Abstract
Bone marrow WT1 mRNA levels assessed by the ELN method are useful to establish prognostic correlations in myeloid malignancies treated with chemotherapy or hematopoietic stem cell transplantation (HCT). Those patients with WT1 levels below ten copies have a good outcome. However, some of these patients relapse. To further characterize this group of cases, we applied a new and sensitive digital (ddPCR) WT1 method. A consecutive series of 49 patients with treated myeloid malignancies and with an ELN WT1 quantitation of < 10 copies were included in the study. All cases (47 AML and 2 MDS) have received intensive chemotherapy or HCT. One to four micrograms of total RNA were retrotranscribed to obtain ≥ 10,000 ABL1 copies using the ELN protocol. Only those cases with a good quality cDNA were used in the ddPCR WT1 test. The ddPCR Gene Expression WT1 Assay of Bio-Rad© was used to perform the PCR amplification, and the microdroplets were quantified in the Bio-Rad’s QX200 droplet reader. Eighteen patients showed a negative WT1 ddPCR assay (0 copies/μl), whereas 31 cases were positive (results ranged from 1 to 15.2 copies/μl). Survival analysis showed statistically significant differences in terms of OS between both groups, 83 ± 8% vs. 46 ± 9% (p = 0.024). A statistically significant correlation was also found between ddPCRWT1 results and CD123+ cell number detected by flow cytometry (p = 0.024). Larger series of patients tested with the current ddPCRWT1 method will solve whether it could be used to stratify patients with myeloid malignancies achieving deep WT1 molecular response (< 10 copies).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Minimal or measurable residual disease (MRD) has been used to predict relapse in patients with myeloid malignancies [1,2,3,4]. Chimeric fusion genes (PML-RARa, RUNX1-RUNX1T1, CBFb-MYH11) or small insertions (NPM1 mutations) analyzed by sensitive real-time PCR methods are the most widely used targets based on its reliability, sensitivity, and specificity. However, a large proportion of AML cases lack such genetic alterations, and alternative methods should be used. Standardized multiparametric flow cytometry and sensitive strategies of next-generation sequencing (NGS) are gaining acceptance in most laboratories. Despite the potential advantages of these techniques, other less complex alternatives based on PCR methods are also employed. WT1 has been used as a surrogate marker of the leukemic clone size based on the overexpression of WT1 mRNA in immature myeloid progenitors [5,6,7,8]. WT1 quantitation has been standardized, and it could be assayed both in peripheral blood and bone marrow [9]. It also could provide meaningful results in cases with low bone marrow cellularity in which multiparametric flow cytometry may be suboptimal. It has been shown that WT1 mRNA levels are increased in the outgrowing subclone irrespective of the genetic background. Furthermore, this technique is simple, cheap, and rapid, and it does not require specialized software or technical expertise. It has been suggested that the best results are obtained with the peripheral blood given the very low number of WT1 expressing cells in this sample. However, about 10% of AML and other myeloid malignancies show no increases in WT1 mRNA levels, and when compared face to face with core-binding factor gene rearrangements or NPM1 mutation assays, this technique showed less sensitivity. Based on these limiting facts, some experts claim that WT1 overexpression should only be used as MRD marker in the absence of other more suitable targets [3]. The accurate detection of WT1 expression ranges from 10 to 1,000,000 copies based on the plasmid levels used to perform the quantitation. In an earlier report using the ELN standardized method, we have shown that those AML cases with less than ten copies at the end of the chemotherapy showed an improved outcome [10, 11]. Thus, in this range of values (< 10 copies), plasmid-based quantification is far from being precise. To further analyze those cases, we applied a new digital PCR (ddPCRWT1) method, and we tried to establish clinical correlations.
Patients and methods
Patients’ characteristics and basic molecular methods
Bone marrow samples (49 patients) at the end of the chemotherapy treatment or after HCT were obtained in each participating institution and sent to the CETLAM repository center at the Hospital de la Santa Creu i Sant Pau in Barcelona for immunophenotype and molecular analyses. Samples at diagnosis were also tested for mutations in the NPM1, FLT3, CEBPA, KMT2A, and WT1 genes using well-established protocols [4, 10]. For WT1 and ABL1 quantification, the ELN method was used as previously reported [10, 11]. In cases with NPM1 mutation, a quantitative real-time PCR method was employed to assess the molecular remission [12]. Most patients were treated in accordance with the AML CETLAM 2003 trial (32 patients). Two samples were obtained from pediatric patients with AML at the end of the chemotherapy. Three samples were from patients with a previous HCT. The remaining 12 samples corresponded to AML patients enrolled in different CETLAM trials (Table 1).
Digital PCR of WT1
Mononuclear cells were separated using Lymphoprep (Alere Technologies, Oslo, Norway). The total RNA was extracted with AllPrep DNA/RNA kit (Qiagen, Hilden, Germany) and Trizol reagent (Invitrogen, Carlsbad, USA) according to the manufacturer’s instructions and quantified by spectrophotometry and input amount was optimized for retrotranscription. In all cases, enough RNA was retrotranscribed to obtain a minimum ABL1 of 104 copies, in a total reaction volume of 20 μl. RNA, Random Hex 15 μM, and dNTP (1 mM) were incubated for 65 °C 5 min and quickly chilled on ice. Collection of the content of the tube was done by brief centrifugation, and then we added 1× First-Strand Buffer, 10 mM DTT, Rnasin 20 units, and 200 units of M-MLV RT enzyme (Life Technologies, Carlsbad, USA), and incubated at 37 °C for 2 min, 10 min at 25 °C, 50 min at 37 °C, 15 min at 70 °C, and finally at 4 °C.
After the cDNA synthesis, an aliquot was employed to test the ABL1 copy number using the standard Biomed protocol. The ddPCR mix was prepared as follows: 10 μl of 2× ddPCR Supermix for Probes (Bio-Rad Laboratories, Inc., USA), 1 μl of 20× ddPCR Assay WT1Hsa (HEX) #10031255 (Bio-Rad Laboratories, Inc., USA), 4 μl of DNAase-free water, and 5 μl of cDNA. The 20-μl droplet digital PCR (ddPCR) reaction mixture was then loaded into a sample well of a DG8 Cartridge for QX200 Droplet Generator (Bio-Rad Laboratories, Inc., USA) followed by 70 μl of Droplet Generation oil for probes into the oil wells, according to the QX200 Droplet Generator instruction manual.
The generated droplets were transferred into a clean 96-well plate. The plate was heat-sealed with pierceable foil seal (# 1814040 Bio-Rad) from PX1 PCR Plate Sealer (Bio-Rad Laboratories, Inc., USA) and then placed on a thermal cycler and amplified to the endpoint. Thermal-cycling conditions are indicated in Suppl table 1.
After PCR, the 96-well PCR plate was loaded on QX200 Droplet Reader (Bio-Rad Laboratories, Inc., USA), which reads the droplets from each well of the plate. Analysis of the ddPCR data was performed with QuantaSoft analysis software version 1.7.4 that accompanied the QX200 droplet reader.
Flow cytometry immunophenotyping
Combinations of four monoclonal antibodies were used to assess the MRD in myeloid neoplasms (CD15/CD34/HLA-Dr/CD45, CD15/CD117/CD45/HLA-Dr, CD34/CD123/HLA-Dr/CD45, CD34/CD33/CD19/CD45) using the clones and fluorochromes previously reported with minor modifications [12]. The percentage of viable CD45+ cells was recorded in every case. A two-step protocol on viable cellularity was employed to assess the most immature myeloid populations and a minimum of 200,000 events were analyzed to establish the percentage of positive cells for each antigen. All the analyses were performed by the same person (JN) in a FACS-Canto flow cytometer (Becton Dickinson, CA) and using the PAINT-A-GATE software (BD).
Statistical methods
Characteristics between groups were compared using the χ2 test and Fisher’s exact test for categorical variables and the Mann-Whitney U test for continuous variables. The median value of continuous variables was used to dichotomize them for prognostic analyses. Overall survival (OS) was measured, from the date of enrollment until the date of death, and was estimated by the Kaplan-Meier method; comparisons between groups were performed by the log-rank test. The threshold values were established by selecting the most accurate values by a nonparametric receiver-operating characteristics (ROC) analysis, taking into account the maximum ratio sensitivity-specificity. The endpoint for the threshold was death and relapse. This approach was applied following the REMARK guidelines [13].
The statistical packages used were the IBM® SPSS® Statistics (version 25.0, USA) and the Rversion 3.3.2 from The R Foundation for Statistical Computing.
Results
ddPCRWT1
One microgram of total RNA was retrotranscribed following the recommendations of the ELN group to perform the molecular diagnostic of the most common chimeric gene rearrangements. A quality requirement for the preanalytical phase was established: ABL1 copy number should be greater than 10,000 copies. Previous experiments performed in cases with lower values showed a lack of reproducibility, i.e., repeated experiments showed marked discrepancies in the number of positive droplets (data not shown). For those cases failing to achieve this requirement, we increased the amount of total RNA in the retrotranscription reaction until four micrograms. The ddPCR volume mix was run following the recommendations of the manufacturer, and the hands-on time was 6 h. The experiments were performed in duplicate on two different days. All samples showed adequate droplet counts (> 11,000) (Table 2). Blank controls (H2O) did not show positive droplets. We established two groups of patients: those without WT1 copies in the ddPCR assay (negative) and the second group of cases with any positive result (positive). The quartile distribution of all the series is depicted in Fig. 1 and Table 2. The interpretation of ddPCR is very easy: a negative case shows no positive droplets, whereas positive cases showed any level of positivity (provided that more than 11,000 droplets have been rightly included in the analysis).
Representative dot plots of ddPCRWT1. Top left: no positive droplets were detected (0 copies/ml, negative). Top right and bottom left: increasing numbers of positive droplets were detected in these cases (1.5 and 15.2 copies/μl, respectively). All two samples had WT1 ELN values of less than ten copies but were considered as positives in the ddPCRWT1 assay. Bottom right, ddPCRWT1 dot plot diagram in a case with more than ten copies in the WT1 ELN test and ddPCRWT1 strong positivity (262 copies/μl). Positive droplets in green and negative droplets in gray
When we investigated the overall survival of both groups, and despite the heterogeneity and the low number of cases included in this series, we detected a statistically significant advantage for those cases being ddPCRWT1 negative (p = 0.024) (Fig. 2). This improved outcome did not reach statistic meaning for leukemia-free survival and cumulative incidence of relapse.
In 10 out of 11 cases with type A-B-D NPM1 mutations, the copy number was below three copies, whereas one case (UPN31) showed 20 copies (Table 1).
Correlation between bone marrow ddPCRWT1 results with myeloid cell populations assessed by flow cytometry
We investigated the number of viable CD45+ cells and immature cell compartments in all the cases (CD34+, CD117+, CD123+). There were no differences in the percentage of CD45+ cases in both groups. In negative ddPCRWT1 samples, the percentage of immature cells was lower than in ddPCRWT1+ patients. This difference reached statistical significance for CD123+ cells, suggesting that the number of stem cells in this group of patients (neoplastic or normal) is lower than in ddPCRWT1+ cases (Table 3).
Discussion
In this work, we applied a ddPCRWT1 method, which makes full use of widely available reagents, and we also established the technical conditions of amplification and results interpretation. As a quality requirement for each retrotranscription, the product was tested using the European Leukemia Net method of real-time PCR amplification for the ABL1 gene, which was used as a control. Only those samples with more than 10,000 ABL1 copies were employed in the ddPCRWT1 assay. Given that some of those samples came from other centers, showed poor cellularity, or are obtained in the post-HCT phase, we retrotranscribed more than 1 μg as needed to reach the 10,000 ABL1 threshold (until 4 μg). The limited number of available samples with deep WT1 molecular response (< 10 copies) and the technical constraints for the amplification procedure restricted our study to only 49 cases.
Using this approach and despite all the above-mentioned limitations, our preliminary results showed that ddPCRWT1 might be informative to establish prognosis stratifications further. Irrespective of the diagnosis or the previous therapy, patients with a negative ddPCRWT1 result showed a statistically significant advantage in terms of overall survival. We also detected a positive correlation between ddPCRWT1 status and CD123+ cell number, suggesting that WT1 levels may be linked to the size of the leukemic stem cell compartment. Given the low number of cases analyzed, we were not able to detect statistically significant associations with the number of positive cells for other immature markers (CD34, CD117). Samples from patients with the lowest quantity of CD123+ cells are those with a negative ddPPCRWT1 result. CD123 (IL3 receptor ⍺ chain) is expressed in immature precursors with stem cell behavior and it is also a marker present in most AML and B cell lineage ALL, being constantly present in the leukemic stem cell fraction. Based on these findings, immunotherapeutic strategies to deplete CD123+ cells are currently being investigated to treat AML [14,15,16,17].
WT1 is expressed in a small population of myeloid committed immature progenitors. In some experimental models, this population could be the target of the myeloid transforming events [18]. Ye et al. [19] have shown that myeloid differentiation is required for acquiring a leukemia stem cell (LSC) phenotype and AML initiation and that blocking GMP formation abrogates leukemic transformation. This critical step in myeloid cell development could be indirectly identified by raised WT1 levels and CD123 expression. Real-time PCR findings in one NPM1 mutated case (UPN31, 20 copies) showing negative digital WT1 results may suggest that both measurements may provide complementary information in selected cases.
Digital PCR techniques rely on the partition of the PCR mix in compartments (droplets in the most commonly used formats, although they could also be obtained in solid cells) to determine the concentration of the target sequence without a need of a calibration curve. Efficient partitioning methods allow obtaining homogeneous, numerous, and of the same size droplets. Most clinical instruments show a volume variation of the droplets of less than 3%. Each partition could contain either a few or no target sequences. After the PCR reaction, a fraction of positive partitions are used to quantify the concentration of the target sequence using Poisson’s statistics. It has been assumed that digital PCR is less prone to inhibition than real-time PCR [20,21,22]. Digital PCR has been employed to detect point mutations in plasma DNA from patients with solid neoplasms [23] and to perform MRD studies in core-binding factor AML with KIT mutations. Despite the promising results obtained in such studies, some uncertainties remain and we should be cautious to wrongly qualify dropout samples, which in our study means a negative ddPCRWT1 result. The increased number of partitions (more than 11,000 in our design) could increase the change of PCR inhibition. Furthermore, single-molecule amplification is often less efficient than amplification with a higher number of molecules, and the readout may be, in some instances, dependent on the source of nucleic acid purification (bone marrow in our series). Bearing all these factors in mind, we tried to establish a simple and reproducible method of ddPCRWT1. We focused on those samples in which the precision of conventional real-time PCR is low. In recent times, other groups have tried a similar approach.
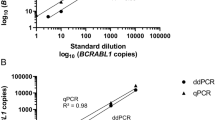
Waterhouse et al. [24] used a digital PCR platform (Bio-Rad) to assess the chimerism status and other molecular abnormalities (NPM1 mutations, core-binding factor chimeric fusions, and WT1 expression levels) in bone marrow samples obtained after HCT. Fourteen patients showed raised levels of WT1 and mixed chimerism, which was predictive of clinical relapse. However, the method of digital amplification of WT1 is not currently available. Koizumi et al. [25] analyzed 40 samples from 32 patients using the Quantstudio 3D Digital PCR System. These authors established a comparison between the WT1 levels obtained using this method and a real-time PCR technique. The correlation between both methods was strong (r = 0.99). The mean ABL1 expression for the real-time PCR group was 15,238 copies and 5947 copies for the digital PCR samples. However, in this paper, WT1 expression was not detected in 20 healthy volunteers suggesting that the sensitivity of both methods was low.
In contrast with these reports, we provide a simple and reproducible protocol that could be applied to samples previously tested for real-time PCR using the ELN method. In more than one-third of cases (18/49) analyzed, the digital PCR was negative (0 copies/ml). We also can assume that our limit of detection was higher than our limit of the blank. The validity of this approach could be supported by the survival advantage.
In conclusion, the digital WT1 PCR method could be easily applied to the study of myeloid malignancies. The main limitation, as in conventional real-time approaches, is the obtention of good quality material in heavily treated patients. The application of this technique to cases with myeloid malignancies achieving WT1 deep molecular response (ELN levels below ten copies) may be helpful in establishing prognostic predictions. The interpretation of negative ddPCRWT1 results needs to be fully elucidated in future prospective trials. This measurement could be combined with the assessment of the number CD123+ by flow cytometry, specific chimeric transcripts, or insertion mutations (NPM1). This approach may be potentially used to define a high-quality remission status after chemotherapy and/or HCT in myeloid neoplasms. The analysis of the efficacy of CD123-targeted therapies by ddPCRWT1 also warrants future studies.
References
Maurillo L, Buccisano F, Del Principe MI et al (2008) Toward optimization of postremission therapy for residual disease-positive patients with acute myeloid leukemia. J Clin Oncol 26:4944–4951
Buccisano F, Maurillo L, Del Principe MI et al (2012) Prognostic and therapeutic implications of minimal residual disease detection in acute myeloid leukemia. Blood 119:332–341
Schuurhuis GJ, Heuser M, Freeman S et al (2018) Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD Working Party. Blood 13:1275–1291
Perea G, Lasa A, Aventin A et al (2006) Prognostic value of minimal residual disease (MRD) in acute myeloid leukemia (AML) with favorable cytogenetics [t(8;21) and inv(16)]. Leukemia 20:87–94
Hohenstein P, Hastie ND (2006) The many facets of the Wilms’ tumour gene, WT1. Hum Mol Genet 15(2):R196–R201
Huff V (2011) Wilms’ tumours: about tumour suppressor genes, an oncogene and a chameleon gene. Nat Rev Cancer 11:111–121
Chau YY, Hastie ND (2012) The role of Wt1 in regulating mesenchyme in cancer, development, and tissue homeostasis. Trends Genet 28:515–524
Ostergaard M, Olesen LH, Hasle H et al (2004) WT1 gene expression: an excellent tool for monitoring minimal residual disease in 70% of acute myeloid leukaemia patients - results from a single-centre study. Br J Haematol 125:590–600
Cilloni D, Renneville A, Hermitte F, Hills RK, Daly S, Jovanovic JV, Gottardi E, Fava M, Schnittger S, Weiss T, Izzo B, Nomdedeu J, van der Heijden A, van der Reijden B, Jansen JH, van der Velden V, Ommen H, Preudhomme C, Saglio G, Grimwade D (2009) Real-time quantitative polymerase chain reaction detection of minimal residual disease by standardized WT1 assay to enhance risk stratification in acute myeloid leukemia: a European LeukemiaNet study. J Clin Oncol 27:5195–5201
Nomdedéu JF, Hoyos M, Carricondo M, Bussaglia E, Estivill C, Esteve J, Tormo M, Duarte R, Salamero O, de Llano MP, García A, Bargay J, Heras I, Martí-Tutusaus JM, Llorente A, Ribera JM, Gallardo D, Aventin A, Brunet S, Sierra J, CETLAM Group (2013) Bone marrow WT1 levels at diagnosis, post-induction and post-intensification in adult de novo AML. Leukemia 27:2157–2164
Nomdedéu JF, Esquirol A, Carricondo M, Pratcorona M, Hoyos M, Garrido A, Rubio M, Bussaglia E, García-Cadenas I, Estivill C, Brunet S, Martino R, Sierra J (2018) Bone marrow WT1 levels in allogeneic hematopoietic stem cell transplantation for acute myelogenous leukemia and myelodysplasia: clinically relevant time points and 100 copies threshold value. Biol Blood Marrow Transplant 24:55–63
Nomdedeu J, Bussaglia E, Villamor N et al (2010) Immunophenotype of acute myeloid leukemia with NPM mutations: prognostic impact of the leukemic compartment size. Leuk Res 35:163–168
Mallett S, Timmer A, Sauerbrei W et al (2009) Reporting of prognostic studies of tumour markers: a review of published articles in relation to REMARK guidelines. Br J Cancer 102:173–180
Jordan CT, Upchurch D, Szilvassy SJ et al (2000) The interleukin-3 receptor alpha chain is a unique marker for human acute myelogenous leukemia stem cells. Leukemia 14:1777–1784
Muñoz L, Nomdedéu JF, López O, Carnicer MJ, Bellido M, Aventín A, Brunet S, Sierra J (2001) Interleukin-3 receptor alpha chain (CD123) is widely expressed in hematologic malignancies. Haematologica 86:1261–1269
Stevens BM, Khan N, D’Alessandro A et al (2018) Characterization and targeting of malignant stem cells in patients with advanced myelodysplastic syndromes. Nat Commun 12(9):3694
Lin J, Lee EM, Ramshaw H et al (2009) Monoclonal antibody-mediated targeting of CD123, IL-3 receptor a chain, eliminates acute myeloid leukemic stem cells. Cell Stem Cell 5:31–42
Hosen N, Shirakata T, Nishida S, Yanagihara M, Tsuboi A, Kawakami M, Oji Y, Oka Y, Okabe M, Tan B, Sugiyama H, Weissman IL (2007) The Wilms’ tumor gene WT1-GFP knock-in mouse reveals the dynamic regulation of WT1 expression in normal and leukemic hematopoiesis. Leukemia 21:1783–1791
Ye M, Zhang H, Yang H, Koche R, Staber PB, Cusan M, Levantini E, Welner RS, Bach CS, Zhang J, Krivtsov AV, Armstrong SA, Tenen DG (2015) Hematopoietic differentiation is required for initiation of acute myeloid leukemia. Cell Stem Cell 17:611–623
Pinheiro L, Emslie KR (2018) Basics concepts and validation of digital PCR measurements. In: Karlin-Neumann G, Bizouarn F (eds) Digital PCR: Methods and Protocols, Methods in Molecular Biology, vol. 1768. Springer Nature
Quan PL, Sauzade M, Brouzes E (2018) dPCR: a technology review. Sensors 18:1271
Chen Y, George AM, Olsson E, Saal LH (2018) Identification and use of personalized genomic markers for monitoring circulating tumor DNA. In: Karlin-Neumann G, Bizouarn F (eds) Digital PCR: Methods and Protocols, Methods in Molecular Biology,vol. 1768. Springer Nature
Ono Y, Sugitani A, Karasaki H, Ogata M et al (2017) An improved digital polymerase chain reaction protocol to capture low-copy KRAS mutations in plasma cell-free DNA by resolving ‘subsampling’ issues. Mol Oncol 11:1448–1458
Waterhouse M, Pfeifer D, Duque-Afonso J et al (2019) Droplet digital PCR for the simultaneous analysis of minimal residual disease and hematopoietic chimerism after allogeneic cell transplantation. Clin Chem Lab Med 57:641–647
Koizumi Y, Furuya D, Endo T, Asanuma K, Yanagihara N, Takahashi S (2018) Quantification of Wilms´ tumor 1 mRNA by digital polymerase chain reaction. Int J Hematol 107:230–234
Funding
The following grants funded this work: Fundación Mutua Madrileña 08/FMMA; PI13/2729, PI16/094 from the Instituto de Salud Carlos III, Ministerio de Economía y Competitividad, Spain; 2014-SGR-383, 2017-SGR-1395, PERIS SLT 002/16/0043 from Plà de Recerca de Catalunya; and a grant from Fundacion Josep Carreras and “Obra Social La Caixa” Barcelona Spain.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Josep Nomdedeu (JN) received honoraria from Novartis. The rest of the authors (EB, MP, MC, LS, MAR, AM, AB, IB, JE, MA, CT, MT, AG, FV, XO, CP, JB, SB, and JS) had nothing to disclose.
Ethical approval
All procedures were following the ethical standards of the Hospital de Sant Pau research committee, followed the SEHH recommendations, and were in accordance with the 1964 Helsinki declaration and its later amendments.
Statement of informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 8 kb)
Rights and permissions
About this article
Cite this article
Bussaglia, E., Pratcorona, M., Carricondo, M. et al. Application of a digital PCR method for WT1 to myeloid neoplasms in CR and deep ELN WT1 molecular response (< 10 copies). Ann Hematol 99, 765–772 (2020). https://doi.org/10.1007/s00277-020-03910-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-020-03910-0