Abstract
Chromosome 1q gain/amplification (1q +) has been reported to be associated with inferior outcomes in multiple myeloma (MM) patients. Big therapeutic advances have shifted the treatment landscape by introducing monoclonal antibodies. There is a relative lack of data on outcomes in patients harboring this alteration in the era of monoclonal antibodies. Baseline characteristics and therapy-related data from newly diagnosed MM patients harboring 1q + detected by fluorescence in situ hybridization (FISH) were collected in a single institution. Among 34 identified subjects, the presence of elevated LDH was found to be associated with shorter overall survival (OS), and increased bone marrow plasma cell percentage (≥ 60%) was associated with worse progression-free survival (PFS). 1q + copy number more than three was associated with both shorter OS and PFS. Additionally, the administration of lenalidomide was associated with superior OS. The use of autologous stem cell transplantation, bortezomib, or daratumumab, was found to have no prognostic benefits in our sample. Lenalidomide may be an optimal therapeutic choice for this population, and future larger studies are warranted to confirm this benefit and further investigate the role of monoclonal antibodies in this subpopulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma (MM), a neoplastic plasma cell disorder, is the second most common hematological malignancy in the USA [1]. Thirty-four thousand nine hundred twenty new cases and 12,410 deaths from multiple myeloma are estimated to occur in 2021 in the USA [2]. Myeloma is a disease having extensive inter-patient heterogeneity with respect to survival which can range from months to more than 10 years, depending on genetic variation, access to autologous stem cell transplantation (ASCT), and the availability of novel therapies [3,4,5].
Fluorescence in situ hybridization (FISH) is a popular tool to detect cytogenetic alterations which in turn, can contribute to the risk stratification of patients with MM. Genetic alterations have been integrated into the revised International Staging System [6]. Gain or amplification of CKS1B gene at chromosome 1q21 region is a common cytogenetic aberration in MM patients; it can be detected in up to 35–40% of newly diagnosed MM (NDMM) patients [7,8,9]. CKS1B is an essential member of the cyclin kinase subunit 1 protein family and plays a critical role in cell growth and division [10, 11]. Unlike high-risk cytogenetic abnormalities such as t(14;16), t(14;20), and deletion 17p (del 17p), the prognostic effect of chromosome 1q gain/amplification (1q +) remains debated, but multiple studies have reported inferior outcomes in MM patients [7, 12,13,14,15,16]. Gain or amplification of CKS1B also frequently occurs with the deletion of CDKN2C, a suppressor gene, at chromosome 1p32.3 (1p-), resulting in increased proliferation of plasma cells due to deregulation of G1 to S transition [17]. 1p- was reported to portend poor prognosis as well [18,19,20]. Given previous studies have reported conflicting results [13, 14, 21], and the prognosis of this particular population remains unclear in the era of monoclonal antibodies, we sought to describe real-world outcomes of NDMM patients harboring 1q + with or without 1p- over the last 6 years in a single institution, and to investigate the impact of concurrent chromosomal alterations and various therapeutic agents on outcomes.
Materials and methods
Patients
This retrospective study included all patients with MM as defined by the International Myeloma Working Group (IMWG) with available FISH studies between 01/01/2015 to 04/01/2021 in a single institution [22]. Thirty-four subjects with chromosome 1q gain or 1q amplification were identified in NDMM patients. All baseline characteristics and clinical data were extracted from the electronic medical records. This study was approved by Institutional Review Board of Tufts Medical Center.
FISH studies
We used the FISH data at the time of initial diagnosis for all NDMM patients. FISH studies were performed on CD138 + selected cells, which were obtained from fresh bone marrow aspirate specimens using a magnetic bead positive selection system (EasySep, Stemcell Technologies). Cocktails of probes were used for 1p32.3 and 1q21 (CDKNDC, CKS18 duplications/deletion, MetaSystems), the centromeres of chromosomes 9 and 15 (D9Z3 and D15Z4, Cytocell), 13q14.3 (D13S1477, D13S319, D13S25 with 13qter MetaSystems), immunoglobin H (IGH) in 14q32 (IGH break apart, MetaSystems) and 17p13.1 (TP53 with NF1, MetaSystems). We also conducted additional FISH tests to identify the partner locus of the IGH translocation under the laboratory reflex testing policy using probes for the t(4;14) (FGFR3 and IGH, dual fusion, Cytocell), the t(11;14) (CCND1 and IGH, dual fusion, Cytocell), the t(14;16) (IGH and MAF, dual fusion, Cytocell), and the t(14;20) (IGH and MAFB, dual fusion, Cytocell). One hundred interphase nuclei were examined for each probe to quantify the size of the involved clone.
Variables
Age was described both as a continuous variable and a categorical variable with a cutoff value of 65 years. Race was classified as non-Hispanic White, non-Hispanic Black, Hispanic, and Asian. Baseline International Staging System (ISS) stage, isotypes including type of immunoglobin heavy and light chains, presence of lytic bone lesions and extramedullary disease (EMD) were treated as categorical variables. Baseline creatinine and monoclonal protein-spike level were described as continuous variables. Elevated serum lactate dehydrogenase (LDH) level was defined as above 220 IU/L. Bone marrow plasma cell percentage (BMPC%) was categorized at the level of 60% (< 60% vs ≥ 60%). Chromosome 1q (CKS18) copies were divided into three different groups: more than three copies (defined as chromosome 1q amplification), three copies (defined as chromosome 1q gain), and two copies (defined as relative chromosome 1q gain due to co-occurrence of deletion of chromosome 1p) [13]. Moreover, clone size of the 1q + was categorized into two groups based on percentage of involved plasma cells (< 20% and ≥ 20%) as this cutoff level was recommended by European Myeloma Network for deletions and numerical molecular cytogenetic aberrations, and a further study indicated that 20% was an optimal cutoff for predicting outcomes [23, 24]. Additional cytogenetic alterations included deletion 13q (del 13q), del 17p, t(4;14), t(11;14), IGH abnormalities (complex IGH rearrangement or IGH loss), and hyperdiploidy. We also collected data on therapeutic modalities such as the use of ASCT as well as bortezomib, lenalidomide, and daratumumab-based therapies.
Statistical analysis
Descriptive statistical analyses were conducted to summarize the patient characteristics, treatment regimens, and disease responses according to the IMWG response criteria [25]. With death as primary event, overall survival (OS) was defined as the time from discovery of 1q + to death. Progression-free survival (PFS) was defined as the time from discovery of 1q + to first progression/relapse or death, whichever occurred first. Those who remained alive, without disease progression at the time of last follow-up or who were lost to follow-up, were censored in this study. Kaplan–Meier method was used to estimate the distributions of survival time. Differences in survival distributions between two groups were compared by log-rank tests. Results were considered to be significant if two-sided P-value was less than or equal to 0.05. All the statistical analyses were performed using R software (version 3.6.2; www.r-project.org).
Results
All thirty-four subjects were different without duplicate count, and all had 1q + detected at the time of initial diagnosis of MM. Baseline patient characteristics are summarized in Table 1. The median age of our patient population was 68 years (range 39–86), 20 (58.8%) subjects were over 65 years old, and 23 (67.6%) patients were men. The majority was non-Hispanic White (70.6%), followed by non-Hispanic Black (14.7%), Asian (11.8%), and Hispanic (2.9%). The median M-spike was 2.8 g/dL. Approximately half of the patients had BMPC% ≥ 60% at the time of diagnosis. The majority of patients had ISS stage II (39.3%) or stage III (42.9%). More than half of the subjects (66.7%) had ≥ 20% 1q + clonal plasma cells, 10 (29.4%) had chromosome 1q copy number more than three, and 12 (35.3%) had co-occurrence of 1p deletion. In addition to 1q + , most patients had concurrent del 13q (67.6%) and hyperdiploidy (64.7%). Notably, none of our patients had concurrent t(4;14). The best hematologic response to plasma-cell directed therapies during the disease course was a complete response in 23.8%, very good partial response in 38.1%, partial response in 23.8%, and disease progression in 14.3%.
At the time of this study analysis, 31 patients were still alive. Nine patients had disease progression after the discovery of 1q + . The estimated median OS for the 34 subjects was not reached (NR) (95% confidence interval [95% CI], NR-NR), and the estimated median PFS was NR (95% CI: 20.9 months, NR).
Several clinical factors were included in the log-rank tests to investigate the impact of baseline characteristics on survival data. It was found that elevated LDH is significantly associated with inferior OS (NR vs NR, P = 0.04) (Fig. 1), but not PFS (20.9 months vs NR, P = 0.4). Increased percentage of bone marrow plasma cell infiltration (≥ 60%) strongly portended to shorter PFS (20.9 months vs NR, P = 0.01) (Fig. 2), and shorter OS (NR vs NR, P = 0.06) as well. When evaluating the impact of number of copies of CKS18 on survival, it was found that the presence of more than three copies of 1q + was significantly associated with both shorter OS (NR vs NR, P = 0.01) and PFS (9.47 months vs NR, P = 0.01) when compared to those with only three copies of 1q + (Fig. 3). The presence of EMD at diagnosis was significantly associated with shorter PFS (5.92 months vs NR) and additionally tended to have worse OS (9.55 months vs NR), though the results are from few patients (only two patients had EMD in our sample). Log-rank tests by other variables including age, gender, baseline ISS stage, monoclonal protein isotype, and presence of lytic bone lesions did not reach any statistical significances. Of note, patients with 1p deletion vs those without 1p deletion showed comparable OS (NR vs NR, P = 0.3) and PFS (NR vs NR, P = 0.5). Clone size of 1q + was also found to have impact on neither OS (NR vs NR, P = 0.8) nor PFS (11.0 months vs NR, P = 0.2) when comparing patients of involved plasma cells ≥ 20% with those < 20%.
Kaplan–Meier analysis on overall survival (A) and progression-free survival (B) in newly diagnosed multiple myeloma patients harboring chromosome 1q gain/amplification with different chromosome 1q CKS18 copies. Orange line shows samples with three copies (or chromosome 1q gain); blue line shows samples with more than three copies (or chromosome 1q amplification)
The impact of other concurrent chromosomal abnormalities on survivals in patients with 1q + was also investigated (See Table 2), and carrying additional chromosomal abnormalities like del 13q, del 17p, t(11;14), hyperdiploidy, and IGH abnormalities did not show any significant influence on survival.
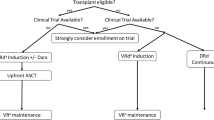
To analyze the effects of treatment regimens in this population, log-rank tests were conducted (Table 3). The administration of lenalidomide-based treatment was found to prolong OS (NR vs NR, P = 0.03). The use of upfront ASCT, daratumumab-based treatment, and bortezomib-based treatment was found to be not significantly associated with a different OS or PFS, compared with patients who did not receive the treatments above. When stratifying for age in log-rank tests, the results remained similar. The significant impact of lenalidomide-based treatment on OS remained robust (P = 0.02). No further multivariable cox regression was done in this study due to small sample size.
Discussion
In this retrospective study, we examined the real-world outcome data of patients with NDMM harboring 1q + in the era of immunotherapy. To our knowledge, this is the one of the first few studies to examine outcomes in this specific patient cohort in the era of monoclonal antibodies which are now widely used in both the newly diagnosed and relapsed, upfront setting. We found that the use of lenalidomide was the only agent which provided an overall survival benefit in this particular subgroup of myeloma patients. We did not find a significantly favorable effect of daratumumab in current study by log-rank tests only.
A recent large study of newly diagnosed patients with MM from Mayo clinic showed that 1q + was associated with significantly shorter median OS (5.3 years vs 8.8 years) compared with those without 1q + in all treatment groups which included proteasome inhibitors, immunomodulatory drugs, and combination of these two. Of note, this study did not look at outcomes with respect to the use of monoclonal antibodies [16]. Du and his team reported that the median PFS and OS in MM patients with 1q + , treated with novel therapies including thalidomide and bortezomib, were 23.1 months and 40.0 months, respectively [26]. For those with newly diagnosed MM harboring 1q + who were administered bortezomib-based or lenalidomide-based therapy followed by ASCT, a previous study reported a median PFS of 2.1 years (95% CI: 1.2 years, NR) and a median OS of 4.4 years (95% CI: 2.9 years, NR) [14]. In this report, the median PFS after the identification of 1q + was not reached (95% CI: 20.9 months, NR), and the median OS was not reached as well (95% CI: NR, NR). The relatively longer OS and PFS that we reported may reflect the widespread use of novel therapies and monoclonal antibody regimens in this study.
LDH is well known to have an independent prognostic value on disease survival, treatment response, and disease aggressiveness in both NDMM and relapsed and refractory multiple myeloma (RRMM) patients [27, 28]. The present study confirmed the inferior impact of elevated LDH on OS in NDMM patients with 1q + . A recent study revealed the prognostic impact of BMPC% in NDMM patients, indicating that BMPC% being more than 60% is predictive for worse PFS and OS [29]. Our study substantiated this conclusion in NDMM patients with 1q + by finding that BMPC% ≥ 60% was associated with worse PFS and marginally significantly associated with worse OS.
The prognostic impact of 1q copy number and clone size has been investigated in the past. A study from Neben et al. showed that the presence of greater than three copies of 1q + was associated with remarkably shorter PFS and OS, compared with those with normal copy number, while the presence of three copies 1q + only had a marginal negative effect on outcomes [30]. Another study from Schmidt et al. found that NDMM patients with 4 or more copies of 1q + had significantly worse PFS compared to those without 1q + , whereas those with three copies had similar PFS [13]. A different study showed that copy numbers of 1q + tended to rise at relapse, whereas the 5-year event-free survival and OS between patients with more than three copies and those with only three copies were comparable in relapsed patients [31]. A study by An et al. reported similar results, demonstrating that copy number variation did not have additional prognostic impact [32]. This was corroborated by Abdallah’s study showing no significant difference in OS between patients with 3 copies gain and those with 1q amplification (> 3 copies) [16]. The results from our study were in agreement with the conclusions from the former two studies, suggesting significant outcome differences in NDMM patients between patients with three copies of 1q + and those with more than three copies with respect to both OS and PFS. While using 20% as the cutoff value to predict prognosis in our study, we found different 1q + clone size carried no additional prognostic value in 1q + NDMM patients in terms of both OS and PFS. This result is consistent with Abdallah’s finding [16].
There were only two patients with EMD out of our 34 subjects detected at diagnosis. In terms of EMD distribution, one had central nervous system involvement and another had liver involvement. A previous study had demonstrated higher incidence of del (17p) (31% vs 13%) and 1q + (55% vs 32%) when comparing patients with and without EMD according to a small sample [33]. In the present study, we found that the presence of EMD had significant impact on PFS and tended to have worse OS in NDMM patients with 1q + . The result is consistent with the conclusions from other studies that indicated EMD was associated with poor prognosis in MM patients compared to those lacking this clinical feature, though our result is limited to small sample size [34, 35].
The roles of concurrent cytogenetic alterations in patients with 1q + have been explored in several studies. It was reported that 1q + had close associations with several genetic features including del (13q) and t(4;14) [26, 36]. Our study showed frequent co-occurrence of 1q + with del (13q) but not t(4:14). Furthermore, the co-existence of other cytogenetic abnormalities including 1p deletion status in our study showed no further impact on prognosis.
By performing log-rank tests, we further investigated the impact of different therapeutic strategies in MM patients harboring 1q + . A previous study showed that 1q + conferred an inferior prognosis in patients treated with chemotherapy incorporating bortezomib [32]. Total therapy 3 trial noted patients with 1q + had early progression and worse overall survival when being treated with bortezomib compared to those without 1q + , and demonstrated that it was likely related to the overexpression of PSMD4, a non-ATPase subunit of the proteosomal 19S regulator on chromosome 1q21, whose level is highly correlated to CKS1B copy numbers [37]. The results from the present study regarding bortezomib are consistent with above data, suggesting that population with 1q + may confer resistance to bortezomib. Varma’s team performed propensity score-matched analysis to compare MM patients with 1q + with/without 1p- and patients with normal FISH panel undergoing ASCT and demonstrated that the former group had shorter PFS (26.5 months vs 38.8 months); however, this median PFS of 26.5 months is longer than historically reported median PFS of 19 months for 1q + NDMM patients of whom not every patient received ASCT [20]. Varma’s study indicated that ASCT improved the outcomes of 1q + with/without 1p- though this approach did not fully overcome the negative impact of this cytogenetic change. A CIBMTR analysis evaluated the prognostic outcomes in patients underwent ASCT from 2008 to 2012, and found those with 1q + abnormalities had comparable outcomes with those without high-risk abnormalities [38]. Our study did not prove the prognostic benefit of ASCT, but it might be limited by the small number. There were only 6 patients who had ASCT, which was likely a result of patients’ eligibility and preference in the setting of advanced age, performance status, and baseline comorbidities. There has been no study examining the impact of lenalidomide alone on this population, but a prior study showed that 1q + was associated with earlier progression with lenalidomide, bortezomib, and dexamethasone compared to a control group [13]. When performing log-rank tests in our study, the lenalidomide-based treatment was found to prolong OS. The crude protective effects of lenalidomide could be partially explained by the healthier status of patients, given lenalidomide is used more frequently in patients with better renal function. A further log-rank test stratified by age confirmed the favorable impact of lenalidomide-based treatment on OS, though further adjustments for other covariates were unable to be done in this study due to relatively small sample size.
Daratumumab, a human monoclonal antibody targeting CD38, has affected durable responses and survival benefits in MM patients of all risk groups generally, especially in relapsed or refractory patients [39,40,41,42]. A systematic review and meta-analysis by Giri et al. suggested that adding daratumumab to backbone regimens in both newly diagnosed or relapsed/refractory high-risk MM patients (defined as the presence of t(4;14), t(4;16), or del (17p)) was associated with improved PFS [43]. However, the studies regarding daratumumab’s impact on patients with 1q + are rare. One study so far investigated outcomes of refractory MM patients who all received daratumumab and reported that both the gene expression profiling (GEP) 70 score and the status of 1q + were independently associated with worse PFS; patient with high GEP 70 score had significantly inferior OS, but 1q + (N = 36) showed only a trend for poor OS (N = 45) [44]. However, this cited study did not include newly diagnosed patients. Most importantly, it only answered the prognostic differences between patients with and without 1q + , but did not evaluate the real efficacy of daratumumab in those patients with 1q + specifically. Another study ever investigating the role of CD38 monoclonal antibody was an abstract retrospectively analyzing the data from ICARIA-MM study and phase 1b TCD 14,079 (NCT02283775), which found that compared to pomalidomide-dexamethasone (Pd) alone, addition of isatuximab to Pd in RRMM patients with 1q + led to significantly improved PFS; however, patients with 1q + still had inferior overall response rate and PFS compared to those without 1q + [45]. Of note, this is a study which only investigated RRMM patients as well. Our study is the very first study exploring the prognostic role of daratumumab in NDMM patients with 1q + , and we did not demonstrate its efficacy in this population. The resistance to CD38 monoclonal antibodies in patients harboring 1q + may be related to the JAK-STAT pathway, though further data are needed. [46, 47]
A strength of our study is its complete data set with no missing information in a real-world setting. It is an important study creatively exploring the baseline characteristics and the impact of novel agents, especially monoclonal antibodies, uniquely in this population of NDMM patients with 1q + . Prior studies usually focused on intergroup differences by comparing cohort with 1q + and those without 1q + [13, 14, 20]; however, this study revealed intragroup outcomes based on different predictors. The primary limitations of this study are the relatively small sample size and its single-center retrospective nature. In addition, we were not able to perform multivariable cox regression analysis due to its small cohort nature; thus, the confounding effect from confounders like age, ISS, and/or renal function still existed, though our stratified log-rank tests adjusted the confounding effect of age and showed similar results. Moreover, we only included bortezomib, lenalidomide, and daratumumab use in this study, but not other proteasome inhibitors such as ixazomib/carfilzomib, or other immunomodulators such as thalidomide/pomalidomide, or other monoclonal antibodies like elotuzumab/isatuximab. Future studies with larger sample sizes and more extensive data to look at the impact of different therapies on this important patient population are required.
Conclusions
In summary, we investigated the NDMM patients harboring chromosome 1q gain/amplification and evaluated the outcomes according to different clinical characteristics, additional cytogenetic abnormalities, and treatment regimens. We investigated the impact of novel therapies and monoclonal antibodies including daratumumab in this unique population and demonstrated the potential prognostic benefit of lenalidomide. These results may help to guide the therapeutic strategies and choices in this population in the future. Larger sample size and prospective clinical trials are warranted to confirm these results, further explore the role of monoclonal antibodies, and improve the outcomes of MM patients with this cytogenetic abnormality.
Data availability
The data of this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Kazandjian D (2016) Multiple myeloma epidemiology and survival: a unique malignancy. Semin Oncol 43(6):676–681
National Cancer Institute S, Epidemiology, and End Results Program (2021) (Cited 2021 September 5). Cancer Stat facts: myleoma. Available from: https://seer.cancer.gov/statfacts/html/mulmy.html
Palumbo A, Anderson K (2011) Multiple myeloma. N Engl J Med 364(11):1046–1060
Kristinsson SY, Anderson WF, Landgren O (2014) Improved long-term survival in multiple myeloma up to the age of 80 years. Leukemia 28(6):1346–1348
Bergsagel PL, Mateos MV, Gutierrez NC, Rajkumar SV, San Miguel JF (2013) Improving overall survival and overcoming adverse prognosis in the treatment of cytogenetically high-risk multiple myeloma. Blood 121(6):884–892
Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L et al (2015) Revised international staging system for multiple myeloma: a report from international myeloma working group. J Clin Oncol 33(26):2863–2869
Walker BA, Leone PE, Chiecchio L, Dickens NJ, Jenner MW, Boyd KD et al (2010) A compendium of myeloma-associated chromosomal copy number abnormalities and their prognostic value. Blood 116(15):e56-65
Saxe D, Seo EJ, Bergeron MB, Han JY (2019) Recent advances in cytogenetic characterization of multiple myeloma. Int J Lab Hematol 41(1):5–14
Dewald GW, Kyle RA, Hicks GA, Greipp PR (1985) The clinical significance of cytogenetic studies in 100 patients with multiple myeloma, plasma cell leukemia, or amyloidosis. Blood 66(2):380–390
Ganoth D, Bornstein G, Ko TK, Larsen B, Tyers M, Pagano M et al (2001) The cell-cycle regulatory protein Cks1 is required for SCF(Skp2)-mediated ubiquitinylation of p27. Nat Cell Biol 3(3):321–324
Spruck C, Strohmaier H, Watson M, Smith APL, Ryan A, Krek W et al (2001) A CDK-independent function of mammalian Cks1. Mol Cell 7(3):639–650
Avet-Loiseau H, Attal M, Campion L, Caillot D, Hulin C, Marit G et al (2012) Long-term analysis of the IFM 99 trials for myeloma: cytogenetic abnormalities [t(4;14), del(17p), 1q gains] play a major role in defining long-term survival. J Clin Oncol 30(16):1949–1952
Schmidt TM, Barwick BG, Joseph N, Heffner LT, Hofmeister CC, Bernal L et al (2019) Gain of Chromosome 1q is associated with early progression in multiple myeloma patients treated with lenalidomide, bortezomib, and dexamethasone. Blood Cancer J 9(12):94
Shah GL, Landau H, Londono D, Devlin SM, Kosuri S, Lesokhin AM et al (2017) Gain of chromosome 1q portends worse prognosis in multiple myeloma despite novel agent-based induction regimens and autologous transplantation. Leuk Lymphoma 58(8):1823–1831
Rajkumar SV, Kumar S (2016) Multiple myeloma: diagnosis and treatment. Mayo Clin Proc 91(1):101–119
Abdallah N, Greipp P, Kapoor P, Gertz MA, Dispenzieri A, Baughn LB et al (2020) Clinical characteristics and treatment outcomes of newly diagnosed multiple myeloma with chromosome 1q abnormalities. Blood Adv 4(15):3509–3519
Leone PE, Walker BA, Jenner MW, Chiecchio L, Dagrada G, Protheroe RK et al (2008) Deletions of CDKN2C in multiple myeloma: biological and clinical implications. Clin Cancer Res 14(19):6033–6041
Hebraud B, Leleu X, Lauwers-Cances V, Roussel M, Caillot D, Marit G et al (2014) Deletion of the 1p32 region is a major independent prognostic factor in young patients with myeloma: the IFM experience on 1195 patients. Leukemia 28(3):675–679
Boyd KD, Ross FM, Walker BA, Wardell CP, Tapper WJ, Chiecchio L, et al. Mapping of chromosome 1p deletions in myeloma identifies FAM46C at 1p12 and CDKN2C at 1p32.3 as being genes in regions associated with adverse survival. Clin Cancer Res. 2011;17(24):7776–84.
Varma A, Sui D, Milton DR, Tang G, Saini N, Hasan O et al (2020) Outcome of multiple myeloma with chromosome 1q gain and 1p deletion after autologous hematopoietic stem cell transplantation: propensity score matched analysis. Biol Blood Marrow Transplant 26(4):665–671
Chen D, Zhou D, Xu J, Zhou R, Ouyang J, Chen B (2019) Prognostic value of 1q21 gain in multiple myeloma. Clin Lymphoma Myeloma Leuk 19(3):e159–e164
Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos M-V et al (2014) International myeloma working group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 15(12):e538–e548
An G, Li Z, Tai YT, Acharya C, Li Q, Qin X et al (2015) The impact of clone size on the prognostic value of chromosome aberrations by fluorescence in situ hybridization in multiple myeloma. Clin Cancer Res 21(9):2148–2156
Ross FM, Avet-Loiseau H, Ameye G, Gutierrez NC, Liebisch P, O’Connor S et al (2012) Report from the European myeloma network on interphase FISH in multiple myeloma and related disorders. Haematologica 97(8):1272–1277
Kumar S, Paiva B, Anderson KC, Durie B, Landgren O, Moreau P et al (2016) International myeloma working group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol 17(8):e328–e346
Du C, Mao X, Xu Y, Yan Y, Yuan C, Du X et al (2020) 1q21 gain but not t(4;14) indicates inferior outcomes in multiple myeloma treated with bortezomib. Leuk Lymphoma 61(5):1201–1210
Terpos E, Katodritou E, Roussou M, Pouli A, Michalis E, Delimpasi S et al (2010) High serum lactate dehydrogenase adds prognostic value to the international myeloma staging system even in the era of novel agents. Eur J Haematol 85(2):114–119
Dimopoulos MA, Kastritis E, Christoulas D, Migkou M, Gavriatopoulou M, Gkotzamanidou M et al (2010) Treatment of patients with relapsed/refractory multiple myeloma with lenalidomide and dexamethasone with or without bortezomib: prospective evaluation of the impact of cytogenetic abnormalities and of previous therapies. Leukemia 24(10):1769–1778
Al Saleh AS, Parmar HV, Visram A, Muchtar E, Buadi FK, Go RS et al (2020) Increased bone marrow plasma-cell percentage predicts outcomes in newly diagnosed multiple myeloma patients. Clin Lymphoma Myeloma Leuk 20(9):596–601
Neben K, Lokhorst HM, Jauch A, Bertsch U, Hielscher T, van der Holt B et al (2012) Administration of bortezomib before and after autologous stem cell transplantation improves outcome in multiple myeloma patients with deletion 17p. Blood 119(4):940–948
Hanamura I, Stewart JP, Huang Y, Zhan F, Santra M, Sawyer JR et al (2006) Frequent gain of chromosome band 1q21 in plasma-cell dyscrasias detected by fluorescence in situ hybridization: incidence increases from MGUS to relapsed myeloma and is related to prognosis and disease progression following tandem stem-cell transplantation. Blood 108(5):1724–1732
An G, Xu Y, Shi L, Shizhen Z, Deng S, Xie Z et al (2014) Chromosome 1q21 gains confer inferior outcomes in multiple myeloma treated with bortezomib but copy number variation and percentage of plasma cells involved have no additional prognostic value. Haematologica 99(2):353–359
Qu X, Chen L, Qiu H, Lu H, Wu H, Qiu H, et al. Extramedullary manifestation in multiple myeloma bears high incidence of poor cytogenetic aberration and novel agents resistance. Biomed Res Int. 2015;2015:787809.
Usmani SZ, Heuck C, Mitchell A, Szymonifka J, Nair B, Hoering A et al (2012) Extramedullary disease portends poor prognosis in multiple myeloma and is over-represented in high-risk disease even in the era of novel agents. Haematologica 97(11):1761–1767
Landau H, Pandit-Taskar N, Hassoun H, Cohen A, Lesokhin A, Lendvai N et al (2012) Bortezomib, liposomal doxorubicin and dexamethasone followed by thalidomide and dexamethasone is an effective treatment for patients with newly diagnosed multiple myeloma with Internatinal Staging System stage II or III, or extramedullary disease. Leuk Lymphoma 53(2):275–281
Shah V, Sherborne AL, Walker BA, Johnson DC, Boyle EM, Ellis S et al (2018) Prediction of outcome in newly diagnosed myeloma: a meta-analysis of the molecular profiles of 1905 trial patients. Leukemia 32(1):102–110
Shaughnessy JD Jr, Qu P, Usmani S, Heuck CJ, Zhang Q, Zhou Y et al (2011) Pharmacogenomics of bortezomib test-dosing identifies hyperexpression of proteasome genes, especially PSMD4, as novel high-risk feature in myeloma treated with Total Therapy 3. Blood 118(13):3512–3524
Scott EC, Hari P, Sharma M, Le-Rademacher J, Huang J, Vogl D et al (2016) Post-transplant outcomes in high-risk compared with non-high-risk multiple myeloma: a CIBMTR analysis. Biol Blood Marrow Transplant 22(10):1893–1899
Chari A, Suvannasankha A, Fay JW, Arnulf B, Kaufman JL, Ifthikharuddin JJ et al (2017) Daratumumab plus pomalidomide and dexamethasone in relapsed and/or refractory multiple myeloma. Blood 130(8):974–981
Usmani SZ, Weiss BM, Plesner T, Bahlis NJ, Belch A, Lonial S et al (2016) Clinical efficacy of daratumumab monotherapy in patients with heavily pretreated relapsed or refractory multiple myeloma. Blood 128(1):37–44
Mateos MV, Spencer A, Nooka AK, Pour L, Weisel K, Cavo M et al (2020) Daratumumab-based regimens are highly effective and well tolerated in relapsed or refractory multiple myeloma regardless of patient age: subgroup analysis of the phase 3 CASTOR and POLLUX studies. Haematologica 105(2):468–477
Facon T, Kumar S, Plesner T, Orlowski RZ, Moreau P, Bahlis N et al (2019) Daratumumab plus Lenalidomide and Dexamethasone for Untreated Myeloma. N Engl J Med 380(22):2104–2115
Giri S, Grimshaw A, Bal S, Godby K, Kharel P, Djulbegovic B, et al. Evaluation of daratumumab for the treatment of multiple myeloma in patients with high-risk cytogenetic factors: a systematic review and meta-analysis. JAMA Oncol. 2020.
Mohan M, Weinhold N, Schinke C, Thanedrarajan S, Rasche L, Sawyer JR et al (2020) Daratumumab in high-risk relapsed/refractory multiple myeloma patients: adverse effect of chromosome 1q21 gain/amplification and GEP70 status on outcome. Br J Haematol 189(1):67–71
Paul Richardson SH, Thierry Facon, Kwee Yong. Isatuximab plus pomalidomide and dexamethasone in relapsed/refractory multiple myeloma patients with 1q21 gain: insights from phase 1 and phase 3 studies. Abstract and Poster EP1017 EHA 2020 June 12, 2020.
Schmidt TM, Fonseca R, Usmani SZ (2021) Chromosome 1q21 abnormalities in multiple myeloma. Blood Cancer J 11(4):83
Ogiya D, Liu J, Ohguchi H, Kurata K, Samur MK, Tai YT et al (2020) The JAK-STAT pathway regulates CD38 on myeloma cells in the bone marrow microenvironment: therapeutic implications. Blood 136(20):2334–2345
Acknowledgements
Thanks to the staff of the Cytogenetics Laboratory at Tufts Medical Center for their contributions to this work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Xiao Hu, Cherng-Horng Wu, Janet M. Cowan, and Cindy Varga. First draft of the manuscript was written by Xiao Hu, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. The respective Institutional Review Boards at Tufts Medical Center approved this study. As this was a retrospective study, informed consent could not be obtained from all patients included in the study.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest/Competing interests
All authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hu, X., Wu, CH., Cowan, J.M. et al. Outcomes of patients with multiple myeloma harboring chromosome 1q gain/amplification in the era of modern therapy. Ann Hematol 101, 369–378 (2022). https://doi.org/10.1007/s00277-021-04704-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-021-04704-8