Abstract
Primary central nervous system lymphoma (PCNSL) is special extranodal malignant non-Hodgkin lymphomas. This study analyzed clinical features and prognostic factors of PCNSL and evaluated the difference of interleukin (IL) concentrations in cerebrospinal fluid (CSF) between PCNSL and systemic non-Hodgkin lymphoma (sNHL). Patients consecutive newly diagnosed with PCNSL were recruited, the demographic and clinicopathological data were retrospectively analyzed, and the potential prognostic factors for overall survival (OS) were identified with survival analysis. 27 patients with PCNSL and 21 patients with sNHL collected CSF IL-5, IL-6, and IL-10 concentrations at diagnosis. The difference in interleukin (IL) concentrations in two diseases was analyzed to evaluate the value of IL concentrations. A total of 64 patients with PCNSL were enrolled, the median age was 54.50 years (range 16–85 years); male: female ratio was 1.91. Headache was the most common complaint symptom involved in 42.19% (27/64) of patients. Diffuse large B-cell lymphoma (DLBCL) accounted for 89.06% (57/64) of patients; other uncommon types accounted for 3.13% (2/64). In prognostic analysis, multiple lesions and Ki67 ≥ 75% expression exhibited a worse prognosis(P = 0.041), and patients with autologous hematopoietic stem cell transplantation (auto-HSCT) treatment presented superior OS (P < 0.05). In multivariate analysis, BCL2 expression was revealed as an unfavorable prognostic marker, and auto-HSCT was revealed as a favorable prognostic marker. CSF IL-10 concentration in patients with PCNSL was significantly higher than sNHL (P = 0.000) and excluded other histopathology of NHL; IL-10 value was still significantly different between DLBCL of PCNSL and sDLBCL (P = 0.003). In ROC curve analysis, the cutoff value of IL-10 was 0.43 pg/mL for the diagnosis value of PCNSL, sensitivity was 96.3%, specificity was 66.67%, and AUC was 0.84 (0.71–0.96). Although IL-6 concentration did not differ in the two groups, IL-10/IL-6 ratio was meaningful, with a cutoff value of 0.21, sensitivity of 81.48%, specificity of 80.95%, and AUC of 0.83 (0.71–0.95). This study highlights the characteristics of patients with PCNSL, potential prognostic makers also have been explained. CSF interleukin (IL) concentrations revealed IL-10 levels, and IL-10/IL-6 ratio may represent a useful biomarker in the differential diagnosis of PCNSL and sNHL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system lymphoma (PCNSL) is special extranodal malignant non-Hodgkin lymphomas; more than 90% of the subtype is diffuse large B-cell lymphoma (DLBCL) [1]; other types reported include Burkitt lymphoma, low-grade lymphoma, T-cell lymphoma (peripheral T-cell lymphoma and anaplastic large T-cell lymphoma), and NK/T cell lymphoma [2].
Epidemiological studies revealed that PCNSL accounted for 4%–6% of extranodal lymphomas, 1% of lymphomas, and approximately 4% of central nervous system tumors (CNST) [3]. Research from Sweden and Australia showed the overall incidence of PCNSL was 0.26–0.43/10000 and increased at a rate of 4%–6.8% per year over the past 10 years [4, 5].
The definitive diagnosis of PCNSL depends on histopathology; the common tissue sample acquisitions are the stereotaxic biopsy, and surgical incisional biopsy, aggressive surgical resection has been discouraged [6]. In addition, magnetic resonance imaging (MRI) provides better visualization of soft tissue to identify lesions and is considered to be more helpful than computed tomography (CT) scan and FDG-positron emission tomography-computed tomography(PET/CT) scan [7]. In recent years, “liquid biopsy” gets researcher’s attention, cell-free DNA fragments (cfDNA) in blood or cerebrospinal fluid (CSF) provide exclusively of tumoral origin and could yield useful results, but the cfDNA concentrations are varied in different lymphoma subtypes, so it is difficult to obtain accordent result [8, 9]. Other CSF examinations may help to establish the diagnosis; the routine tests include protein levels, cytology, and flow cytometry, but with low sensitivities of 13.3–23.3% [10]. Other new biomarkers include interleukin (IL) concentrations, CXCL13, MYD88, and IgH gene rearrangement, the approaches provide higher sensitivities of over 50%, and the microRNAs even provide a diagnostic accuracy of over 90% [11].
Most pathological types of PCNSL are highly aggressive; due to the obstruction of the blood–brain barrier (BBB), many chemotherapy regimens have a poor effect on PCNSL [2]. Therefore, the clinical outcome of PCNSL patients is less than expected, and the 5-year overall survival (OS) rate is just about 30% [1, 2]. Against this background, we designed a retrospective analysis of the clinical and pathological features of patients with PCNSL in our center. The aim is to gain further understanding of PCNSL and potential prognostic factors. In addition, CSF interleukin (IL) concentrations were evaluated in available patients to distinguish PCNSL from systemic non-Hodgkin lymphoma (sNHL).
Methods
Patient screening
Patients with the initial diagnosis of PCNSL based on histopathological evidence from January 2012 to March 2022 in First Affiliated Hospital of Chongqing Medical University were enrolled. A systematic CT scan or PET/CT scan is used to exclude systemic lymphomas. Patients with evidence of relapsed lymphomas or secondary central nervous system lymphomas were excluded in this study.
In CSF examination, Patients with PCNSL and systematic non-Hodgkin lymphoma (sNHL) whose CSF data were available would be enrolled. The patients should be initial diagnosis and without any immunosuppressive therapy, no previous disease with immune system abnormalities. SNHL was confirmed by pathological evidence and whole-body PET/CT scan. The patients received bone marrow aspirate and flow cytometry to exclude lymphoma cells infiltrating the bone marrow. The data of IL levels in CSF were available before treatment. Informed consents were obtained from all patients, and the study protocol was approved by the Human ethics committee of the Affiliated Hospital of Chongqing Medical University.
Clinical data
The clinical data of PCNSL patients were collected, including gender, age, chief complaint symptoms, HIV infection status, LDH value, biopsy approach, and treatments. The lesions’ features were evaluated by MRI scan; CSF examination included protein level, glucose level, nucleated cells, and flow cytometry. IL concentrations in CSF included IL-5, IL-6, IL-8, and IL-10 proteins; the protein level was measured by multiple microsphere flow immunofluorescence techniques; the detection kit was provided by LTD Qingdao Raisecare Biological Technology Co., Ltd.
Histopathology
The specimens were preserved and paraffin-embedded; the sliced tissues were observed after hematoxylin–eosin staining (HE) staining. Protein expression was assessed by immunohistochemistry (IHC): Ki67, TP53, BCL-2, BCL-6, MYC, CD10, and MUM-1, and the expression of more than 30% of lymphoma cells was applied for positive [12]; TP53 protein expression more than10% was considered positive [13]. According to the Hans algorithm, PCNSL was further divided into germinal center B cell (GCB) and non-germinal center B-cell (non-GCB) [3]. The results were re-read by two pathologists to confirm the diagnosis.
Treatments and prognosis
The treatment approaches and prognosis of patients with PCNSL were collected. The choice of treatment approaches was decided by the clinician according to the patient’s condition and objective. The study endpoint was the time of the last follow-up or patient’s death, and overall survival (OS) was defined as the time from the patient's diagnosis to the study endpoint.
Statistical analysis
The univariate analysis used Kaplan–Meier’s test; all variables with P values less than 0.20 in univariate analysis were involved in the Cox proportional hazards model. The Mann–Whitney U test was used to compare the IL concentrations in patients, the receiver operating characteristic (ROC) curve analysis to investigate the optimal values of IL in PCNSL and sNHL, and the area under the ROC curve(AUC) > 0.80, the cutoff value was defined as meaningful for diagnosis. In all analyses, P < 0.05 indicated statistical significance. All graphics and statistical methods were conducted with the software packages SPSS (version 26.0; IBM Corporation, Armonk, NY, USA) and GraphPad Prism (Datamatics 8.0, San Diego, California, USA).
Results
Patient cohort: clinical features
64 patients with PCNSL were diagnosed in our department, and the HIV infection status of patients was negative. In 64 patients, 65.63% (42/64) were male, the male: female ratio was 1.91, and the median age was 54.50 years (range 16–85) (Fig. 1). The complaint symptoms involved various neurological symptoms, headache presented in 42.19% (27/64) patients, dizziness in 26.56% (17/64), numbness and weakness in 20.31% (13/64), nausea and vomiting in 7.81% (5/64), vision loss in 6.25% (4/64), slurred speech in 3.13% (2/64), and apathism, unsteady, hemiplegia, facial paralysis, which were relatively rare, just presented in 1.57% (1/64). 79.69% (51/64) of patients had only one symptom, 14.06% (9/64) had two symptoms, and 6.25% (4/64) had three and more symptoms. The specimens were obtained by stereotactic biopsy, incisional biopsy, and surgical resection. The median LDH of all patients was 236U/L (range 96–723U/L) (Table 1).
Auxiliary examinations (MRI, pathology, and CSF)
MRI
The features of lesions in patients with PCNSL were assessed by brain image examination, brain MRI would be conducted as patient was suspected with abnormality in the brain. The MRI image revealed 32.81% (21/64) of patients with lesions in the parietal lobe, 29.69% (19/64) of patients in the frontal lobe, 23.44% (15/64) of patients in the basal lobe, 14.06% (9/64) of patients in the temporal lobe, 12.50% (8/64) of patients in the occipital lobe, 6.25% (4/64) of patients in the retrobulbar and involving the optic nerve, 4.69% (3/64) of patients in the cerebellum, 3.13% (2/64) of patients in the sellar region, 3.13% (2/64) of patients in the thalamus, and 1.56% (1/64) of patients in the precentral gyrus. Solitary lesions presented in 67.19% (43/64) of patients and multiple lesions were presented in 32.81% (21/64) patients. The median size of lesions was 3.25 × 3.09 cm (range 1.60 × 2.10–8 × 5 cm). The edema was observed around the lesions in 35 (54.67%) patients (Table 1).
Pathology
89.06% (57/64) of patients with PCNSL were diffuse large B-cell lymphoma (DLBCL), the subtype of non-GCB accounted for 64.91% (37/57), and GCB accounted for 35.09% (20/57). Other uncommon types include B lymphoblastic lymphoma and NK/T-cell lymphoma accounted for 3.13% (2/64); follicular lymphoma, anaplastic large cell lymphoma, and mantle cell lymphoma accounted for 1.56% (1/64). Immunohistochemistry presented TP53 protein expression was positive in 56.25% (36/64) of patients, MYC expression was positive in 35.93% (23/64) of patients, and BCL-2 and BCL-6 proteins were positive in 51.56% (33/64) and 45.31%(29/64) of patients respectively. CD10 expression was positive only in 23.44% (15/64) of patients. The median Ki67 expression was 70% (Table 2).
CSF
The CSF examination was available in 27 patients with PCNSL and 21 patients with sNHL. IL levels of IL-5, IL-6, IL-8, and IL-10 in CSF were detected. In patients with PCNSL, the median value of CSF protein was 0.50 g/L (range 0.17–4.70), the median value of nucleated cells was 4.00 × 106/L (range 0.30 × 106–5.00 × 106), and the median value of glucose was 3.60 mmol/L (range 2.80–4.70). According to flow cytometry of CSF, abnormal monoclonal lymphoma cells were detected in 11.11% (3/27) patients. The median value of IL-5 concentration was 2.00 pg/mL (range 0.20–9.38), IL-6 was 4.20 pg/mL (range 0.96–198.14), and IL-10 was 3.80 pg/mL (range 0.19–339.98). The value of IL-8 was relatively high, and the median value was 198 pg/mL (range 70.79–482.00) (Table 2).
Treatments
The treatments for patients with PCNSL included chemotherapy (CT), radiotherapy (RT), autologous hematopoietic stem cell transplantation (auto-HSCT), and intraocular injection. 35.94% (23/64) patients received chemotherapy, 18.75% (12/64) received supportive treatment, 14.06% (9/64) patients received CT combined with whole brain RT, 12.50% (8/64) received auto-HSCT, 9.38% (6/64) received BTK inhibitors (BTKi) chemotherapy, 7.81% (5/64) received whole brain RT, and 1.56% (1/64) received an intraocular injection of MTX (Table 2). After the treatment, 32.81% (21/64) patients achieved complete remission (CR), 35.94% (23/64) patients achieved partial remission (PR), and the overall effective rate (OR) was 68.75%. 3.13% (2/64) patients were in stable disease (SD), and 28.13% (18/64) patients had disease progress (PD).
Prognostic factors
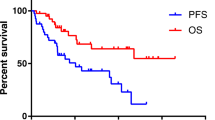
This study analyzed the prognostic factors of patients with PCNSL. The median follow-up time of all patients was 12 months (range1–84) and 35.94% (23/64) of patients alive until the final follow-up time; the median survival time was 24 months. 41 patients died during the follow-up time; the median survival time was 8 months. A total of 16 clinical factors were analyzed to clarify the prognosis. The OS of patients was not influenced by age, gender, the value of LDH, size of lesions, or CSF tests (P > 0.050) (Table 3). However, patients with multiple lesions were an adverse factor of OS (P = 0.000). The BCL2, BCL6, TP53, and MYC expression did not affect the OS of patients (P > 0.05), but the expression of Ki67 ≥ 75% exhibited a worse prognosis (P = 0.041) (Fig. 2A). In terms of treatments, one patient with intraocular injection was excluded and 63 patients participated in the statistical analysis, the analysis result displayed different treatments were significant predictors of patients (P = 0.000), and Auto-HSCT could better improve the OS of patients in comparison with other treatments (P < 0.050). Chemotherapy, radiotherapy, the combination of radiotherapy, and BTKi chemotherapy were associated with favorable OS when compared with supportive treatment (P = 0.000), but the OS was not different among them (P > 0.050) (Fig. 2B). Multivariate analysis showed auto-HSCT displayed significantly more superior OS than chemotherapy (P = 0.036), but there was no significant difference with radiotherapy, combined therapy, and BTKi chemotherapy. Although BCL2 expression did not affect OS in univariate analysis, it adversely affected OS in multivariate analysis (P = 0.029) (Fig. 3).
A Kaplan–Meier analysis of potential prognostic factors. Overall survival (OS) in patients with age ≥ 60 years and age < 60 years (a), LDH level ≥ 215 U/L and LDH level < 215 U/L (b), multifocal lesions and unifocal lesions (c), OS in patients with different pathological subtypes (d), BCL-2 expression positive and negative (e), Ki 67 expression ≥ 75% and < 75% (f). B Kaplan–Meier analysis of treatments. OS in PCNSL patients treated with auto-HSCT, chemotherapy, radiotherapy(RT), chemotherapy combined with RT, and supportive treatment (a), active treatment and supportive treatment (b), OS in PCNSL patients treated with chemotherapy, RT, chemotherapy combined with RT (c), BTKi chemotherapy and auto-HSCT (d), BTKi, auto-HSCT, and chemotherapy (e), BTKi and chemotherapy (f)
Difference in IL levels
DLBCL was 66.67% (14/21) in patients with sNHL, which was the major histology, and there was no difference in baseline data of patients with PCNSL and sNHL (Table 4). The median of IL-5 concentration in sNHL was 2.11 pg/mL (range 1.14–5.12), IL-6 concentration was 3.88 pg/mL (range 2.58–16.72), and IL-8 concentration was 315 pg/mL (range 145.20–515). According to the comparison, the IL-5, IL-6, and IL-8 concentrations were no significant difference between the two subtypes of lymphomas (P > 0.05). However, the median of IL-10 concentration in sNHL was 0.37 pg/mL (range 0.27–0.74), and that in PCNSL was 3.80 pg/mL (range 0.90–10.31), the difference was significant (P = 0.000), and IL-10 value was significantly higher in PCNSL (Fig. 4A). Excluding other histopathologies of NHL, there was still a significant difference in IL-10 value between DLBCL of PCNSL and sDLBCL (P = 0.003) (Fig. 4B).
A The comparison of the median value of cerebrospinal fluid interleukin (IL) concentrations in patients with primary central nervous system lymphomas (PCNSL) and patients with systemic non-Hodgkin lymphoma (sNHL). B The comparison of the median value of IL concentrations in patients with DLBCL of PCNSL and sDLBCL
Referring to previous studies of PCNSL, ROC curve analysis was performed in the IL-10, IL-6, and IL-10/IL-6 level of PCNSL and sNHL. The results showed the cutoff value of IL-10 concentration was 0.43 pg/mL, sensitivity was 96.3%, specificity was 66.67%, and AUC was 0.84 (0.71–0.96); cutoff value of IL-10/IL-6 ratio was 0.21, sensitivity was 81.48%, specificity was 80.95%, and AUC was 0.83 (0.71–0.95); and cutoff value of IL-6 was 3.71 pg/m, sensitivity was 66.67%, specificity was 47.62%, and AUC was 0.51 (0.33–0.68) (Fig. 5).
Discussion
In this study, the clinical features of 64 PCNSL patients were analyzed. The gender, age, and clinical manifestations were similar to previous studies [14,15,16]. The high incidence age stage was 60–69 years as reported previously, but the median age in this study was younger, maybe PCNSL tends to develop in younger patients in recent years. The lesions of PCNSL in MRI generally were different from systemic lymphoma or metastases tumors which often with mild edema around the lesions [17]; in this study, 54.67% of patients showed edema around the mass in MRI, which was consistent with previous reports. In addition, although the pathological types of patients were mainly non-GCB (64.91%), the proportion was lower than that in previous studies, and BCL6 protein expression was lower, while the CD10 expression was higher [14, 18], and in addition, the immunohistochemistry showed the lymphomas in this study were more prone to expressed TP53 protein.
The prognostic factors of PCNSL are controversial, and the conclusions of previous research are not completely consistent. A study showed the factors of age > 60 years, high IELSG score, and overexpression of MYC were associated with worse prognosis [19]. Sopittapan et al. also found age > 60 years was a significant poor prognostic factor [18]. Two other studies have shown cell origin of DLBCL, and lesion characteristics affect the prognosis of patients [20]. TP53 is an indicator of poor prognosis in many tumors, it was also a poor prognosis factor in PCNSL [21], and BCL2 expression may be a poor prognostic factor [22]. Studies have shown patients with the expression of immune checkpoint inhibitors such as PD-1 and PD-L1 exhibited worse OS [23]. In recent years, the analysis of prognosis has gradually extended to molecular biology, whole-exome sequencing (WES) showed MYD88 and CD79B mutations could be detected in more than 60% of patients [24], and ETV6, BTG1, TBL1XR1 mutations could be detected in about 30% of patients, but the prognostic significance of these mutated genes is unclear [25, 26]. In this study, the analysis of prognostic factors refers to The International Extranodal Lymphoma Study Group (IELSG) mode, and factors such as cerebrospinal fluid cytokines were also included. The multiple lesions and expression of Ki67 ≥ 75% were poor prognosis factors associated with worse OS. Multivariate analysis revealed overexpression of BCL2 protein was an adverse factor, and the choice of treatment was also a factor affecting OS.
Analysis of treatments and consolidation of auto-HSCT (with Thiotepa regimen) could prolong OS as a favorable prognostic factor and was the most effective treatment in this study. Several recent studies have also shown that HDC-ASCT consolidation therapy after high-dose MTX chemotherapy has ORR (> 90%) and prolonged PFS (> 74 m), and Thiotepa-based conditioning regimens are better than BCNU and BEAM commonly used lymphoma transplantation programs [27,28,29]. In a 7-year randomized trial study, high-dose MTX regimen chemotherapy was followed by auto-HSCT with a 7-year OS of 70%, WBRT although the therapeutic effect is similar to auto-ASCT, the symptoms of neurological damage were more obvious [30]. Although lymphoma tissue is sensitive to radiotherapy, some studies have shown chemotherapy combined with whole brain radiotherapy can better improve the prognosis [18], but a large phase III study randomized patients showed that MTX based with a complete response and then randomized to 45 Gy WBRT can improve the PFS, but no benefit to OS [31]. Although the combination of chemotherapy and low-dose whole-brain radiotherapy is one of the treatment options with less neurotoxicity, many chemotherapeutic regimens and targeted drugs with good effects have gradually replaced the status of radiotherapy. BTK inhibitors act on the BCR pathway, as a well-targeted drug that can pass through the BBB, BTK inhibitors were the most potential target for PCNSL, and ibrutinib demonstrated an ORR rate of 52% as of single therapy and could reach 80% with MTX [32]. Many clinical studies for the application of the new generation of BTKi in PCNSL were underdeveloped. However, in this study, the patients with BTKi chemotherapy showed no obvious advantage to prolonging OS than CT and RT, which may be related to the small cases in this study.
In addition, this study analyzed cytokines in CSF, but the abnormally increased cytokines had no significant effect on the prognosis of patients with PCNSL. However, the CSF IL-10 concentration in PCNSL was significantly higher than in sNHL. The ROC curve analysis displayed a cutoff value of 0.43 pg/mL, and the AUC revealed it was meaningful for diagnosis. IL-10 was strong immunosuppressive and anti-inflammatory cytokines in PCNSL and plays an important role in the progression of lymphoma [33]. A recent prospective study enrolled 118 cases of PCNSL; the results also showed IL-10 in CSF was higher in PCNSL than in other types of lymphoma, setting a cut-off level of 2.0 pg/mL [34]. Similar data were reported by Sasagawa et al., IL-10 in CSF with a cut-off of 3 pg/mL, providing a sensitivity and specificity of 94.7% and 100%, respectively [35]. Two other studies showed that CSF concentrations of IL-10 are significantly increased in PCNSL and can predict the recurrence of PCNS 67 days earlier than MRI [36,37,38]. Some studies also showed that IL-10 combined with the IL-10/IL-6 ratio can better determine the diagnosis of PCNSL [39]. Previous studies have reported a cutoff value of IL-10/IL-6 ratio of 0.94 in PCNSL, and AUC is 0.92; it was also meaningful to distinguish PCNSL from other lymphomas [34]. In this study, the cutoff value of the IL-10/IL-6 ratio was 0.21, the AUC suggesting this index has a diagnostic value for PCNSL. Other studies have shown that the concentration of IL-6 is significantly higher in central inflammatory changes for PCNSL; IL-6 may also be an effective cerebrospinal fluid marker [40]. However, the IL-6 level in this study indicated little significance for differential diagnosis of PCNSL. Other biological markers in CSF of PCNSL including MYD88, CXCL13, microRNAs, and free light chains have also been studied as predictive biomarkers [34, 41,42,43]. The limitation of this study is the limited number of cases in PCNSL and sNHL, and peripheral blood IL-10 levels were not tested in study. Therefore, it is challenging to fully clarify the role of IL-10 in differential diagnosis of PCNSL and sNHL. In the future, we needed to expand samples and make more comprehensive exploration to clarify this problem.
In conclusion, this study analyzed the clinical features and prognostic factors of PCNSL. At the same time, we found the IL-10 concentration in CSF and IL-10/IL-6 ratio in patients with PCNSL was different from sNHL, which was helpful for the diagnosis of PCNSL.
Data availability
All data and code generated or used during the study appear in the submitted article.
References
Dolecek TA, Propp JM, Stroup NE, Kruchko C (2012) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2005–2009. Neuro Oncol 14(Suppl 5):v1-49
Grommes C, DeAngelis LM (2017) Primary CNS Lymphoma. J Clin Oncol 35(21):2410–2418
Ferreri AJM, Teresa C, Marco CG, et al. (2019) R-CHOP preceded by blood-brain barrier permeabilization with engineered tumor necrosis factor-α in primary CNS lymphoma. Blood 134(3)
Eloranta S, Brånvall E, Celsing F et al (2018) Increasing incidence of primary central nervous system lymphoma but no improvement in survival in Sweden 2000–2013. Eur J Haematol 100(1):61–68
Farrall AL, Smith JR (2021) Changing incidence and survival of primary central nervous system lymphoma in Australia: a 33-year national population-based study. Cancers (Basel) 13(3)
Weller M, Martus P, Roth P, Thiel E, Korfel A (2012) Surgery for primary CNS lymphoma? Challenging a paradigm. Neuro Oncol 14(12):1481–1484
Krebs S, Barasch JG, Young RJ, Grommes C, Schöder H (2021) Positron emission tomography and magnetic resonance imaging in primary central nervous system lymphoma-a narrative review. Ann Lymphoma. 5
Best MG, Sol N, Zijl S, Reijneveld JC, Wesseling P, Wurdinger T (2015) Liquid biopsies in patients with diffuse glioma. Acta Neuropathol 129(6):849–865
Roschewski M, Dunleavy K, Pittaluga S et al (2015) Circulating tumor DNA and CT monitoring in patients with untreated diffuse large B-cell lymphoma: a correlative biomarker study. Lancet Oncol 16(5):541–549
Schroers R, Baraniskin A, Heute C et al (2010) Diagnosis of leptomeningeal disease in diffuse large B-cell lymphomas of the central nervous system by flow cytometry and cytopathology. Eur J Haematol 85(6):520–528
Baraniskin A, Kuhnhenn J, Schlegel U et al (2011) Identification of microRNAs in the cerebrospinal fluid as marker for primary diffuse large B-cell lymphoma of the central nervous system. Blood 117(11):3140–3146
Green TM, Young KH, Visco C et al (2012) Immunohistochemical double-hit score is a strong predictor of outcome in patients with diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol 30(28):3460–3467
Young KH, Leroy K, Møller MB et al (2008) Structural profiles of TP53 gene mutations predict clinical outcome in diffuse large B-cell lymphoma: an international collaborative study. Blood 112(8):3088–3098
Yuan XG, Huang YR, Yu T et al (2020) Primary central nervous system lymphoma in China: a single-center retrospective analysis of 167 cases. Ann Hematol 99(1):93–104
Radotra BD, Parkhi M, Chatterjee D et al (2020) Clinicopathological features of primary central nervous system diffuse large B cell lymphoma: experience from a tertiary Center in North India. Surg Neurol Int 11:424
Dalia S, Forsyth P, Chavez J et al (2014) Primary B-cell CNS lymphoma clinicopathologic and treatment outcomes in 89 patients from a single tertiary care center. Int J Hematol 99(4):450–456
Bataille B, Delwail V, Menet E et al (2000) Primary intracerebral malignant lymphoma: report of 248 cases. J Neurosurg 92(2):261–266
Sopittapan T, Tunthanathip T, Kaewborisutsakul A (2020) Outcome and prognostic factors of primary central nervous system lymphoma in Southern Thailand. Asian J Neurosurg 15(3):560–565
Gomes Candido Reis D, Levy D, Lage L et al (2021) New genetic prognostic biomarkers in primary central nervous system lymphoma (PCNSL). Brain Behav 11(4):e02061
Niparuck P, Boonsakan P, Sutthippingkiat T et al (2019) Treatment outcome and prognostic factors in PCNSL. Diagn Pathol 14(1):56
Munch-Petersen HD, Asmar F, Dimopoulos K et al (2016) TP53 hotspot mutations are predictive of survival in primary central nervous system lymphoma patients treated with combination chemotherapy. Acta Neuropathol Commun 4:40
Villa D, Tan KL, Steidl C et al (2019) Molecular features of a large cohort of primary central nervous system lymphoma using tissue microarray. Blood Adv 3(23):3953–3961
Kim S, Nam SJ, Park C et al (2019) High tumoral PD-L1 expression and low PD-1(+) or CD8(+) tumor-infiltrating lymphocytes are predictive of a poor prognosis in primary diffuse large B-cell lymphoma of the central nervous system. Oncoimmunology 8(9):e1626653
Nayyar N, White MD, Gill CM et al (2019) MYD88 L265P mutation and CDKN2A loss are early mutational events in primary central nervous system diffuse large B-cell lymphomas. Blood Adv 3(3):375–383
Chapuy B, Roemer MG, Stewart C et al (2016) Targetable genetic features of primary testicular and primary central nervous system lymphomas. Blood 127(7):869–881
Ou A, Sumrall A, Phuphanich S et al (2020) Primary CNS lymphoma commonly expresses immune response biomarkers. Neurooncol Adv 2(1):vdaa018
Houillier C, Taillandier L, Dureau S et al (2019) Radiotherapy or autologous stem-cell transplantation for primary CNS lymphoma in patients 60 years of age and younger: results of the intergroup ANOCEF-GOELAMS randomized phase II PRECIS study. J Clin Oncol 37(10):823–833
Illerhaus G, Kasenda B, Ihorst G et al (2016) High-dose chemotherapy with autologous haemopoietic stem cell transplantation for newly diagnosed primary CNS lymphoma: a prospective, single-arm, phase 2 trial. Lancet Haematol 3(8):e388–e397
Omuro A, Correa DD, DeAngelis LM et al (2015) R-MPV followed by high-dose chemotherapy with TBC and autologous stem-cell transplant for newly diagnosed primary CNS lymphoma. Blood 125(9):1403–1410
Ferreri A, Cwynarski K, Pulczynski E et al (2022) Long-term efficacy, safety and neurotolerability of MATRix regimen followed by autologous transplant in primary CNS lymphoma: 7-year results of the IELSG32 randomized trial. Leukemia 36(7):1870–1878
Thiel E, Korfel A, Martus P et al (2010) High-dose methotrexate with or without whole brain radiotherapy for primary CNS lymphoma (G-PCNSL-SG-1): a phase 3, randomised, non-inferiority trial. Lancet Oncol 11(11):1036–1047
Grommes C, Tang SS, Wolfe J et al (2019) Phase 1b trial of an ibrutinib-based combination therapy in recurrent/refractory CNS lymphoma. Blood 133(5):436–445
Mosser DM, Zhang X (2008) Interleukin-10: new perspectives on an old cytokine. Immunol Rev 226:205–218
Ferreri A, Calimeri T, Lopedote P et al (2021) MYD88 L265P mutation and interleukin-10 detection in cerebrospinal fluid are highly specific discriminating markers in patients with primary central nervous system lymphoma: results from a prospective study. Br J Haematol 193(3):497–505
Sasagawa Y, Akai T, Tachibana O, Iizuka H (2015) Diagnostic value of interleukin-10 in cerebrospinal fluid for diffuse large B-cell lymphoma of the central nervous system. J Neurooncol 121(1):177–183
Nguyen-Them L, Costopoulos M, Tanguy ML et al (2016) The CSF IL-10 concentration is an effective diagnostic marker in immunocompetent primary CNS lymphoma and a potential prognostic biomarker in treatment-responsive patients. Eur J Cancer 61:69–76
Shao J, Chen K, Li Q et al (2020) High level of IL-10 in cerebrospinal fluid is specific for diagnosis of primary central nervous system lymphoma. Cancer Manag Res 12:6261–6268
Zhang Y, Zou D, Yin J et al (2021) Changes in cerebrospinal fluid interleukin-10 levels display better performance in predicting disease relapse than conventional magnetic resonance imaging in primary central nervous system lymphoma. BMC Cancer 21(1):183
Costopoulos M, Kim R, Choquet S et al (2018) Cerebrospinal fluid interleukin (IL)-10 and IL-10:IL-6 ratio as biomarkers for small B-cell lymphoproliferations with leptomeningeal dissemination. Semin Hematol 55(4):179–181
Ungureanu A, Le Garff-Tavernier M, Costopoulos M et al (2021) CSF interleukin 6 is a useful marker to distinguish pseudotumoral CNS inflammatory diseases from primary CNS lymphoma. J Neurol 268(8):2890–2894
Schroers R, Baraniskin A, Heute C et al (2010) Detection of free immunoglobulin light chains in cerebrospinal fluids of patients with central nervous system lymphomas. Eur J Haematol 85(3):236–242
Rubenstein JL, Wong VS, Kadoch C et al (2013) CXCL13 plus interleukin 10 is highly specific for the diagnosis of CNS lymphoma. Blood 121(23):4740–4748
Mihailovich M, Bremang M, Spadotto V et al (2015) miR-17-92 fine-tunes MYC expression and function to ensure optimal B cell lymphoma growth. Nat Commun 6:8725
Acknowledgements
The authors would like to thank all the members of their department for their contributions.
Author information
Authors and Affiliations
Contributions
Junnan Li designed and performed study, analyzed and interpreted data, and wrote the manuscript. Li Yang and Lin Liu performed the study and revised the manuscript. Xiaoqiong Tang and Xiaohua Luo guided the study. Dan Li provided data for the study. All authors read and approved the final manuscript. Li Yang and Lin Liu have equivalent contributions to the study.
Corresponding author
Ethics declarations
Ethics approval
This study was approved according to the ethical guidelines of the First Affiliated Hospital of Chongqing Medical University (institutional review board) and was performed according to the Declaration of Helsinki.
Consent to participate
Written informed consent was obtained from the patients.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Novelty statements
This work further investigates unique clinical features and prognostic factors of primary central nervous system lymphoma (PCNSL) and explains applications of cerebrospinal fluid (CSF) interleukin (IL) concentrations in patients with PCNSL.
The study finds BCL2 expression is an unfavorable prognostic marker and autologous hematopoietic stem cell transplantation is the most effective method to prolong overall survival (OS) of PCNSL, IL-10 levels and IL-10/IL-6 ratio in CSF are useful biomarkers for distinguishing PCNSL from sNHL.
Those results will help us understand PCNSL more clearly and provide theoretical basis for non-invasive diagnosis and differential diagnosis of PCNSL.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, J., Tang, X., Luo, X. et al. Clinicopathological analysis and specific discriminating markers of interleukin detection in cerebrospinal fluid with primary central nervous system lymphoma: results from a retrospective study. Ann Hematol 102, 2153–2163 (2023). https://doi.org/10.1007/s00277-023-05301-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05301-7