National Cancer Institute and Children’s Cancer Group trial. J Clin Oncol 15:1538–1543
Boote DJ, Dennis IF, Twentyman PR, Osborne RJ, Laburte C, Hensel S, Smyth JF, Brampton MH, Bleehen NM (1996) Phase I study of etoposide with SDZ PSC 833 as a modulator of multidrug resistance in patients with cancer. J Clin Oncol 14:610–618
Bradshaw DM, Arceci RJ (1998) Clinical relevance of transmembrane drug efflux as a mechanism of multidrug resistance. J Clin Oncol 16:3674–3690
Chan HS, Grogan TM, DeBoer G, Haddad G, Gallie BL, Ling V (1996) Diagnosis and reversal of multidrug resistance in paediatric cancers. Eur J Cancer 32A:1051–1061
Clarke SJ, Rivory LP (1999) Clinical pharmacokinetics of docetaxel. Clin Pharmacokinet 36:99–114
Deuchars KL, Ling V (1989) P-glycoprotein and multidrug resistance in cancer chemotherapy. Semin Oncol 16:156–165
Fojo AT, Ueda K, Slamon DJ, Poplack DG, Gottesman MM, Pastan I (1987) Expression of a multidrug-resistance gene in human tumors and tissues. Proc Natl Acad Sci U S A 84:265–269
Fojo T, Bates S (2003) Strategies for reversing drug resistance. Oncogene 22:7512–7523
Frost BM, Eksborg S, Bjork O, Abrahamsson J, Behrendtz M, Castor A, Forestier E, Lonnerholm G (2002) Pharmacokinetics of doxorubicin in children with acute lymphoblastic leukemia: multi-institutional collaborative study. Med Pediatr Oncol 38:329–337
Gardner ER, Smith NF, Figg WD, Sparreboom A (2009) Influence of the dual ABCB1 and ABCG2 inhibitor tariquidar on the disposition of oral imatinib in mice. J Exp Clin Cancer Res 28:99
Gottesman MM, Fojo T, Bates SE (2002) Multidrug resistance in cancer: role of ATP-dependent transporters. Nat Rev Cancer 2:48–58
Johansen M, Kuttesch J, Bleyer WA, Krailo M, Ames M, Madden T (2006) Phase I evaluation of oral and intravenous vinorelbine in pediatric cancer patients: a report from the Children’s Oncology Group. Clin Cancer Res 12:516–522
Kelly RJ, Draper D, Chen CC, Robey RW, Figg WD, Piekarz RL, Chen X, Gardner ER, Balis FM, Venkatesan AM, Steinberg SM, Fojo T, Bates SE (2011) A pharmacodynamic study of docetaxel in combination with the P-glycoprotein antagonist tariquidar (XR9576) in patients with lung, ovarian, and cervical cancer. Clin Cancer Res 17:569–580
Kuhnle M, Egger M, Muller C, Mahringer A, Bernhardt G, Fricker G, Konig B, Buschauer A (2009) Potent and selective inhibitors of breast cancer resistance protein (ABCG2) derived from the p-glycoprotein (ABCB1) modulator tariquidar. J Med Chem 52:1190–1197
Larsen AK, Escargueil AE, Skladanowski A (2000) Resistance mechanisms associated with altered intracellular distribution of anticancer agents. Pharmacol Ther 85:217–229
Martin C, Berridge G, Mistry P, Higgins C, Charlton P, Callaghan R (1999) The molecular interaction of the high affinity reversal agent XR9576 with P-glycoprotein. Br J Pharmacol 128:403–411
Montesinos RN, Moulari B, Gromand J, Beduneau A, Lamprecht A, Pellequer Y (2014) Coadministration of P-glycoprotein modulators on loperamide pharmacokinetics and brain distribution. Drug Metab Dispos 42:700–706
Pajeva IK, Sterz K, Christlieb M, Steggemann K, Marighetti F, Wiese M (2013) Interactions of the multidrug resistance modulators tariquidar and elacridar and their analogues with P-glycoprotein. ChemMedChem 10:1701–1713
Pick A, Klinkhammer W, Wiese M (2010) Specific inhibitors of the breast cancer resistance protein (BCRP). ChemMedChem 5:1498–1505
Pinwnica-Worms D (2000) Functional identification of multidrug resistance gene expression in vivo. Lippincott Williams & Wilkins, New Orleans
Pusztai L, Wagner P, Ibrahim N, Rivera E, Theriault R, Booser D, Symmans FW, Wong F, Blumenschein G, Fleming DR, Rouzier R, Boniface G, Hortobagyi GN (2005) Phase II study of tariquidar, a selective P-glycoprotein inhibitor, in patients with chemotherapy-resistant, advanced breast carcinoma. Cancer 104:682–691
Rao VV, Dahlheimer JL, Bardgett ME, Snyder AZ, Finch RA, Sartorelli AC, Piwnica-Worms D (1999) Choroid plexus epithelial expression of MDR1 P glycoprotein and multidrug resistance-associated protein contribute to the blood-cerebrospinal-fluid drug-permeability barrier. Proc Natl Acad Sci U S A 96:3900–3905
Robey R, Bakke S, Stein W, Meadows B, Litman T, Patil S, Smith T, Fojo T, Bates S (1999) Efflux of rhodamine from CD56+ cells as a surrogate marker for reversal of P-glycoprotein-mediated drug efflux by PSC 833. Blood 93:306–314
Seibel NL, Blaney SM, O’Brien M, Krailo M, Hutchinson R, Mosher RB, Balis FM, Reaman GH (1999) Phase I trial of docetaxel with filgrastim support in pediatric patients with refractory solid tumors: a collaborative Pediatric Oncology Branch, National Cancer Institute and Children’s Cancer Group trial. Clin Cancer Res 5:733–737
Stewart A, Steiner J, Mellows G, Laguda B, Norris D, Bevan P (2000) Phase I trial of XR9576 in healthy volunteers demonstrates modulation of P-glycoprotein in CD56+ lymphocytes after oral and intravenous administration. Clin Cancer Res 6:4186–4191
Thompson PA, Rosner GL, Matthay KK, Moore TB, Bomgaars LR, Ellis KJ, Renbarger J, Berg SL (2009) Impact of body composition on pharmacokinetics of doxorubicin in children: a Glaser Pediatric Research Network study. Cancer Chemother Pharmacol 64:243–251
Witherspoon SM, Emerson DL, Kerr BM, Lloyd TL, Dalton WS, Wissel PS (1996) Flow cytometric assay of modulation of P-glycoprotein function in whole blood by the multidrug resistance inhibitor GG918. Clin Cancer Res 2:7–12
Wunder JS, Bull SB, Aneliunas V, Lee PD, Davis AM, Beauchamp CP, Conrad EU, Grimer RJ, Healey JH, Rock MJ, Bell RS, Andrulis IL (2000) MDR1 gene expression and outcome in osteosarcoma: a prospective, multicenter study. J Clin Oncol 18:2685–2694
Zinzi L, Capparelli E, Cantore M, Contino M, Leopoldo M, Colabufo NA (2014) Small and innovative molecules as new strategy to revert MDR. Front Oncol 4:2
Acknowledgments
With sadness, we acknowledge the remarkable contributions of Dr Robert Arceci to our understanding of multidrug resistance and to the field of Pediatric Oncology.
Funding
The research was supported by the Intramural Research Program of the NIH, National Cancer Institute, Center for Cancer Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fox, E., Widemann, B.C., Pastakia, D. et al. Pharmacokinetic and pharmacodynamic study of tariquidar (XR9576), a P-glycoprotein inhibitor, in combination with doxorubicin, vinorelbine, or docetaxel in children and adolescents with refractory solid tumors. Cancer Chemother Pharmacol 76, 1273–1283 (2015). https://doi.org/10.1007/s00280-015-2845-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-015-2845-1