Abstract
Purpose
To investigate the influence of addition of docetaxel to neoadjuvant chemotherapy (NAC) with cisplatin plus 5-fluorouracil (CF) in patients with clinical stage III or T3 esophageal squamous cell carcinoma.
Methods
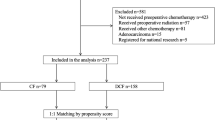
Information about 209 esophageal cancer patients with stage III or T3 disease, who underwent NAC consisting of CF with or without docetaxel, was reviewed. The survival outcomes were analyzed using the Kaplan–Meier method and propensity score-adjusted Cox proportional hazards models. The relevant variables were included in the propensity score model.
Results
NAC was administered to 149 patients in the CF group and 60 patients in the docetaxel plus CF (DCF) group. Overall, 129 patients treated with CF and 58 patients treated with DCF underwent surgery after NAC. The overall response rate was significantly higher in the DCF group compared with the CF group (61.0 vs. 43.2 %, p = 0.021). After matching, recurrence-free survival did not differ statistically between the CF and DCF groups [hazard ratio (HR) 0.83, 95 % confidence interval (CI) 0.50–1.37, p = 0.46]. After matching, the improvement in overall survival in the DCF group reached statistical significance (HR 0.49, 95 % CI 0.24–0.999, p = 0.050). No significant differences in rate of locoregional or distant recurrences were observed between the CF and DCF groups (53.0 vs. 48.3 %, p = 0.54).
Conclusions
NAC with DCF is superior to CF in patients with clinical stage III or T3 esophageal squamous cell carcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neoadjuvant chemotherapy (NAC) or chemoradiotherapy (CRT) followed by surgery is the standard treatment for resectable esophageal cancer. The Western world has seen a dramatic rise in adenocarcinomas of the esophagus in recent years. However, adenocarcinomas represent only 4.3 % of all esophageal cancers; the majority of esophageal carcinomas in Japan are squamous cell carcinomas [1]. The Japan Clinical Oncology Group (JCOG) has conducted several randomized phase III trials to establish new standard treatments for locally advanced esophageal cancer, defined as clinical stage IB–IIIC in the 7th edition of the Union for International Cancer Control (UICC) TNM classification. A randomized phase III trial (JCOG9204), which compared adjuvant chemotherapy with cisplatin plus 5-fluorouracil (CF) to surgery alone, showed the superiority of adjuvant chemotherapy with respect to disease-free survival [2]. A subsequent randomized phase III trial (JCOG9907) confirmed the survival benefit of NAC with CF compared to adjuvant CF chemotherapy [3]. The 5-year overall survival (OS) rate was 43 % in the adjuvant group and 55 % in the NAC group [hazard ratio (HR) 0.73, 95 % confidence interval (CI) 0.54–0.99, p = 0.04]. Therefore, NAC with CF is considered the current standard treatment for locally advanced esophageal cancer in Japan. However, JCOG9907 subgroup analyses revealed that NAC is not effective in patients with clinical stage III disease or T3 tumors. Thus, development of more intensive perioperative therapy is required for patients with clinical stage III disease or T3 tumors.
To further improve survival, a phase II trial that evaluated the addition of docetaxel to CF (DCF) in the NAC setting in patients with clinical stage II/III (UICC-TNM 6th edition) squamous cell carcinoma of the thoracic esophagus was conducted; this regimen yielded a good response rate (62.5–64.2 %) and 2-year OS rate (88.0 %), with no treatment-related deaths [4, 5]. NAC with DCF thus appears to be promising as preoperative treatment.
Only one retrospective report, which compared neoadjuvant CF with DCF in a small cohort of patients with clinical stage II–IV disease without distant metastases, has been published [6]. This report showed that neoadjuvant DCF provides significantly better OS compared with neoadjuvant CF. The objective of the present study was to investigate the influence of adding docetaxel to CF as neoadjuvant therapy in patients with clinical stage III or T3 esophageal squamous cell carcinoma.
Patients and methods
Patient population
This was a retrospective cohort study of esophageal cancer patients treated with NAC followed by surgery at Aichi Cancer Center Hospital between January 2003 and January 2013. A total of 209 patients met the following inclusion criteria: (1) carcinoma of the thoracic esophagus; (2) histological diagnosis of primary esophageal squamous cell carcinoma; (3) clinical stage III or T3 tumor (the 7th UICC-TNM classification); (4) no distant organ metastasis; (5) NAC consisting of CF or DCF; and (6) no previous thoracic radiotherapy (RT) or thoracic surgery. Patients who received neoadjuvant CRT followed by surgery were excluded from this analysis.
Pretreatment staging
Pretreatment staging evaluation included physical examination, laboratory tests, esophagogastroduodenoscopy, barium esophagography, and contrast-enhanced computed tomography (CT) from the neck to the upper abdomen. Pretreatment stage, based on the 6th edition of the AJCC Cancer Staging Manual until 2009 and based on the 7th edition after 2010, was determined during a meeting of thoracic surgeons, radiologists, gastroenterologists, and medical oncologists. Treatment strategies were also determined at the meeting.
Neoadjuvant chemotherapy and treatment assessments
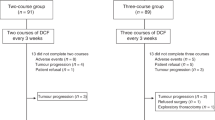
The CF regimen consisted of intravenous cisplatin (80 mg/m2) on day 1 followed by continuous infusion of 5-fluorouracil (800 mg/m2/day) for 5 days, given every 3 weeks for two cycles. The DCF regimen was based on the previous phase II study [4, 5] and consisted of intravenous docetaxel (60–70 mg/m2) and cisplatin (80 mg/m2) on day 1 followed by continuous infusion of 5-fluorouracil (750–800 mg/m2/day) for 5 days, given every 3–4 weeks for two to three cycles. Two DCF regimens were used: the lower-dose DCF regimen consisted of intravenous docetaxel (60 mg/m2) and cisplatin (60 mg/m2) on day 1 followed by continuous infusion of 5-fluorouracil (800 mg/m2/day) for 5 days, while the higher-dose DCF regimen consisted of intravenous docetaxel (70 mg/m2) and cisplatin (70 mg/m2) on day 1 followed by continuous infusion of 5-fluorouracil (750 mg/m2/day) for 5 days. Patients in the DCF group were given prophylactic antibiotics. Granulocyte colony-stimulating factor (G-CSF) was used if patients experienced grade 4 neutropenia or febrile neutropenia, but was not used for prophylaxis. Because few patients had measurable disease as determined by the Response Evaluation Criteria in Solid Tumors (RECIST), the treatment response of each primary esophageal lesion was endoscopically evaluated in patients without measurable disease and categorized as complete response (CR), partial response, stable disease, or progressive disease [7]. Partial response was defined as obvious morphological change, such as reduction in or flattening of the tumor or elevated lesion(s) around the ulcer, along with healing of the ulcer floor.
Surgery and histopathological response evaluation
Patients were scheduled to undergo surgery 4–8 weeks after the last day of NAC, when esophageal resection was defined as potentially curative. All patients underwent subtotal esophagectomy with regional lymphadenectomy through right thoracotomy and laparotomy, and reconstruction was performed using the stomach via a retrosternal route with cervical anastomosis through a neck incision. The entire tumor bed was cut into slices containing the entire esophageal wall, and histological therapeutic effects were classified as follows: grade 3, complete disappearance of viable cancer cells in the tumor bed; grade 2, disappearance of greater than two-thirds of viable cancer cells; and grade 1, disappearance of less than two-thirds of viable cancer cells [8].
History and physical examination, complete blood cell count, gastrointestinal endoscopy, chest X-ray, and CT scanning of the neck, chest, and abdomen were performed approximately every 3–6 months after initiation of treatment until death or until patients were lost to follow-up.
Data collection
The following information was recorded from the medical records and radiological images of each patient: treatment initiation date, age, gender, Eastern Cooperative Oncology Group performance status (ECOG PS), cancer site, primary tumor length, histopathological grade, clinical stage according to the AJCC 7th edition, serum albumin at pretreatment, clinical response, pathological stage, pathological margin, histological therapeutic effects, and final date of survival assessment.
Statistical analysis
All patient characteristics were considered categorical variables, with the exception of age and primary tumor length, which were treated as continuous data. Specific comparisons between groups were made using Chi-square and Mann–Whitney tests. OS was calculated from treatment initiation date to the time of death from any cause, or to time of last follow-up. Relapse-free survival (RFS), locoregional recurrence-free survival (LRFS), and distant recurrence-free survival (DRFS) were determined from treatment initiation date to documented date of first recurrence, to the time of death from any cause, or to time of last follow-up. Unmatched survival analyses were performed using the Kaplan–Meier method comparing survival curves with the log-rank test and unadjusted Cox proportional hazard models.
Multivariable adjusted Cox proportional hazards regression analyses were performed that included age, gender, PS, cancer site, primary tumor length, histopathological grade, clinical T stage (cT), number of lymph node metastases, serum albumin, and year of treatment (three groups). The propensity score was calculated using a multivariable logistic regression model with NAC regimen as the dependent variable and age, gender, PS, cancer site, primary tumor length, histopathological grade, cT, number of lymph node metastases, serum albumin, and year of treatment (three groups) as independent variables. The Cox proportional hazards models for OS and RFS were then adjusted using propensity score matching together with the aforementioned a priori-defined covariates. Therefore, the measure of association in this study was HR plus the 95 % CI. Statistical analyses were performed using STATA version 13 (Stata Corp LP, College Station, TX, USA) and R version 3.1.0 (R Project for Statistical Computing, Vienna, Austria). A p value less than 0.05 was considered statistically significant.
Results
Patient characteristics
Patient characteristics are summarized in Table 1. Of 209 consecutive esophageal cancer patients, 149 patients were treated with NAC with CF and 60 patients were treated with DCF. Most of the primary tumors were located in the mid-lower thoracic esophagus. The histological diagnosis of all tumors was squamous cell carcinoma. The histopathological grade values were significantly different among all patients (p = 0.020). In the DCF group, 28 patients received lower-dose DCF and 32 patients received higher-dose DCF. The median follow-up periods were 2.7 years (range 0.46–10.1) in all patients. The follow-up period was significantly longer in the CF group (p = 0.0026).
Response to chemotherapy
The overall response rate was significantly better in the DCF group than in the CF group (61.0 vs. 43.2 %, p = 0.021) (Table 2), but no significant difference in CR rate was observed between the two groups (3.4 vs. 4.7 %, p = 0.64). Overall, 129 (87 %) patients in the CF group and 58 (97 %) patients in the DCF group underwent surgery after NAC. In the CF group, 20 (13 %) patients underwent CRT instead of esophagectomy for the following reasons: Six patients were hopeful after achieving a CR, three patients refused to undergo surgery, and 11 patients had incurable disease. In the DCF group, two (3 %) patients underwent CRT instead of esophagectomy for the following reasons: one patient was hopeful after achieving a PR, and one patient had incurable disease.
No significant difference in R0 resection rate was observed between the CF and DCF group [80 % (119 of 149) vs. 80 % (48 of 60), p = 0.98]. Histological examination of primary lesions revealed that eight (6.2 %) of 129 patients in the CF group and seven (12.1 %) of 58 patients in the DCF group achieved a grade 3 histological postchemotherapeutic effect (Table 3, p = 0.23). Two (7.1 %) and five (16.7 %) patients who received lower- and higher-dose DCF, respectively, achieved a grade 3 histological postchemotherapeutic effect.
Survival
In the unadjusted situation, no statistically significant difference in median RFS was observed between the CF (2.1 years) and DCF (2.8 years) groups. The following RFS rates were observed: 1-year RFS rate, 60.9 versus 71.7 %, respectively; 2-year RFS rate, 51.1 versus 51.8 %, respectively; and 3-year RFS rate, 45.5 versus 39.9 %, respectively (HR 0.91, 95 % CI 0.60–1.37, p = 0.66). After matching, RFS did not differ statistically between the CF and DCF groups (HR 0.83, 95 % CI 0.50–1.37, p = 0.46) (Fig. 1a).
The OS difference also did not reach statistical significance in the unadjusted situation, but was higher in the DCF group compared with the CF group: median OS, not reached versus 4.7 years, respectively; 1-year OS rate, 93.1 versus 88.3 %, respectively; 2-year OS rate, 85.4 versus 70.6 %, respectively; and 3-year OS rate, 70.2 versus 59.9 %, respectively (HR 0.60, 95 % CI 0.33–1.07, p = 0.088). After matching, the higher OS in the DCF group reached statistical significance (HR 0.49, 95 % CI 0.24–0.999, p = 0.050) (Fig. 1b).
Patterns of postoperative recurrence
No significant differences in rates of locoregional or distant recurrences were observed between the CF and DCF groups (53.0 vs. 48.3 %, p = 0.54). The LRFS did not differ statistically between the CF and DCF groups (HR 0.80, 95 % CI 0.50–1.30, p = 0.385). Moreover, estimated LRFS rates at 1 and 2 years were 79.4 and 63.9 %, respectively, in the CF group, whereas they were 84.5 and 64.7 %, respectively, in the DCF group.
The DRFS did not differ statistically between the CF and DCF groups (HR 0.83, 95 % CI 0.49–1.43, p = 0.515). Moreover, estimated DRFS rates at 1 and 2 years were 73.6 and 68.2 %, respectively, in the CF group, whereas they were 81.6 and 74.9 %, respectively, in the DCF group.
With respect to treatment modality after recurrence, no significant differences were observed between the CF and DCF groups (Table 4).
Discussion
Although NAC or CRT followed by esophagectomy has been standard therapies for resectable esophageal cancer [9–13], the prognosis of esophageal cancer patients with advanced squamous cell carcinoma remains poor. The JCOG9907 study showed the superiority of NAC with CF with respect to OS compared with adjuvant chemotherapy in patients with resectable (non-T4) esophageal cancer [3]. Furthermore, subgroup analyses of the JCOG 9907 study suggested that NAC does not provide a survival benefit in patients with stage III disease or T3 tumors. We hypothesized that intensive preoperative chemotherapy could improve survival outcomes in patients with stage III disease or T3 tumors. The present results show that the RFS survival curve in the DCF group almost overlapped with the curve in the CF group, and that the DCF group had a favorable OS curve compared with that of the CF group. The 2-year RFS and LRFS rates were similar between groups, but the DCF group had a favorable 2-year DRFS rate compared with that of the CF group.
Ui et al. [6] reported that NAC with DCF improves histological response, progression-free survival, and OS compared with CF. Because patients with stage IV disease were included in this study analysis, the outcomes of patients treated with CF were poorer than in those who received CF in the JCOG9907 study. In contrast, the survival outcomes of patients treated with CF in the present study were similar to those of patients in the JCOG9907 study: The 3-year OS rate in the present study was 59.9 %, compared to 62.6 % in the JCOG9907 study.
Patients who receive neoadjuvant CRT and have a complete pathologic response experienced significantly improved survival [14]. In the present study, although the overall response rate was significantly better in the DCF group, histopathological findings revealed that pathological CR rate was similar between groups. An additional subgroup analysis showed that pathological CR rate was slightly higher in patients who received higher-dose DCF compared with those who received CF or lower-dose DCF. Higher-dose DCF therefore appears to improve survival outcomes.
In the Western world, neoadjuvant CRT followed by surgery is the standard treatment for resectable esophageal cancer [9]. We also hypothesized that reinforcement of systemic control with more intensive NAC is an additional strategy to improve survival of patients with locally advanced esophageal cancer. The addition of docetaxel to CF might lead to improvement in local control and reduce distant metastasis compared with neoadjuvant CRT. A slightly lower rate of distant metastasis was observed in patients treated with DCF; this result may be associated with the better OS observed in the matched analysis.
We recognize that the present study has several limitations. First, only squamous cell carcinomas were evaluated. A second limitation is that this was a retrospective study using a small number of patients. A third limitation is that the median follow-up period in the DCF group was 2.2 years. A fourth limitation is that propensity score adjustment can only be based on measured covariates and lacks inclusion of unmeasured potential confounders.
In conclusion, the results of the present study indicate that NAC with DCF is superior to CF in patients with clinical stage III or T3 esophageal squamous cell carcinoma. A three-arm randomized controlled trial comparing CF versus DCF versus CRT as NAC therapy for locally advanced esophageal cancer (JCOG1109, NExT study) is ongoing [15].
References
Tachimori Y, Ozawa S, Numasaki H et al (2015) Comprehensive registry of esophageal cancer in Japan, 2008. Esophagus 12:130–157
Ando N, Iizuka T, Ide H et al (2003) Surgery plus chemotherapy compared with surgery alone for localized squamous cell carcinoma of the thoracic esophagus: a Japan Clinical Oncology Group Study–JCOG9204. J Clin Oncol 21:4592–4596
Ando N, Kato H, Igaki H et al (2012) A randomized trial CF postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus neoadjuvant chemotherapy for clinical stage II/III squamous cell carcinoma of the thoracic esophagus (JCOG 9907). Ann Surg Oncol 19:68–74
Ura T, Nagase M, Fujii H et al (2010) Feasibility study of preoperative docetaxel (D), cisplatin (C), and fluorouracil (F) in esophageal cancer. ASCO Gastrointestinal Cancers Symposium, abstr 81
Hara H, Tahara M, Daiko H et al (2013) Phase II feasibility study of preoperative chemotherapy with docetaxel, cisplatin, and fluorouracil for esophageal squamous cell carcinoma. Cancer Sci 104:1455–1460
Ui T, Fujii H, Hosoya Y et al (2015) Comparison of preoperative chemotherapy using docetaxel, cisplatin and fluorouracil with cisplatin and fluorouracil in patients with advanced carcinoma of the thoracic esophagus. Dis Esophagus 28:180–187
Isono K, Uchida Y, Watanabe H et al (2004) Guidelines for clinical and pathologic studies on carcinoma of the esophagus, ninth edition: preface, general principles, part I. Esophagus 1:61–88
Japanese Society for Esophageal Diseases (2004) Guidelines for clinical and pathologic studies on carcinoma of the esophagus, ninth edition: preface, general principles, part II. Esophagus 1:107–125
van Hagen P, Hulshof MC, van Lanschot JJ et al (2012) Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 366:2074–2084
Stahl M, Walz MK, Stuschke M et al (2009) Phase III comparison of preoperative chemotherapy compared with chemoradiotherapy in patients with locally advanced adenocarcinoma of the esophagogastric junction. J Clin Oncol 27:851–856
Urschel JD, Vasan H (2003) A meta-analysis of randomized controlled trials that compared neoadjuvant chemoradiation and surgery to surgery alone for resectable esophageal cancer. Am J Surg 185:538–543
Herskovic A, Martz K, Al-Sarraf M et al (1992) Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus. N Engl J Med 326:1593–1598
Minsky BD, Pajak TF, Ginsberg RJ et al (2002) INT 0123 (Radiation Therapy Oncology Group 94-05) phase III trial of combined-modality therapy for esophageal cancer: high-dose versus standard-dose radiation therapy. J Clin Oncol 20:1167–1174
Donahue JM, Nichols FC, Li Z et al (2009) Complete pathologic response after neoadjuvant chemoradiotherapy for esophageal cancer is associated with enhanced survival. Ann Thorac Surg 87:392–398
Nakamura K, Kato K, Igaki H et al (2013) Three-arm phase III trial comparing cisplatin plus 5-FU (CF) versus docetaxel, cisplatin plus 5-FU (DCF) versus radiotherapy with CF (CF-RT) as preoperative therapy for locally advanced esophageal cancer (JCOG1109, NExT study). Jpn J Clin Oncol 43:752–755
Conflict of interest
None of the authors have identified a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nomura, M., Oze, I., Abe, T. et al. Impact of docetaxel in addition to cisplatin and fluorouracil as neoadjuvant treatment for resectable stage III or T3 esophageal cancer: a propensity score-matched analysis. Cancer Chemother Pharmacol 76, 357–363 (2015). https://doi.org/10.1007/s00280-015-2806-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-015-2806-8