Summary
The study analysed the clinical characteristics, treatment approaches, and survival outcomes of 97 consecutive patients with orbital lymphoma (OL) over a 25-year period at. The median age of the patients was 57.6 years, and 59.8% (n = 58) were male. Marginal zone lymphoma constitutes the most prevalent subtype, accounting for 67% of cases, whereas other common subtypes include diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, Burkitt lymphoma, and T-cell lymphomas. Unilateral involvement was observed in the majority of cases (72.3%). Common clinical presentations included mass (30.9%), swelling (26.8%), and epiphora (11.3%). Of the patients, 7.2% received rituximab alone, 14.4% received radiotherapy alone, 48.5% received chemotherapy, 27.8% received radiotherapy plus rituximab, 22.7% received radiotherapy plus chemotherapy, and 5.2% underwent surgery as the first-line treatment. During a median follow-up of 4.3 years, 15.5% of patients experienced relapse or disease progression. The 5-year and 10-year progression-free survival rates were 84.1% and 79.1%, respectively. This study contributes to our understanding of OLs and provides a foundation for further investigations in this field. Male gender, presence of B symptoms, advanced stage, secondary orbital lymphoma, aggressive histological subtype, and elevated serum lactate dehydrogenase levels were associated with poorer (either inferior or worse) progression-free survival.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Orbital lymphomas (OLs) represent a subset of non-Hodgkin lymphomas (NHLs) that primarily affect the orbital tissues, including the eyelids, extraocular muscles, conjunctiva, lacrimal glands, or soft tissues of the orbital adnexa [1, 2]. OL is considered a distinct entity within the spectrum of lymphoid neoplasms due to its unique anatomical localization and clinical behaviour. OL accounts for more than half of all orbital tumors and constitutes approximately 1–2% of all NHL cases [3]. The majority of OLs originates from B cells, and extranodal marginal zone lymphoma (MZL) is the most prevalent histological subtype. Other subtypes, including follicular lymphoma (FL), diffuse large B-cell lymphoma (DLBCL), and mantle-cell lymphoma (MCL), are less common but still contribute to the overall disease spectrum [1, 4]. The incidence of OL increases in the seventh decade of life [5, 6]. Although most cases are unilateral, approximately 7–24% of patients develop bilateral OL [1, 6].
OL may present with diverse signs including proptosis, palpable periocular mass or painless eyelid swelling [7]. Advanced age, clinical stage, histological subtype, lymph node involvement, and serum lactate dehydrogenase levels have all been reported as prognostic indicators in OL [8]. However, the prognosis of OL is especially influenced by the histological subtype and clinical stage. Low-grade lymphomas account for 84%, while high-grade lymphomas account for only 16% of all OL cases [9]. Furthermore, emerging evidence suggests a potential association between OL and certain microorganisms, most notably Chlamydia psittaci [10, 11]. Studies have implicated infectious agents in the development of OL, highlighting the complex interplay between infection and lymphomagenesis in the orbital region.
Despite the clinical significance of OL, research focusing on it is scarce. Therefore, the present study aimed to comprehensively characterize the histological subtypes of OL, determine the clinical stages at diagnosis, evaluate the treatment approaches, and assess the impact of these factors on survival outcomes in a cohort of Turkish patients. By providing insights into the unique characteristics and management of OLs in the Turkish population, this study aims to contribute to the existing knowledge and guide future research efforts in this field.
Methods
Study design and patient selection
This retrospective study aimed to analyse the clinical characteristics, treatment approaches, and survival outcomes of patients diagnosed with OL. The study was conducted at Hacettepe University Cancer Institute in collaboration with Hacettepe School of Medicine Department of Ophthalmology, including a total of 97 consecutive patients diagnosed with OL between January 2000 and May 2023. The study protocol was approved by the institutional review board of Hacettepe University, and written informed consent was obtained from all patients or their legal representatives.
Data collection
A comprehensive review of electronic medical records, pathology reports, and imaging studies was performed to collect relevant patient data. Demographic characteristics such as age and sex, relevant medical history, clinical presentation, symptom duration, lesion localization, and Eastern Cooperative Oncology Group performance status (ECOG-PS) were carefully documented. Imaging studies and laboratory tests, were reviewed to confirm the diagnosis of orbital lymphoma. Histological specimens, including biopsy or surgical resection samples, were evaluated by experienced pathologists to confirm the diagnosis of OL and determine the specific histological subtype according to the World Health Organization (WHO) classification system. Furthermore, the diagnosis was established in all patients through biopsy.
Clinical staging and treatment approaches
Clinical staging was determined based on a combination of imaging studies, including computed tomography (CT), magnetic resonance imaging (MRI), and fluorine-18 labeled fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) whenever available. Ann Arbor classification was used for staging. By definition, "primary" orbital lymphomas are stage IE since primary lymphomas are thought to be confined to the orbit. In "secondary" orbital lymphomas, on the other hand, where systemic illness may be present concurrently or prior, the orbit is the site of secondary extranodal involvement [3]. Treatment approaches were individualized based on the histological subtype, clinical stage, and patient-specific factors. Treatment modalities included systemic chemotherapy, radiotherapy, immunotherapy, and surgical excision. The choice and sequence of treatments were determined by a multidisciplinary team of medical oncologists, radiation oncologists, and ophthalmologists.
Follow-up and outcome measures
Patients were followed up at regular intervals after the completion of primary treatment. The duration of follow-up varied among patients depending on their treatment response and disease progression. The primary outcome measure was progression-free survival (PFS) which was defined as radiological evidence of disease recurrence or progression. The follow-up data were collected from electronic medical records, outpatient visits, and telephone interviews.
Data analysis
Statistical analyses were performed using IBM® SPSS software version 28. Descriptive statistics were presented as frequency (percent), mean ± SD, or median (min-max). Continuous variables were examined by visual and analytical methods to determine the normal distribution and analyzed with the Mann-Whitney U test. Survival estimates were calculated with the Kaplan-Meier method. The univariate and multivariate Cox regression analyses were used to identify the independent effects on PFS. An overall type-1 error level was used to infer statistical significance.
Ethical considerations
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. The study protocol was approved by the institutional review board, and patient confidentiality was strictly maintained. All patient data were de-identified and analyzed anonymously to ensure data privacy and confidentiality.
Results
Baseline characteristics
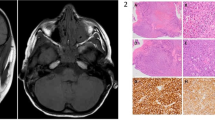
A total of 97 patients (59.8% male) were included in the study. The mean age at diagnosis was 57.6 ± 15.7 years. Forty-two (43.3%) patients had comorbid diseases, the most common of which was hypertension (26.8%). The most common local symptom or sign was mass (30 patients, 30.9%), while the others were swelling (26 patients, 26.8%), epiphora (11 patients, 11.3%), proptosis (9 patients, 9.3%), ptosis (7 patients, 7.2%), blindness (4 patients, 4.1%), diplopia (4 patients, 4.1%), limited ocular motility (3 patients, 3.1%), and paraxial globe displacement (3 patients, 3.1%) respectively. B symptoms, such as fever, weight loss, or night sweats, were present in 14 (14.4%) patients. The median time from symptom onset to diagnosis was 4 (0.5–180) months. While this time was 4 (0.5–180) months in MZL patients, it was 3 (1–14) months in non-MZL group (p = 0.006). ECOG-PS was 0, 1, and 2 in 80 (82.5%), 15 (15.5%), and 2 (2.1%) patients, respectively. The majority of cases presented with unilateral involvement (93 patients, 72.3%), while 4 patients (16.9%) had bilateral involvement. The tumor was localized in the orbit in 57 (58.8%) patients, in the lacrimal gland in 28 (28.9%) patients, and in the eyelids in 12 (12.4%) patients. Based on the Ann Arbor staging system, 68 (70.1%) patients were classified as stage IE, 10 (10.3%) patients as stage IIE, 5 (5.2%) patients as stage IIIE, and 14 (14.4%) patients as stage IV. The majority of cases presented with primary orbital lymphoma (77 patients, 79.4%), while 20 (20.6%) patients had secondary OL. Histopathologic subtypes of the OL were as follows: 65 (67%) patients had MZL, 13 (13.4%) patients had FL, 13 (13.4%) patients had DLBCL, 4 (4.1%) patients had MCL, and 2 (2.1%) patients had T/NK-cell lymphoma (Table 1, Fig. 1). There was no significant difference between histological subtypes according to tumor localization (p = 0.479, Fig. 2).
The median serum lactate dehydrogenase (LDH) level was 221 (115–1586) U/l and it was higher than normal in 36 (37.1%) patients. Laboratory examination results are detailed in Table 2. First-line treatment strategies employed in the study cohort included rituximab alone (7 patients, 7.2%), radiotherapy alone (14 patients, 14.4%), chemotherapy (47 patients, 48.5%), radiotherapy plus rituximab (27 patients, 27.8%), radiotherapy plus chemotherapy (22 patients, 22.7%), and surgical excision (5 patients, 5.2%) (Table 3).
Treatment response
Complete response (CR) was documented in 72 (74.2%) patients, 17 (17.5%) patients showed a partial response (PR), 6 (6.2%) patients had stable disease (SD), and 2 (2.1%) patients experienced progressive disease (PD). The objective response rate (CR + PR) was 91.7%, and the disease control rate (CR + PR + SD) was 97.9% (Table 4). Responses by first-line treatment types are detailed and visualized in Figs. 3, 4 and 5.
Images of pre (left) and post-treatment (right) physical examination findings. a) Proptosis due to marginal zone lymphoma in the left eye and response after 4 doses of rituximab. b) Follicular lymphoma mass in the right eye and response to 4 doses of R-CHOP treatment. c) Ptosis due to marginal zone lymphoma in the right eye and response to 2 doses of rituximab
Images of pre (left) and post-treatment (right) radiological findings. a) Marginal zone lymphoma involvement in the right eye and response after 4 doses of Rituximab. b) Diffuse large B-cell lymphoma involvement in the left eye and response after 4 doses of R-CVP therapy. c) Secondary follicular lymphoma involvement behind the right eye and response with 4 doses of R-CVP
Survival outcomes
During a median follow-up of 4.3 (0.2–21.5) years, 15 (15.5%) patients experienced relapse or progression. Among these, 8 (53.3%) patients had MZL, 3 (20%) patients had DLBCL, 3 (20%) patients had MCL, and 1 (6.7%) had T/NK cell lymphoma. Five of the patients with recurrent MZL received rituximab re-treatment, while three patients received a rituximab and radiotherapy combination. One of the 3 relapsed DLBCL patients underwent enucleation, while the other two patients had systemic involvement and one of them died. All MCL and T/NK cell lymphoma cases had widespread disease and received combined chemotherapy along with radiotherapy.
The median PFS estimate could not be reached in the Kaplan-Meier analysis. The 5-year and 10-year PFS rates were 84.1% (95%CI: 76.1–92.1) and 79.1% (95%CI: 68.9–89.3), respectively (Fig. 6). Factors affecting PFS were analysed with univariate and multivariate analyses. In univariate analyses, age at diagnosis (> vs ≤ 60 years, p = 0.658), ECOG-PS (≥ 1 vs. 0, p = 0.713), bilateral involvement (p = 0.84), and orbital localization (p = 0.646) were not associated with PFS; whereas male gender (HR: 11.05, p = 0.02), presence of B symptoms (HR: 8.623, p < 0.001), stage IV disease (HR: 3.375, p = 0.027), secondary OL (HR: 4.875, p = 0.002), aggressive histological subtype (HR: 5.062, p = 0.002), and high LDH (< vs. > 1 × normal, HR: 3.625, p = 0.029) significantly affected PFS. Multivariate analysis revealed that male gender (HR: 12.632, p = 0.017) and presence of B symptoms (HR: 6.34, p = 0.031) were independent predictors of PFS (Table 5, Figs. 7 and 8).
Discussion
Our study provides a comprehensive analysis of OLs in a Turkish cohort. The study highlighted the long-term clinical outcomes in this specific subset of patients. The analysis included 97 consecutive patients diagnosed with OL, with MZL being the most prevalent histological subtype. Common symptoms observed were a visible and/or palpable mass, eyelid swelling, and proptosis. The mean age of patients was 57.6 ± 15.7 years, and a slight male predominance was noted. These findings contribute to our understanding of the demographic and clinical characteristics of OL. The study identified male gender and presence of B symptoms as poor prognostic factors for PFS. The findings provide important insights into the clinical characteristics, histological subtypes, treatment modalities, and outcomes of OL in a Turkish cohort. Understanding prognostic factors helps in predicting patient outcomes and tailoring treatment strategies.
Min et al., in 2022, conducted a single-center study involving treatment-naïve patients with orbital adnexal mucosa-associated lymphoid tissue (MALT) lymphoma [12]. Similar to our cohort, they identified male gender and the presence of B symptoms as poor prognostic factors for PFS [12]. In Savino's study, OL patients with the DLBCL subtype had a significantly higher risk of relapse, as indicated by an odds ratio of 7.7 (95% CI: 1.8–32.3) [13]. Similarly, patients treated with chemotherapy had a higher likelihood of relapse, with an odds ratio of 14.9 (95% CI: 2.6–83.7) [13]. Another study showed that patients treated with chemotherapy alone experienced an inferior PFS compared to those who received combined therapies (p = 0.034) [4]. These factors provide valuable information in predicting response to treatment and guiding personalized management.
As evident from our study, due to the indolent nature of the MZL subtype and the delayed diagnosis over several years, patients may remain under observation without receiving a definite diagnosis if not evaluated by an experienced ophthalmologist. Therefore, patients with ocular pathological findings without a confirmed diagnosis must be evaluated by ophthalmologists experienced in orbital lymphoma and confirmed through biopsy. Additionally, MZL and FL subtypes present with indolent courses and fewer systemic manifestations, leading these patients to primarily seek care from ophthalmologists. Conversely, aggressive lymphomas such as DLBCL, T-NK cell lymphoma, Burkitt lymphoma, or secondary lymphomas are more likely to be referred to hematologist-oncologists rather than ophthalmologists initially. The course of the disease, the specific pathological subtype, and the evaluation by an experienced center can significantly impact the time to diagnosis and treatment for these patients.
Treatment approaches for OL vary depending on factors such as histological subtype, disease stage, and patient-specific considerations. Olsen et al., in 2019, conducted an international multicenter retrospective study to assess different treatment modalities and their outcomes [1]. The study emphasized the significance of histological subtype in determining treatment response and overall survival. Treatment modalities employed in OL management include rituximab alone, radiotherapy alone, and various chemotherapy regimens. The overall response rate reported across these studies was 91.7%. Furthermore, the use of radiotherapy as a primary treatment modality was explored in a systematic review by Oktariana et al. in 2022, further demonstrating its efficacy in managing OL [14].
Before the discovery of rituximab, radiotherapy was more commonly used; however, it is known to be associated with ocular side effects, such as radiation retinopathy, optic neuropathy, and neovascular glaucoma [15, 16]. Since 2005, at our center, rituximab therapy has become a preferred treatment method due to its early response in MZL patients and high rates of complete response, along with being less toxic compared to radiotherapy. When patients are appropriately evaluated and monitored for infusion reactions and hepatitis B reactivation, rituximab is considered a more favorable agent in terms of side effects and response rates, especially in MZL patients compared to radiotherapy. Nevertheless, considering that orbital lymphoma is a rare tumor, we present an appropriate treatment algorithm for approaching these patients in line with our center's practices and the approaches of other centers in the literature (Algorithm 1).
Approach to orbital lymphoma. CNS: central nervous system, DLBCL: diffuse large B-cell lymphoma, FL: follicular lymphoma, MZL: marginal zone lymphoma, MCL: mantle cell lymphoma, RT: radiotherapy. *For the majority of patients, rituximab monotherapy alone is adequate. **Bulky disease, visual disturbances, and the necessity for a rapid treatment response are considered. *** If the patient is frail and elderly (over 80 years of age) or if there are any contraindications to rituximab therapy. ****If the patient is asymptomatic, has no cosmetic concerns, or does not actively seek treatment
However, our study has several limitations. Firstly, it was conducted in a single-center setting, which may limit the generalizability of our findings to other populations. Secondly, the retrospective nature of the study introduces the possibility of incomplete data. Thirdly, the sample size of our study was relatively small, which may impact the statistical power and precision of our results. Lastly, our study did not evaluate the cost-effectiveness or long-term side effects of different treatment modalities. Future research should address these limitations to provide more comprehensive and robust evidence in the field of orbital lymphoma management. Despite these limitations, our study contributes valuable insights into the understanding of OL and lays the foundation for future investigations in this field.
Conclusions
In conclusion, this study provides a comprehensive analysis of OL in a Turkish cohort, focusing on clinical characteristics, histological subtypes, treatment modalities, and prognostic factors. The findings contribute to our understanding of this rare lymphoma subtype and can guide clinicians in making informed decisions regarding diagnosis, treatment selection, and prognostic assessment. Further research is warranted to validate these findings and advance our knowledge of orbital lymphoma.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Olsen TG, Holm F, Mikkelsen LH, Rasmussen PK, Coupland SE, Esmaeli B, Finger PT, Graue GF, Grossniklaus HE, Honavar SG, Khong JJ, McKelvie PA, Mulay K, Sjö LD, Vemuganti GK, Thuro BA, Heegaard S (2019) Orbital lymphoma-an international multicenter retrospective study. Am J Ophthalmol 199:44–57
Hsu CR, Chen YY, Yao M, Wei YH, Hsieh YT, Liao SL (2021) Orbital and ocular adnexal lymphoma: a review of epidemiology and prognostic factors in Taiwan. Eye 35(7):1946–1953 (Lond)
Olsen TG, Heegaard S (2019) Orbital lymphoma. Surv Ophthalmol 64(1):45–66
Kalicińska E, Giza A, Zaucha JM, Giebel S, Zimowska-Curyło D, Andrasiak I, Spychałowicz W, Wojnar J, Balcerzak A, Romejko-Jarosińska J, Paszkiewicz-Kozik E, Knopińska-Posłuszny W, Rybka J, Jabłonowska P, Wróbel T (2023) A survey across orbital lymphoma in Poland: Multicenter retrospective study of polish lymphoma research group (PLRG). Cancer Med 12(3):3036–3045
Sjö LD (2009) Ophthalmic lymphoma: epidemiology and pathogenesis. Acta Ophthalmol 87(Thesis 1):1–20
Svendsen FH, Rasmussen PK, Coupland SE, Esmaeli B, Finger PT, Graue GF, Grossniklaus HE, Honavar SG, Khong JJ, McKelvie PA, Mulay K, Ralfkiaer E, Sjö LD, Vemuganti GK, Thuro BA, Curtin J, Heegaard S (2017) Lymphoma of the eyelid - an international multicenter retrospective study. Am J Ophthalmol 177:58–68
Tranfa F, Di Matteo G, Strianese D, Forte R, Bonavolontà G (2001) Primary orbital lymphoma. Orbit 20(2):119–124
Wierda WG, Byrd JC, Abramson JS, Bilgrami SF, Bociek G, Brander D, Brown J, Chanan-Khan AA, Chavez JC, Coutre SE, Davis RS, Fletcher CD, Hill B, Kahl BS, Kamdar M, Kaplan LD, Khan N, Kipps TJ, Ma S, Malek S, Mato A, Mosse C, Neppalli VT, Shadman M, Siddiqi T, Stephens D, Wagner N, Dwyer MA, Sundar H (2019) NCCN Guidelines Insights: Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma, Version 2.2019. J Natl Compr Canc Netw 17(1):12–20
Bessell EM, Henk JM, Wright JE, Whitelocke RA (1988) Orbital and conjunctival lymphoma treatment and prognosis. Radiother Oncol 13(4):237–244
Collina F, De Chiara A, De Renzo A, De Rosa G, Botti G, Franco R (2012) Chlamydia psittaci in ocular adnexa MALT lymphoma: a possible role in lymphomagenesis and a different geographical distribution. Infect Agent Cancer 7:8
Chanudet E, Zhou Y, Bacon CM, Wotherspoon AC, Müller-Hermelink HK, Adam P, Dong HY, Jong D, Li Y, Wei R, Gong X, Wu Q, Ranaldi R, Goteri G, Pileri SA, Ye H, Hamoudi RA, Liu H, Radford J, Du MQ (2006) Chlamydia psittaci is variably associated with ocular adnexal MALT lymphoma in different geographical regions. J Pathol 209(3):344–351
Min GJ, Kim SE, Kim TY, Jeon YW, Hyun OJ, Choi BO, Park G, Yang SW, Cho SG (2022) Long-Term Clinical Outcomes in Treatment-Naïve Patients With Orbital Adnexal mucosa-associated lymphoid tissue lymphoma: A Single-center study. Front Oncol 12:769530
Savino G, Midena G, Blasi MA, Battendieri R, Grimaldi G, Maceroni M, Tranfa F, Napolitano P, Lanni V, Iuliano A (2020) Orbital and eyelid B-cell lymphoma: a multicenter retrospective study. Cancers (Basel) 12(9):2538.
Oktariana TP, Andriana A, Nugroho RS (2022) The outcome of radiation therapy as a primary treatment in orbital lymphoma: a systematic review. Rep Pract Oncol Radiother 27(4):724–733
Bischof M, Karagiozidis M, Krempien R, Treiber M, Neuhof D, Debus J, Zierhut D (2007) Radiotherapy for orbital lymphoma : outcome and late effects. Strahlenther Onkol 183(1):17–22
Alberti W (1997) Acute and late side effects of radiotherapy for ocular disease: an overview. Front Radiat Ther Oncol 30:281–286
Acknowledgements
The authors thank all faculty members of the Department of Radiation Oncology, Hacettepe University Medical School, for their continuous support in the evaluation and treatment of cases with orbital lymphomas.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
Conceptualization, A.A. and H.K.; Formal analysis, A.A.; R.I.; and S.A.; Funding acquisition, H.K.; Investigation, A.A., N.R., M.T., and I.K.; Methodology, A.A., R.I. and S.A.; Project administration, A.A.; Resources, S.A. and H.K.; Supervision, H.K., and I.B; Validation, I.K. and S.A.; Visualization, R.I.; Writing-original draft, A.A.; Writing-review & editing, R.I., S.A., H.K., and I.B. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to publish
Patients signed informed consent regarding publishing their data and photographs.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Akyildiz, A., Ismayilov, R., Rustamova, N. et al. Comprehensive analysis of orbital lymphoma in a Turkish cohort: clinical characteristics, histological subtypes, treatment modalities, prognostic factors, and implications for management. Ann Hematol 103, 905–915 (2024). https://doi.org/10.1007/s00277-023-05569-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05569-9