Abstract
Venous thromboembolism (VTE) poses a significant challenge in the context of multiple myeloma, with an incidence of up to 10% in newly diagnosed patients and varying frequency in the relapsed/refractory setting. Accurate VTE risk assessment and personalized thromboprophylaxis strategies are important parts of supportive care in myeloma. There are three validated risk assessment models for prediction of VTE risk in newly diagnosed myeloma-SAVED, IMPEDE-VTE, and PRISM. In this review, we delve into the practical applications of VTE risk prediction models in the context of current therapies. By emphasizing the necessity of a tailored approach, we underscore the importance of considering patient-specific, disease-specific, and treatment-specific risk factors in each clinical scenario, and using that data to complement the output from risk assessment models. We also provide a summary of currently available data on VTE thromboprophylaxis in myeloma, and highlight specific situations where direct oral anticoagulants should be strongly considered. Our objective is to fill the critical gaps in VTE prophylaxis and management through the analysis of specific patient cases and provide a practical overview for clinicians.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma (MM) is a hematologic malignancy characterized by the clonal proliferation of plasma cells [1]. With significant improvements in the overall survival (OS) of patients with MM over the past two decades, optimizing the management of treatment-related toxicities has become a critical unmet need. Patients with MM experience significant disease-related complications as well as treatment-related toxicities during their disease course [2, 3]. Among these, venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), poses a major concern, especially in the first year after diagnosis [4,5,6,7]. VTE is a leading cause of morbidity in MM patients, and despite the routine use of thromboprophylaxis strategies, incidence rates remain high, with an estimated 10% risk in the first year after diagnosis [8,9,10,11,12,13,14,15]. In clinical trials involving patients with newly diagnosed, relapsed, or refractory myeloma treated with the immunomodulatory drug (IMiD) lenalidomide, the pooled incidence of VTE has been reported to be 6.2% (95% CI, 5.4–7.1%) over median treatment durations of 2–34 cycles, translating to 1.2 VTE events per 100 patient-cycles [16].
VTE can result in long-term complications such as post-thrombotic syndrome and chronic thromboembolic pulmonary hypertension [17]. Moreover, VTE can negatively impact the quality of life of MM patients and increase the burden on healthcare systems, resulting in frequent hospitalizations and treatment interruptions [18, 19]. Although a survival detriment from VTE is not clearly established in MM, many studies have reported an increased hazard ratio (HR) (up to 3-fold) for patients with thrombotic events compared to those without [13, 20, 21]. Similar outcomes are also seen for patients experiencing arterial thromboses [22].
The association between MM and VTE is multifactorial, with patient-related, disease-related, and treatment-related factors contributing to the increased risk [23, 24]. Patient-related factors include age, obesity, comorbidities (such as cardiovascular disease, diabetes, and hypertension), personal or family history of VTE, and immobilization [25, 26]. Disease-related factors encompass abnormal metaphase cytogenetics, the presence of other prothrombotic factors, and the production of procoagulant proteins by malignant plasma cells [12, 27,28,29,30]. Current treatment options for MM, such as immunomodulatory drugs (IMiDs) like lenalidomide and proteasome inhibitors (PIs) like carfilzomib, are also associated with an increased risk of VTE [31,32,33,34,35]. These factors collectively contribute to a hypercoagulable state, predisposing MM patients to a higher risk of VTE, and underscore the need for effective thromboprophylaxis approaches in MM patients receiving these therapies.
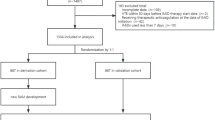
While the International Myeloma Working Group (IMWG) and European Myeloma Network Guidelines (EMN) offer recommendations for VTE prevention through routine thromboprophylaxis, significant VTE rates persist, possibly due to a mix of non-compliance and less-than-ideal risk stratification systems and thromboprophylaxis regimens [16, 36,37,38,39]. In this article, a case-based review of thromboprophylaxis in MM patients is presented, given the intricate nature and variability of individual patient profiles, treatment plans, and potential complications. Thromboprophylaxis strategies should be adapted to suit each patient’s distinct risk factors and clinical circumstances, as a one-size-fits-all approach may not be appropriate. Adopting a case-based methodology allows for a more in-depth understanding of the real-world challenges and decision-making processes associated with managing thromboprophylaxis in MM patients.
Case 1. Newly diagnosed MM patient started on lenalidomide-based induction
A 56-year-old Caucasian male is diagnosed with high-risk MM (t[4;14] on FISH) and about to start induction treatment with DVRd (daratumumab, bortezomib, lenalidomide, and low-dose dexamethasone). He is transplant eligible. His ECOG status is 1. The patient is fully ambulatory with no prior history of DVT and no other high-risk features for thrombosis. What are the most important aspects to consider when choosing thromboprophylaxis for this patient?
Risk stratification and choice of VTE prophylaxis for low-risk MM patients
When treating a newly diagnosed MM patient with a lenalidomide-containing regimen that has no high-risk feature for DVT, thromboprophylaxis is recommended by both the IMWG and the EMN [37, 38]. In general, it is important to balance the risk of thrombosis with the risk of bleeding and consider any absolute contraindications such as thrombocytopenia (platelets < 20 × 109), active bleeding, or congenital bleeding disorders (e.g., hemophilia). In this case, comprehensive risk stratification should be performed using the currently available risk-stratification models as well as additional patient-specific, disease-specific, and treatment-specific risk factors that are known to impart a greater risk of VTE. According to the IMWG and EMN Guidelines, the options for thromboprophylaxis in MM include aspirin (81–325 mg), low-molecular-weight heparin, and full-dose therapeutic warfarin [37, 38, 40, 41]. The choice of therapy may depend on the patient’s individual risk factors and the potential for drug interactions with other medications. A brief summary of the thromboprophylaxis regimen commonly used in MM is provided in Table 1.
Several studies have investigated the efficacy of aspirin, low-molecular-weight heparin (LMWH), and warfarin in preventing VTEs in patients with newly diagnosed multiple myeloma (NDMM). A randomized controlled trial (RCT) study compared aspirin (100 mg/day) with LMWH (enoxaparin 40 mg/day) in NDMM patients treated with lenalidomide plus dexamethasone. VTE incidence was reported to be 2.3% in the aspirin cohort and 1.2% in the LMWH cohort, demonstrating no statistically significant difference between the two groups. Additionally, in both aspirin and LMWH cohorts, no major or minor bleeding complications were reported, with only 1 gastrointestinal minor bleeding observed in the LMWH cohort, which was completely and spontaneously resolved [9]. Another phase III randomized study investigated the role of aspirin (100 mg/day), LMWH (enoxaparin 40 mg/day), and warfarin (fixed dose of 1.25 mg/day) in patients with NDMM treated with a thalidomide-based regimen and again found no difference in the incidence of symptomatic VTE (6.4% in the aspirin group, 8.2% in the warfarin group, and 5.0% in the LMWH group) [10]. During the first six months, three patients (1.4%) experienced significant bleeding while taking aspirin, whereas none of the patients on warfarin or LMWH had such a major event. Minor bleeding was observed in six patients (2.7%) from the aspirin group, one patient (0.5%) from the warfarin group, and three patients (1.4%) from the LMWH group. In both trials, the rate of VTEs was lower (< 10%) than the reported incidences in real-world studies, which was likely driven by the exclusion of high-risk patients (e.g., prior VTE, immobilization leading to poor performance status). The phase 3 Myeloma XI study is the largest randomized trial reporting data on the utilization of IMiDs and corticosteroids in NDMM patients and reports thrombosis outcomes data in transplant-eligible and transplant-ineligible patients after the adoption of thrombosis prevention guidelines. In Myeloma XI, patients were stratified based on VTE risk and assigned to receive aspirin or LMWH for at least three months. Despite risk-based thromboprophylaxis, breakthrough VTE events occurred in a significant proportion of patients (11.8%), especially in the first six months of treatment [14]. Similarly, the rate of VTE in the Phase II randomized GRIFFIN trial was substantial, with VTEs (grades 2–4, none grade 5) reported in 10 (10.1%) patients in D-VRd arm and 16 (15.7%) patients in VRd arm. These results indicate a substantial VTE risk despite the use of IMWG-recommended anti-thrombotic prophylaxis [15].
In terms of risk stratification, there are three scores most commonly used for newly diagnosed MM patients: the SAVED model, the IMPEDE-VTE model, and the PRISM score [12, 42, 43]. All three scores were derived from a retrospective review of large datasets and multivariable analysis in NDMM patients. The SAVED model takes into account the patient’s age, race, history of prior thrombosis, surgery within 90 days, and the dose of dexamethasone received. The IMPEDE-VTE model includes various factors, including BMI, administration of immunomodulator drugs or erythropoiesis-stimulating agents, doxorubicin, dose-dependent dexamethasone, race, prior history of VTE, insertion of a central venous catheter, recent bone fractures, and the utilization of LMWH, warfarin, or aspirin. The PRISM score adopted a 5-variable system that included the following: prior VTE, prior surgery, immunomodulatory drug use, abnormal metaphase cytogenetics, and race (Table 2). A recent external validation of the PRISM score in 213 consecutive patients demonstrated an area under the curve (AUC) of 0.76 for predicting VTEs during the treatment course. The score was especially useful for high-risk patients, with 77% developing a VTE during the study course [44]. However, it is important to note that these scores have been developed in heterogeneous populations, with significant heterogeneity in the treatments received and the prophylactic measures taken in each cohort (e.g., the SAVED model only included patients treated with IMiD-based regimens). Notably, risk stratification based on FISH cytogenetics and ISS stage did not seem to correlate with the risk of thrombosis in NDMM [12, 13].
The patient in this vignette is classified as low-risk (1) according to the SAVED model, as they are treated with low-dose dexamethasone [45]. However, the patient is intermediate-risk (scoring 6 and 2, respectively) according to the IMPEDE-VTE model (which considers the use of low-dose dexamethasone and an IMiD) and the PRISM score (use of an IMiD). The corresponding 6-month risk for developing a VTE event would be 7% according to the SAVED model and 8.3% according to the IMPEDE-VTE model. For PRISM, the 12-month cumulative risk would be 10.8%. In terms of induction therapy, the addition of daratumumab to any MM regimen does not seem to increase the risk for VTEs, as shown in a recent analysis of the MAIA and GRIFFIN trials [46, 47]. We thus recommend aspirin (81–325 mg) alone as thromboprophylaxis in this patient, given that he is at a low to intermediate risk of VTE. When it comes to the duration of thromboprophylaxis, the patient should remain on their initial dosage for as long as they are on induction therapy. For the peri-transplant period, a study of 493 patients found a 3.5% incidence of symptomatic VTEs from mobilization until 30 days post-transplant, indicating a reduced incidence in the post-induction setting [48]. Since the risk of VTE decreases further during maintenance therapy [14], the omission of thromboprophylaxis could be considered at that point.
In summary, thromboprophylaxis in MM should be tailored to the individual patient and their risk factors. The choice of therapy should be made with careful consideration of the risk of thrombosis and bleeding, as well as potential drug interactions and contraindications. The use of risk stratification scores such as SAVED, IMPEDE-VTE, and PRISM can help guide the choice of thromboprophylaxis; however, clinical judgment remains important in determining the optimal thromboprophylaxis agent.
Case 2. Newly diagnosed MM patient, treated with KRd as induction: the role of DOACs
A 65-year-old African American woman was recently diagnosed with MM and is starting treatment with KRd (low-dose dexamethasone). The plan is to continue induction treatment for 8–12 cycles and transition to lenalidomide maintenance, with auto-transplant reserved for 1st relapse. She also had an arthroplasty for a hip fracture 2 months prior to diagnosis. Which is the best regimen to consider for this patient?
Choice of VTE prophylaxis for high-risk patients
Based on the information provided, the patient is considered high-risk for the IMPEDE-VTE model (IMiD use, recent fracture, surgery, dexamethasone), the SAVED model (surgery, dexamethasone), and the PRISM score (race, IMiD use, surgery), scoring 10, 3, and 8 respectively. According to the IMPEDE-VTE score, the risk of developing VTE within 6 months is estimated to be 15.2%, while the SAVED score predicts a risk of 11–12%. On the other hand, the PRISM model indicates that high-risk patients have a cumulative risk of 36.5% for developing VTE within 12 months. The patient is also receiving the PI carfilzomib, which also seems to increase the risk of thrombosis as shown in the phase 3 ENDURANCE trial comparing KRd vs. VRd in NDMM patients, which found increased grade 3–5 VTE rates for the KRd arm (5% vs. 2%, respectively) [34]. The increased risk for carfilzomib is also shown in other retrospective studies [13, 35]. In the absence of other characteristics (e.g., other drugs, renal failure), this patient should be considered for either LMWH, warfarin, or a DOAC for at least the first 6 months of therapy, when the risk of VTE is greatest [20].
The use of LMWH or warfarin, over aspirin, for high-risk patients can be supported by the results of a meta-analysis of 1,964 patients that showed an increased risk of VTEs in patients treated with aspirin, compared to LMWH (OR = 2.6) [49, 50]. Lower rates were also seen in the prospective MELISSE trial from France, with VTEs occurring in 7% of patients on aspirin, 3% on LMWH, and none on vitamin K antagonists [24]. Finally, a recent analysis of the IFM/DFCI 2009, where 90% of patients treated with heparin or analogs, found a cumulative rate of 4.8% in the first six months, which is lower than what is reported in the literature [13, 51]. The National Comprehensive Cancer Network recently added the option of fondaparinux (2.5 mg/day) or a DOAC as an alternative option for patients with an IMPEDE-VTE score > 3 or a SAVED score > 1 [52]. Two randomized clinical trials have established the efficacy of DOACs for thromboprophylaxis in ambulatory cancer patients and a high Khorana score (> 2, which includes primary cancer location, platelet, and WBC count, hemoglobin level), with both studies showing significantly reduced rates of VTEs compared to placebo treatment (6 vs. 8.8% for rivaroxaban vs. placebo, and 4.2 vs. 10.2% for apixaban vs. placebo, respectively) [25, 53, 54]. . Moreover, neither drug resulted in a statistically significant increase in the risk of major bleeding events during treatment, suggesting that DOACs are a safe alternative for LMWH. In the AVERT trial, a major bleeding event occurred in 2.1% of the apixaban group and 1.8% of the placebo group, whereas, in the CASSINI trial, only 2% of the rivaroxaban group and 1% of the placebo group had major bleedings. However, these trials included very few or no patients with MM [just 15 (2.6%) in the AVERT trial and unclear in the CASSINI trial]. Furthermore, the use of DOACs for thromboprophylaxis among patients with MM was explored in multiple single-arm studies [55]. The corresponding results suggest that DOACs may be a viable alternative to aspirin and LMWH for thromboprophylaxis in MM patients [56,57,58,59]. For example, a single institution retrospective review conducted by Man et al. on IMiD-treated patients found that the use of DOACs resulted in fewer bleeding events (none being major) compared to warfarin. Additionally, a phase 2 study explored the use of apixaban, for six months, in 104 patients with MM who received IMiD agents. Two VTEs and one major bleeding event (11 non-major) were recorded among those 104 patients on apixaban, with NDMM (N = 11) and R/R MM on IMiDs (N = 93). Finally, a retrospective study reported the outcomes of 305 NDMM patients, who received either aspirin or rivaroxaban for induction therapy (KRd or VRd). They found that patients treated with KRd plus aspirin had higher rates of VTEs compared to patients treated with VRd plus aspirin (16.1% vs. 4.8%). The VTE risk of KRd, however, was abrogated with the use of DOACs, and patients who received KRd plus rivaroxaban had identical VTE rates as VRd (4.8%) [35].
Therefore, considering the patient’s clinical scenario, a more intensive thromboprophylaxis approach is recommended than aspirin alone. Given the potential benefits of DOACs (effectiveness, ease of administration, and lack of monitoring requirement), it is recommended to use apixaban (2.5 mg x 2/day) or rivaroxaban (10 mg/day) as thromboprophylaxis in this patient with MM, receiving an induction regimen with carfilzomib combined with an IMiD. However, as the current evidence on the use of DOACs in MM patients is limited to small single-arm studies, there is a need for randomized controlled studies to definitively assess their efficacy and safety in this patient population.
Case 3. ΜΜ patient post-induction, consideration of maintenance
A 60-year-old Caucasian male is considering maintenance options after an autologous stem cell transplant for standard-risk MM with normal metaphase-cytogenetics. The physician’s choice is lenalidomide (10 mg/day) until progression. He has no prior history of VTE, and no surgery, with an ECOG of 0 and a BMI of 24. Should the patient be considered for thromboprophylaxis?
Role of VTE prophylaxis in the maintenance setting
A comprehensive risk stratification for this patient, including the three models (IMPEDE-VTE, PRISM, and SAVED), suggests a low risk for VTE at diagnosis. Furthermore, he presents no identifiable risk factors, such as recent surgery, fracture, or use of dexamethasone. However, these risk models are not applicable for patients on maintenance and thus should not be used to guide decisions for this patient. Due to the low risk of VTE in the maintenance setting, it remains unclear whether VTE prophylaxis is required during IMiD-based maintenance therapy. The consideration for low-dose aspirin is substantiated by studies that involved more than 1,000 patients and examined the use of lenalidomide maintenance after transplant. These studies reported VTE rates of up to 6% when prophylaxis was not used but less than 1% when a risk-adapted approach to prophylaxis was employed [60, 61]. Naturally, clinical circumstances, such as recent fractures or surgery, must always be considered when determining the appropriate thromboprophylaxis strategy.
A recent meta-analysis of trials with single-agent lenalidomide maintenance found only a 3.2% pooled incidence rate for VTEs, and a corresponding 0.0 [0.0–0.7] pooled incidence per 100 patient cycles [16]. These rates were the lowest among all lenalidomide-containing combinations across all studies and treatment phases. Moreover, while carfilzomib is associated with a greater VTE risk in the induction setting, the risk of VTE does not seem to increase with the addition of carfilzomib in the maintenance setting, as shown by the FORTE trial (carfilzomib-lenalidomide vs. lenalidomide maintenance), in which both treatment arms experienced 1 (1%) grade 3 VTE event in the observation period [62].
Considering the patient’s low-risk profile as per the IMPEDE, PRISM, and SAVED models at diagnosis and the low risk of VTE in the maintenance setting overall, either low-dose aspirin or no thromboprophylaxis can be considered reasonable.
Case 4. Relapsed/refractory MM (RRMM) patient with no DVT-specific risk factors
A 70-year-old African American male, post two lines of therapy, is currently relapsing and will start a new line of therapy. The next line includes a combination of daratumumab, bortezomib, and dexamethasone. The patient is fully ambulatory with no prior history of DVT and no other high-risk features for thrombosis, including no recent or prior surgeries. He is very active.
VTE prophylaxis in the relapsed/refractory setting and risk of thrombosis based on MM regimen
After utilizing the IMPEDE-VTE, PRISM, and SAVED models, as well as considering the patient information, a low risk for VTE has been indicated (IMPEDE-VTE, SAVED, and PRISM scores of 2, 1, and 1, respectively) at the time of diagnosis. However, it is important to note that these scores were created for NDMM patients, and the corresponding risks may not apply in the RR setting. When determining the need for thromboprophylaxis in RRMM, it is essential to take into account the most significant clinical factors as well as the specific treatment chosen.
For proteasome inhibitors, carfilzomib seems to be more thrombogenic than bortezomib in the relapsed setting, as shown in the phase 3 ENDEAVOR study comparing Kd vs. Vd (3.7% vs. 0.9% all grade VTE rates, respectively) [63]. The addition of carfilzomib in the ASPIRE study reported 6.6% DVT events in the KRd cohort and 3.9% in the lenalidomide and dexamethasone group [64]. For pomalidomide, studies have demonstrated that the incidence of VTE is similar in RRMM patients treated with pomalidomide plus low-dose dexamethasone compared to pomalidomide alone (2% vs. 3%) [65]. In this trial, all patients received prophylactic aspirin (81–100 mg/day) unless contraindicated. Low VTE rates are also seen with the lenalidomide and dexamethasone combination, with an estimated risk of 3.9% in RRMM patients [66]. The addition of daratumumab does not seem to increase the risk for DVT in IMiD-treated RRMM patients, as shown by the POLLUX and the APOLLO trials, with similar VTE rates between the daratumumab and control cohorts [66, 67]. The same is true for the other approved anti-CD-38 antibody (isatuximab), as shown in the phase 3 IKEMA trial (IKd vs. Kd), with similar VTE rates between the two groups (15% vs.16%).
In conclusion, while the risk of VTE remains relatively lower in RRMM compared to NDMM, a personalized approach to thromboprophylaxis should be taken into consideration by evaluating individual patient risk factors and the potential benefits of combination therapies (including IMiDs, PIs, and others). Clinical judgment is paramount in determining the appropriate treatment. If the combination regimen contains IMiD or carfilzomib, it is reasonable to use low-dose aspirin as a thromboprophylaxis regimen. For patients who had a prior history of VTE with these agents, DOACs should be strongly considered for thromboprophylaxis if rechallenging at relapse.
In summary, notwithstanding the progress made in VTE prophylaxis and management in MM, critical gaps persist. First, as our understanding of the factors associated with VTEs deepens, the development of more accurate prediction models will facilitate the identification of high-risk patients and thus allow for a personalized approach to VTE prevention. There is also a need for RCTs to examine DOACs’ efficacy and safety in high VTE-risk patients (e.g., ≥ 10%). Additionally, the advent of innovative T-cell-based therapies, such as CAR-T and bispecific antibodies, necessitates the prospective characterization of associated VTE risk profiles. Addressing these needs will promote the development of targeted and efficacious preventative measures, ultimately enhancing patient prognosis and overall well-being.
Data availability
No datasets were generated or analysed during the current study.
References
Rajkumar SV (2022) Multiple myeloma: 2022 update on diagnosis, risk stratification, and management. Am J Hematol 97(8):1086–1107
Binder M et al (2022) Mortality trends in multiple myeloma after the introduction of novel therapies in the United States. Leukemia 36(3):801–808
Chakraborty R, Majhail NS (2020) Treatment and disease-related complications in multiple myeloma: implications for survivorship. Am J Hematol 95(6):672–690
Fotiou D, Gavriatopoulou M, Terpos E (2020) Multiple myeloma and thrombosis: Prophylaxis and Risk Prediction Tools. Cancers (Basel), 12(1)
Kristinsson SY et al (2008) Deep vein thrombosis after monoclonal gammopathy of undetermined significance and multiple myeloma. Blood 112(9):3582–3586
Covut F, Sanfilippo KM (2022) Mitigating the risk of venous thromboembolism in patients with multiple myeloma receiving immunomodulatory-based therapy. Hematol Am Soc Hematol Educ Program 2022(1):363–367
Dimopoulos M et al (2007) Lenalidomide plus dexamethasone for relapsed or refractory multiple myeloma. N Engl J Med 357(21):2123–2132
De Stefano V et al (2022) Thrombosis in multiple myeloma: risk stratification, antithrombotic prophylaxis, and management of acute events. A consensus-based position paper from an ad hoc expert panel. Haematologica 107(11):2536–2547
Larocca A et al (2012) Aspirin or enoxaparin thromboprophylaxis for patients with newly diagnosed multiple myeloma treated with lenalidomide. Blood 119(4):933–939 quiz 1093
Palumbo A et al (2011) Aspirin, warfarin, or enoxaparin thromboprophylaxis in patients with multiple myeloma treated with thalidomide: a phase III, open-label, randomized trial. J Clin Oncol 29(8):986–993
Palumbo A et al (2008) Prevention of thalidomide- and lenalidomide-associated thrombosis in myeloma. Leukemia 22(2):414–423
Chakraborty R et al (2022) Abnormal metaphase cytogenetics predicts venous thromboembolism in myeloma: derivation and validation of the PRISM score. Blood 140(23):2443–2450
Charalampous C et al (2023) Thrombosis in multiple myeloma: risk estimation by induction regimen and association with overall survival. Am J Hematol 98(3):413–420
Bradbury CA et al (2020) Thrombosis in patients with myeloma treated in the myeloma IX and myeloma XI phase 3 randomized controlled trials. Blood 136(9):1091–1104
Sborov DW et al (2022) Daratumumab plus Lenalidomide, bortezomib and dexamethasone in newly diagnosed multiple myeloma: analysis of vascular thrombotic events in the GRIFFIN study. Br J Haematol 199(3):355–365
Chakraborty R et al (2020) Venous thromboembolism risk with contemporary lenalidomide-based regimens despite thromboprophylaxis in multiple myeloma: a systematic review and meta-analysis. Cancer 126(8):1640–1650
Winter MP, Schernthaner GH, Lang IM (2017) Chronic complications of venous thromboembolism. J Thromb Haemost 15(8):1531–1540
Khorana AA et al (2013) Health care costs associated with venous thromboembolism in selected high-risk ambulatory patients with solid tumors undergoing chemotherapy in the United States. Clinicoecon Outcomes Res 5:101–108
Rajkumar SV (2018) Value and cost of Myeloma Therapy. Am Soc Clin Oncol Educ Book 38:662–666
Kristinsson SY et al (2012) Thrombosis is associated with inferior survival in multiple myeloma. Haematologica 97(10):1603–1607
Schoen MW et al (2020) Venous thromboembolism in multiple myeloma is associated with increased mortality. Res Pract Thromb Haemost 4(7):1203–1210
Chakraborty R et al (2021) Arterial thromboembolism in multiple myeloma in the context of modern anti-myeloma therapy. Blood Cancer J 11(6):121
Huang H, Li H, Li D (2015) Effect of serum monoclonal protein concentration on haemostasis in patients with multiple myeloma. Blood Coagul Fibrinolysis 26(5):555–559
Leleu X et al (2013) MELISSE, a large multicentric observational study to determine risk factors of venous thromboembolism in patients with multiple myeloma treated with immunomodulatory drugs. Thromb Haemost 110(4):844–851
Khorana AA et al (2008) Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 111(10):4902–4907
Khan F et al (2021) Venous thromboembolism. Lancet 398(10294):64–77
Kwaan HC (2013) Hyperviscosity in plasma cell dyscrasias. Clin Hemorheol Microcirc 55(1):75–83
Cortelezzi A et al (2005) Incidence of thrombotic complications in patients with haematological malignancies with central venous catheters: a prospective multicentre study. Br J Haematol 129(6):811–817
Anaissie EJ et al (2012) Prophylactic recombinant erythropoietin therapy and thalidomide are predictors of venous thromboembolism in patients with multiple myeloma: limited effectiveness of thromboprophylaxis. Cancer 118(2):549–557
Zangari M et al (2004) Deep vein thrombosis in patients with multiple myeloma treated with thalidomide and chemotherapy: effects of prophylactic and therapeutic anticoagulation. Br J Haematol 126(5):715–721
Rajkumar SV et al (2010) Lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open-label randomised controlled trial. Lancet Oncol 11(1):29–37
Rosovsky R et al (2013) Endothelial stress products and coagulation markers in patients with multiple myeloma treated with lenalidomide plus dexamethasone: an observational study. Br J Haematol 160(3):351–358
Patel JN et al (2021) Thromboembolism incidence and risk factors in multiple myeloma after first exposure to Immunomodulatory Drug-based regimens. Clin Lymphoma Myeloma Leuk 21(3):188–198e2
Kumar SK et al (2020) Carfilzomib or bortezomib in combination with lenalidomide and dexamethasone for patients with newly diagnosed multiple myeloma without intention for immediate autologous stem-cell transplantation (ENDURANCE): a multicentre, open-label, phase 3, randomised, controlled trial. Lancet Oncol 21(10):1317–1330
Piedra K et al (2022) Comparison of venous thromboembolism incidence in newly diagnosed multiple myeloma patients receiving bortezomib, lenalidomide, dexamethasone (RVD) or carfilzomib, lenalidomide, dexamethasone (KRD) with aspirin or rivaroxaban thromboprophylaxis. Br J Haematol 196(1):105–109
Carrier M et al (2011) Rates of venous thromboembolism in multiple myeloma patients undergoing immunomodulatory therapy with thalidomide or lenalidomide: a systematic review and meta-analysis. J Thromb Haemost 9(4):653–663
Terpos E et al (2015) European Myeloma Network guidelines for the management of multiple myeloma-related complications. Haematologica 100(10):1254–1266
Palumbo A et al (2014) International Myeloma Working Group consensus statement for the management, treatment, and supportive care of patients with myeloma not eligible for standard autologous stem-cell transplantation. J Clin Oncol 32(6):587–600
Palumbo A et al (2006) Oral melphalan and prednisone chemotherapy plus thalidomide compared with melphalan and prednisone alone in elderly patients with multiple myeloma: randomised controlled trial. Lancet 367(9513):825–831
Weber D et al (2003) Thalidomide alone or with dexamethasone for previously untreated multiple myeloma. J Clin Oncol 21(1):16–19
Rajkumar SV et al (2005) Combination therapy with lenalidomide plus dexamethasone (Rev/Dex) for newly diagnosed myeloma. Blood 106(13):4050–4053
Sanfilippo KM et al (2019) Predicting venous thromboembolism in multiple myeloma: development and validation of the IMPEDE VTE score. Am J Hematol 94(11):1176–1184
Li A et al (2019) Derivation and validation of a risk Assessment Model for Immunomodulatory Drug-Associated thrombosis among patients with multiple myeloma. J Natl Compr Canc Netw 17(7):840–847
Sekar A et al (2023) External validation of PRISM score in multiple myeloma patients in a community setting: a retrospective cohort study. Blood 142(Supplement 1):4721–4721
Dima D et al (2023) External validation of the SAVED score for venous thromboembolism risk stratification in patients with multiple myeloma receiving immunomodulatory drugs. Br J Haematol 201(2):280–284
Voorhees PM et al (2023) Addition of daratumumab to lenalidomide, bortezomib, and dexamethasone for transplantation-eligible patients with newly diagnosed multiple myeloma (GRIFFIN): final analysis of an open-label, randomised, phase 2 trial. Lancet Haematol 10(10):e825–e837
Rosqvist S et al (2023) High rates of thrombotic events in newly diagnosed multiple myeloma patients enrolled on the Maia Trial. Blood 142(Supplement 1):4718–4718
Awada H et al (2023) Risk of venous thromboembolism in multiple myeloma patients during the Immediate Peri-autologous hematopoietic cell transplantation phase. Clin Appl Thromb Hemost 29:10760296231177678
Zoppellaro G et al (2018) Primary thromboembolic prevention in multiple myeloma patients: an exploratory meta-analysis on aspirin use. Semin Hematol 55(4):182–184
Al-Ani F et al (2016) Thromboprophylaxis in multiple myeloma patients treated with lenalidomide - A systematic review. Thromb Res 141:84–90
Chalayer E et al (2022) Prediction of venous thromboembolism in patients with multiple myeloma treated with lenalidomide, bortezomib, dexamethasone, and transplantation: lessons from the substudy of IFM/DFCI 2009 cohort. J Thromb Haemost 20(8):1859–1867
Callander NS et al (2022) NCCN Guidelines® insights: multiple myeloma, Version 3.2022. J Natl Compr Canc Netw 20(1):8–19
Khorana AA et al (2019) Rivaroxaban for Thromboprophylaxis in High-Risk Ambulatory patients with Cancer. N Engl J Med 380(8):720–728
Carrier M et al (2019) Apixaban to prevent venous thromboembolism in patients with Cancer. N Engl J Med 380(8):711–719
Cornell RF et al (2020) Primary prevention of venous thromboembolism with apixaban for multiple myeloma patients receiving immunomodulatory agents. Br J Haematol 190(4):555–561
Pegourie B et al (2019) Apixaban for the prevention of thromboembolism in immunomodulatory-treated myeloma patients: Myelaxat, a phase 2 pilot study. Am J Hematol 94(6):635–640
Storrar NPF et al (2019) Safety and efficacy of apixaban for routine thromboprophylaxis in myeloma patients treated with thalidomide- and lenalidomide-containing regimens. Br J Haematol 185(1):142–144
Cornell RF et al (2019) Apixaban for Primary Prevention of venous thromboembolism in patients with multiple myeloma receiving Immunomodulatory Therapy. Front Oncol 9:45
Man L et al (2017) Use of direct oral anticoagulants in patients on immunomodulatory agents. J Thromb Thrombolysis 44(3):298–302
Attal M et al (2012) Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. N Engl J Med 366(19):1782–1791
McCarthy PL et al (2012) Lenalidomide after stem-cell transplantation for multiple myeloma. N Engl J Med 366(19):1770–1781
Gay F et al (2021) Carfilzomib with cyclophosphamide and dexamethasone or lenalidomide and dexamethasone plus autologous transplantation or carfilzomib plus lenalidomide and dexamethasone, followed by maintenance with carfilzomib plus lenalidomide or lenalidomide alone for patients with newly diagnosed multiple myeloma (FORTE): a randomised, open-label, phase 2 trial. Lancet Oncol 22(12):1705–1720
Dimopoulos MA et al (2016) Carfilzomib and dexamethasone versus bortezomib and dexamethasone for patients with relapsed or refractory multiple myeloma (ENDEAVOR): a randomised, phase 3, open-label, multicentre study. Lancet Oncol 17(1):27–38
Stewart AK et al (2015) Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med 372(2):142–152
Richardson PG et al (2014) Pomalidomide alone or in combination with low-dose dexamethasone in relapsed and refractory multiple myeloma: a randomized phase 2 study. Blood 123(12):1826–1832
Dimopoulos MA et al (2016) Daratumumab, Lenalidomide, and Dexamethasone for multiple myeloma. N Engl J Med 375(14):1319–1331
Dimopoulos MA et al (2021) Daratumumab plus Pomalidomide and dexamethasone versus pomalidomide and dexamethasone alone in previously treated multiple myeloma (APOLLO): an open-label, randomised, phase 3 trial. Lancet Oncol 22(6):801–812
Gray E, Mulloy B, Barrowcliffe TW (2008) Heparin and low-molecular-weight heparin. Thromb Haemost 99(5):807–818
Gulati S, Eckman MH (2023) Anticoagulant therapy for Cancer-Associated thrombosis: a cost-effectiveness analysis. Ann Intern Med 176(1):1–9
Funding
None.
Author information
Authors and Affiliations
Contributions
C.C. and R.C. conceived the study. C.C. and D.S. wrote the first draft of the manuscript. S.K. and R.C. provided critical feedback and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Charalampous, C., Shah, D., Kumar, S. et al. Thromboprophylaxis in multiple myeloma: a case-based review with practical guidelines. Ann Hematol (2024). https://doi.org/10.1007/s00277-024-05733-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00277-024-05733-9