Abstract
Idarubicin 12 mg/m2 has been recommended as a standard induction therapy for acute myeloid leukemia (AML). It is unknown whether a higher dose of idarubicin can improve the remission rate. This phase 2 prospective single-arm study enrolled 45 adults with newly diagnosed AML between September 2019 and May 2021 (NCT 04,069,208). Induction therapy included administration of idarubicin 14 mg/m2 for 3 days and cytarabine 100 mg/m2 every 12 h subcutaneously for 7 days. The primary endpoint was the composite complete response rate (complete response (CR) plus complete response with incomplete blood count recovery (CRi)). The median age was 45 years (range 14–60 years). Forty (88.9%) patients had CR or CRi, including 39 patients with CR and 1 patient with CRi after one course of induction therapy. The median times to recovery of absolute neutrophil and platelet counts were 21 days. Only 1 patient died of intracranial hemorrhage during induction therapy. After a median follow-up of 14 months (range 3.5–24 months), the estimated 18-month overall survival and disease-free survival (DFS) were 66.9% and 57.5%, respectively. In conclusion, idarubicin 14 mg/m2 plus cytarabine was a safe and efficient intensive regimen for younger and fit patients with newly diagnosed AML.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The combination of anthracycline plus cytarabine has been the standard induction therapy for acute myeloid leukemia (AML) for more than 3 decades. For young and fit adults, the complete remission rates (CRs) are approximately 60% after one course [1,2,3]. Over the years, modifications to the anthracycline plus cytarabine induction strategy have been implemented. Studies have shown that daunorubicin 90 mg/m2 provides a higher complete remission rate and higher overall survival than daunorubicin 45 mg/m2 as part of the 7 + 3 regimen [4,5,6]. These results indicate that anthracycline dose intensification could improve complete remission and survival. Other efforts have included using alternative anthracyclines. A randomized trial by EORTC-GIMEMA compared daunorubicin 50 mg/m2, mitoxantrone 12 mg/m2, and idarubicin 10 mg/m2 plus cytarabine and etoposide, and the results showed that mitoxantrone or idarubicin improved the 5-year disease-free survival and overall survival rates compared with daunorubicin [7]. Pautas and colleagues also showed improved rates of complete remission and 4-year event-free survival with administration of idarubicin 12 mg/m2 compared with daunorubicin 80 mg/m2 for 3 days [8]. Another randomized trial compared daunorubicin 90 mg/m2 and idarubicin 12 mg/m2 plus cytarabine. After one course of induction, 69.2% of patients attained CR. The CR rate and survival did not show significant differences between the two arms [9]. Based on these results, administration of idarubicin 12 mg/m2 for 3 days is used as standard induction therapy for young and fit newly diagnosed AML.
Although the remission rate and survival have improved in recent years, it is still important to improve induction chemotherapy, since better initial cytoreduction and induction of minimal residual disease negativity can reduce or delay the risk of subsequent relapse and thereby improve survival [10,11,12]. In a previous study, daunorubicin dose intensification improved the complete remission rate and survival, suggesting the potential of further intensifying the anthracycline dose. Idarubicin doses greater than 12 mg/m2/day have rarely been investigated. To address these questions, we designed this phase 2, prospective, single-arm study to evaluate the efficacy and safety of administration of idarubicin 14 mg/m2 for 3 days plus a standard dose of cytarabine as induction therapy for younger (aged ≤ 60 years) and fit patients with newly diagnosed AML.
Methods
Study design and participants
This phase 2, single-center, single-arm trial was conducted by the Peking Union Medical College Hospital (Beijing, China). All patients aged 60 years or younger with newly diagnosed de novo AML were considered eligible candidates for this study. Patients with acute promyelocytic leukemia or secondary AML with a history of antecedent hematological disorders, including myelodysplastic syndrome, chronic myelomonocytic leukemia, or myeloproliferative neoplasms, were not eligible. No lower age limit was specified in the protocol, but this trial was performed in the adult leukemia department; therefore, treated patients were aged 14 years and older. All patients were required to have an ejection fraction of > 50% determined by echocardiography. Other eligibility criteria included an Eastern Cooperative Oncology Group performance status of 2 or less and good organ function.
Informed consent was obtained from all patients, and the protocol was approved by the Peking Union Medical College Hospital Ethics Committee. The study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Cytogenetic, molecular, and measurable residual disease analyses
Cytogenetic evaluation using standard metaphase karyotype analysis and molecular analysis via a 42-gene next-generation sequencing platform was performed (as previously described) at study enrollment [13]. Patients were classified into three risk groups according to the 2017 European LeukemiaNet (ELN) criteria [14]. Measurable residual disease (MRD) was assessed by 8-color multiparameter flow cytometry based on leukemia-associated immunophenotypes or differences from normal samples with a minimum sensitivity of 10−3 (0.1%).
Procedures and response criteria
IA14 induction consisted of administration of idarubicin 14 mg/m2 for 3 days and cytarabine 100 mg/m2 every 12 h subcutaneously for 7 days. Bone marrow aspiration was performed on days 21 to 28. For patients showing persistent leukemia after initial induction chemotherapy, the second cycle of induction therapy consisted of administration of idarubicin 10 mg/m2 (or daunorubicin 60 mg/m2) for 3 days, cytarabine 100 mg/m2 every 12 h subcutaneously for 7 days, and etoposide 100 mg/m2 for 3 days. Antifungal prophylaxis was recommended during periods of neutropenia. Patients who achieved CR proceeded to consolidation courses with administration of high-dose cytarabine at 3 g/m2 every 12 h for 3 days. Allogeneic hematopoietic stem cell transplantation (HSCT) was offered to high-risk patients or intermediate-risk patients who had available donors. CR and complete response with incomplete blood count recovery (CRi) were determined by using the 2017 ELN response criteria [11].
Outcome
The primary endpoint was to determine the composite complete response rate (CR and CRi) after IA14 induction. Secondary endpoints included toxicity, disease-free survival (DFS), and overall survival (OS). DFS was calculated from the date of remission (inclusive of CR and CRi) to the date of relapse or death from any cause. OS was defined as the duration from initiation of treatment to the date of death or last follow-up. In patients who experienced remission, the time to neutrophil recovery was measured from day 1 of induction treatment until the first day that the absolute neutrophil count was ≥ 500 cells per μL, and the time to platelet recovery was measured from day 1 of induction until the platelet count was ≥ 20 000 platelets per μL. Adverse events were assessed according to National Cancer Institute Common Terminology Criteria for Adverse Events version 4.0.
Statistical analysis
The clinical and demographic characteristics of the study participants were summarized using descriptive statistics. All analyses were performed using SPSS statistics version 24.0 (SPSS Inc., Chicago, IL, USA). Time-to-event variables (OS and DFS) were estimated according to Kaplan–Meier survival analysis and compared with the log-rank test. Comparisons between the variables of interest were performed using univariate Cox regression models. P < 0.05 was considered statistically significant. The final follow-up date was August 31, 2021. The study is registered with ClinicalTrials.gov, number NCT 04,069,208.
Data sharing statement
Individual participant data will not be available. Study protocol will be available beginning 9 months and ending 36 months following article publication at caoxinxin@pumch.cn.
Results
From September 2019 to May 2021, 45 patients were eligible for the study. The baseline characteristics of the 45 patients are summarized in Table 1. The median age was 45 years (range 14–60 years). ELN risk was favorable in 44.4%, intermediate in 28.9% and adverse in 26.7% of patients. Core-binding factor mutations were present in 9 patients (20%), including 7 patients with RUNX1-RUNX1T1 and 2 patients with CBFB-MYH11. A diploid karyotype was present in 18 (40%) of 45 patients. Other intermediate-risk karyotypes were present in nine (20%) patients, and adverse-risk or complex cytogenetics were present in six (13.3%) patients. Five (11.1%) patients harbored KMT2A rearrangements. Baseline cytogenetics were not available in 2 (4.4%) patients because of insufficient metaphases obtained for analysis. Mutations of NPM1 (22.2%), FLT3-ITD (20.0%, 8/9 were FLT3-ITDhigh), DNMT3A (15.6%), CEBPA (15.6%, 5/7 were biallelic mutated), IDH2 (13.3%), WT1 (13.3%), NRAS (13.3%), and IDH1 (8.9%) were common.
After 1 course of IA14 induction therapy, 40 (88.9%) patients had CR or CRi, including 39 (86.7%) who had CR and 1 (2.2%) who had CRi. One patient died of intracerebral hemorrhage during induction therapy. Patients who did not achieve CR received a second course of induction therapy (3 patients received daunorubicin combined with cytarabine and etoposide, and 1 patient received idarubicin combined with cytarabine and etoposide). Three of 4 patients achieved CR after the second course of induction. In total, 43 (95.6%) patients had CR or CRi after induction therapy. The patients who did not respond had ELN adverse-risk disease with a high allelic ratio of FLT-ITD mutation. Eleven (27.5%) of 40 patients with CR or CRi attained MRD negativity after IA14 induction.
The median time to recovery of an absolute neutrophil count of 500 or more cells per μL was 21 days (range, 18–32 days) and that to recovery of a platelet count of 20,000 or more per μL was 21 days (range, 14–27 days). Count recovery data included only responding patients.
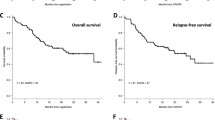
After a median follow-up of 14 months (range 3.5–24 months), 11 patients had died. One patient died of intracerebral hemorrhage during induction, 1 patient died of graft versus host disease after allogenic HSCT, and 9 patients died of disease relapse. The median OS was not reached; the estimated 18-month OS was 66.9% (Fig. 1A). The median DFS was 20 months (95% CI, 14.4–25.6 months); the estimated 18-month DFS was 57.5% (Fig. 1B). The estimated 18-month DFS rates were 75.2%, 64.7% and 17.2% in the ELN favorable-, intermediate-, and adverse-risk groups, respectively (p = 0.028). The median DFS was not reached, 18.5 months (95% CI, 5.7–31.3 months) and 11.5 months (95% CI, 8.8–14.2 months) in the ELN favorable-, intermediate-, and adverse-risk groups, respectively (Fig. 1C). Eight patients received allogeneic HSCT in first remission. All of them were in the ELN intermediate- or adverse-risk groups. Compared to ELN intermediate- or adverse-risk patients who did not have allogeneic HSCT, patients who had HSCT in first remission had significantly better DFS (not reached vs. 9.5 months [95% CI, 7.4–11.6 months], p = 0.004) (Fig. 1D).
The major toxicities and adverse events are summarized in Table 2. The most common adverse event was febrile neutropenia, including 40 (88.9%) grade 3 and 3 (2.4%) grade 4 cases. Other grade 3 or worse adverse events included one grade 3 case of acute appendicitis and one grade 3 case of hyperglycemia. One patient experienced paroxysmal atrial fibrillation. Death within 4 weeks of induction occurred in one patient (intracerebral hemorrhage).
Discussion
Several efforts have been made to optimize therapy to improve the outcome for patients with newly diagnosed AML over the years. Complete response is strongly associated with improved survival. There have been several efforts to achieve a higher rate of CR safely during induction therapy, including increasing the dose of cytarabine, optimizing anthracycline choice, and adding more drugs. In the current study, we built on these modifications with anthracycline dose intensification and tried to explore the safety and efficacy of higher doses of idarubicin. The results showed that 88.9% of patients achieved CR after 1 course of induction and 95.6% of patients achieved CR after 2 courses of induction. Although cross-trial comparisons should be made with caution, the rate of complete remission after IA14 induction therapy compares favorably with those in published studies using idarubicin 12 mg/m2 for 3 days in young AML patients [9, 15]. This result indicates that further anthracycline intensification in younger patients may improve the complete remission rate. Additionally, idarubicin intensification was not associated with additional toxicity. Febrile neutropenia accounted for the majority of grade 3 and grade 4 adverse events. The median times to recovery of absolute neutrophil and platelet counts were only 21 days. These results were comparable to those of administration of idarubicin 12 mg/m2 for 3 days or administration of daunorubicin 60 mg/m2 for 3 days. Only one patient died during induction therapy. The low early mortality and short times to count recovery indicate that IA14 could be used safely.
Although in this study the overall proportion of patients in the ELN favorable-risk group was higher than those in other AML cohorts, the proportion of patients in the ELN adverse-risk group was comparable with those in other AML patient cohorts [16,17,18]. Additionally, across ELN risk groups, IA14 resulted in high CR rates. In the current study, we found that outcomes differed dramatically depending on the ELN risk group. Inferior disease-free survival was observed in the intermediate- and adverse-risk groups. Allogenic HSCT in first remission led to favorable disease-free survival in the ELN intermediate- and adverse- risk groups. The data regarding patients who did not receive HSCT were confounding; however, this result may suggest that IA14 could be used to bridge AML patients to allogenic HSCT, especially in the ELN intermediate- and adverse-risk groups.
This study has several limitations. This was a single-center, single-arm, phase 2 clinical trial without a control group. As there were small numbers of patients in the subgroup analysis, limited conclusions could be drawn. Additionally, the number of patients who underwent allogeneic HSCT was relatively low. However, this study had one of the largest cohorts of younger and fit patients with newly diagnosed AML which is one of the first with the goal of evaluating the efficacy and safety of idarubicin 14 mg/m2 combined with a standard dose of cytarabine as induction therapy. This study can provide the basis for future randomized clinical trials to help confirm the benefit of increasing long-term overall survival. Larger numbers of patients and multicenter studies of IA14 as induction therapy are warranted to confirm the possible benefits and safety of the regimen.
In conclusion, this study confirmed that administration of idarubicin 14 mg/m2 for 3 days plus cytarabine was a safe and efficient intensive regimen for younger and fit patients with newly diagnosed AML. In this phase 2 prospective study from our single center experience, we observed high rates of complete remission without increased toxicity.
References
Rai KR, Holland JF, Glidewell OJ et al (1981) Treatment of acute myelocytic leukemia: a study by cancer and leukemia group B. Blood 58:1203–1212
Berman E, Heller G, Santorsa J et al (1991) Results of a randomized trial comparing idarubicin and cytosine arabinoside with daunorubicin and cytosine arabinoside in adult patients with newly diagnosed acute myelogenous leukemia. Blood 77:1666–1674
Vogler WR, Velez-Garcia E, Weiner RS et al (1992) A phase III trial comparing idarubicin and daunorubicin in combination with cytarabine in acute myelogenous leukemia: a Southeastern Cancer Study Group study. J Clin Oncol 10:1103–1111
Löwenberg B, Ossenkoppele GJ, van Putten W et al (2009) High-dose daunorubicin in older patients with acute myeloid leukemia. N Engl J Med 361:1235–1248
Fernandez HF, Sun Z, Yao X et al (2009) Anthracycline dose intensification in acute myeloid leukemia. N Engl J Med 361:1249–1259
Lee JH, Joo YD, Kim H et al (2011) A randomized trial comparing standard versus high-dose daunorubicin induction in patients with acute myeloid leukemia. Blood 118:3832–3841
Mandelli F, Vignetti M, Suciu S et al (2009) Daunorubicin versus mitoxantrone versus idarubicin as induction and consolidation chemotherapy for adults with acute myeloid leukemia: the EORTC and GIMEMA Groups Study AML-10. J Clin Oncol 27:5397–5403
Pautas C, Merabet F, Thomas X et al (2010) Randomized study of intensified anthracycline doses for induction and recombinant interleukin-2 for maintenance in patients with acute myeloid leukemia age 50 to 70 years: results of the ALFA-9801 study. J Clin Oncol 28:808–814
Lee JH, Kim H, Joo YD et al (2017) Prospective randomized comparison of idarubicin and high-dose daunorubicin in induction chemotherapy for newly diagnosed acute myeloid leukemia. J Clin Oncol 35:2754–2763
Burnett AK, Russell NH, Hills RK et al (2013) Optimization of chemotherapy for younger patients with acute myeloid leukemia: results of the Medical Research Council AML15 trial. J Clin Oncol 31:3360–3368
Holowiecki J, Grosicki S, Giebel S et al (2012) Cladribine, but not fludarabine, added to daunorubicin and cytarabine during induction prolongs survival of patients with acute myeloid leukemia: a multicenter, randomized phase III study. J Clin Oncol 30:2441–2448
Short NJ, Zhou S, Fu C et al (2020) Association of measurable residual disease with survival outcomes in patients with acute myeloid leukemia: a systematic review and meta-analysis. JAMA Oncol 6(12):1890–9
Cao XX, Cai H, Mao YY et al (2018) Next-generation sequencing-based genetic landscape and its clinical implications for Chinese acute myeloid leukemia patients. Cancer Cell Int 18:215
Döhner H, Estey E, Grimwade D et al (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129:424–447
Ohtake S, Miyawaki S, Fujita H et al (2011) Randomized study of induction therapy comparing standard-dose idarubicin with high-dose daunorubicin in adult patients with previously untreated acute myeloid leukemia: the JALSG AML201 Study. Blood 117:2358–2365
Jin J, Wang JX, Chen FF et al (2013) Homoharringtonine-based induction regimens for patients with de-novo acute myeloid leukaemia: a multicentre, open-label, randomised, controlled phase 3 trial. Lancet Oncol 14:599–608
Wei H, Wang Y, Gale RP et al (2020) Randomized trial of intermediate-dose cytarabine in induction and consolidation therapy in adults with acute myeloid leukemia. Clin Cancer Res 26:3154–3161
DiNardo CD, Lachowiez CA, Takahashi K et al (2021) Venetoclax combined with FLAG-IDA induction and consolidation in newly diagnosed and relapsed or refractory acute myeloid leukemia. J Clin Oncol 39:2768–2778
Acknowledgements
The authors thank the patients and their families.
Funding
This work was supported by the institutional research funding provided by the Non-profit Central Research Institute Fund of the Chinese Academy of Medical Sciences (Grant No. 2019-RC-HL-001 to CXX) and the Beijing Natural Science Foundation (Grant No. 7202160 to CXX).
Author information
Authors and Affiliations
Contributions
Cao XX, Li J, and Zhou DB contributed to study conception and design; Mao YY contributed to patient follow-up; Mao YY and Cao XX contributed to data analysis and interpretation; Mao YY, Cai HC, Shen KN, Chang L, Zhang L, Zhang Y, Feng J, Wang W, Yang C, Zhu TN, Duan MH, Cao XX, and Li J contributed to patient enrollment; Mao YY and Cao XX wrote the paper; and all authors revised the paper and approved the submitted version.
Corresponding authors
Ethics declarations
Ethical approval
The study was approved by each site’s Institutional Ethics Committee and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all patients included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mao, Yy., Cai, Hc., Shen, Kn. et al. Benefit of high-dose idarubicin as induction therapy in acute myeloid leukemia: a prospective phase 2 study. Ann Hematol 101, 831–836 (2022). https://doi.org/10.1007/s00277-022-04764-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-022-04764-4