Abstract
The outcome of high-risk myelodysplastic syndrome (MDS) patients treated with 5-azacitidine (5-AZA) in the real-life setting remains largely unknown. We evaluated 110 MDS patients (IPSS intermediate 2/high) treated outside of clinical trials at a single institution between September 2003 and January 2017. Median duration of therapy was 9.5 cycles. The overall survival (OS) of the whole cohort was 66.1% at 1 year and 38.3% at 2 years. No differences in terms of OS were observed with regard to gender (p = 0.622) and age at baseline (< 65 years, 65–75, and > 75 years, p = 0.075). According to the IPSS-R, the very high-risk group had an inferior 2-year OS (17%) compared with intermediate-group patients (64%, p < 0.001). Transfusion independency at baseline was identified as a favorable prognostic factor on 1-year (66.8%) and 2-year OS (43.4%) (p < 0.001). After four cycles, the persistence of bone marrow blasts > 10% identified patients with a worse outcome, with a 2-year OS of 9.4% (p = 0.002). The occurrence of an infection during the first four cycles impacted on the 2-year OS (31.6% vs 58.3% in patients without infections, p = 0.032). Patients receiving at least 24 cycles of the drug have a 5-year OS of 38.2%. This analysis allowed to identify features at baseline or during treatment with 5-AZA associated with a different 2-year OS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myelodysplastic syndromes (MDS) are a group of clonal hematologic disorders that mainly affect elderly people and are characterized by cytopenias, ineffective hematopoiesis, and an increased risk of evolution into an acute myeloid leukemia (AML) [1, 2]. The prognosis of individuals with MDS is very heterogeneous and accurately estimated by universally accepted prognostic scoring indexes such as IPSS, IPSS-R, and WPSS, which are able to stratify different risk groups in terms of overall survival (OS) and risk of AML evolution [3,4,5]. 5-Azacitidine (5-AZA) has changed the therapeutic approach to intermediate 2/high IPSS risk MDS by improving the outcome of patients, even in the absence of a complete response. 5-AZA is a cytidine analogue, which inhibits a group of enzymes called DNA methyltransferases (DNMTs) and subsequently leads to the demethylation of the cytosine residues in the promoter-associated CpG islands. The hypomethylation and subsequent reversal of the transcriptional inhibition of important tumor suppressor and DNA repair genes is believed to represent the main mechanism of action [6]. Approximately 80–90% of 5-AZA is processed through the entire sequence and incorporated into RNA. This ultimately disrupts mRNA and protein metabolism, leading to apoptosis. A smaller fraction (10–20%) of AZA is converted to decitabine triphosphate: in this form, it is incorporated into DNA and covalently binds DNA methyltransferases (DNMTs), thereby inhibiting the activity of these proteins [7]. Real-life experiences in MDS patients treated with 5-AZA have reported contrasting results compared with the sponsored AZA001 randomized study [8,9,10]. Aim of our analysis was to identify the clinicobiologic features at baseline and during treatment associated with a 2-year OS and progression-free survival (PFS) in a consecutive cohort of MDS patients treated with 5-AZA outside of clinical trials.
Patients and methods
We retrospectively analyzed 110 consecutive MDS patients (IPSS intermediate 2/high risk) treated outside of clinical trials at a single institution with 5-AZA between September 2003 and January 2017. Diagnosis was carried according to the WHO 2016 criteria [11]. Baseline clinical and biologic features were collected in a specific database, including cytogenetics, morphologic diagnosis, IPSS, WPSS, IPSS-R stratification, and comorbidities. 5-AZA was administered at a dose of 75 mg/m2 according to the 5 + 2 + 2 schedule every 28 days. Responses were evaluated according to the IWG 2006 criteria [12]. Continued variables were expressed as median, whereas categorical variables as frequencies. OS and PFS (considering only leukemic progression) curves were generated using the Kaplan-Meier method, and the log-rank tests were used to compare subgroups of patients. None of the patients reported received investigative therapies in case or relapse or nonresponse. A significant p value was expressed as < 0.05. All statistical analyses were performed using the “R Project for Statistical Computing” version 3.5.0 software.
Results
Characteristics of patients
The baseline demographic, clinical, and treatment characteristics were recorded and are summarized in Table 1. The median age was 70 years (range 38–85). A male predominance was observed (male/female 66%/34%). Only 1 patient received another treatment before 5-AZA (lenalidomide), whereas 61 (55.4%) did not receive any treatment, 21 patients (19.1%) received vitaminic support, and 8 patients (7.4%) erythroid-stimulating agents. Thirty-five patients (31.8%) had no transfusion requirement. According to the IPSS score stratification, 97 patients (88.2%) were diagnosed as intermediate 2 and 13 (11.8%) as high risk. According to the IPSS-R, 4 patients (3.6%) were stratified as low, 18 (16.4%) as intermediate, 46 (41.8%) as high, and 42 (38.2%) as very high risk. Cytogenetic aberrations were stratified according to the IPSS risk score, and 75 patients (68.3%) were diagnosed as good risk, 15 (13.6%) as intermediate, and 20 (18.1%) as poor risk. The median dose of 5-AZA received was 135 mg/day (range 105–150) after a median time from diagnosis of 2.3 months (range 0.1–119). Median duration of therapy was 9.5 cycles (range 4–77) with a median time on treatment of 8.5 months (range 1–86.7).
Efficacy and outcome
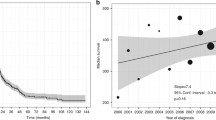
According to the IWG criteria applied after the fourth cycle, 54.5% of patients achieved a complete response (CR), 14.2% a partial response (PR) (including also 4 patients with an erythroid hematologic improvement), and 22.4% a stable disease (SD) for an overall response rate of 68.7% (Fig. 1). The OS of the whole cohort was 66.1% (95% CI 57.2–76.4) at 1 year and 38.3% (95% CI 29.4–49.9) at 2 years. PFS at 1 year was 56.7% (95% CI 47.7–67.5) and at 2 years 30.9% (95% CI 22.3–41.6) (Fig. 2). No differences in terms of OS were observed with respect to gender (p = 0.622) or age at baseline (< 65 years, 65–75, and > 75 years, p = 0.075) or different percentage of bone marrow blast cells at baseline (p = 0.867) (Suppl. Fig. 1a). A slight difference was observed in PFS according to gender (male vs female, p = 0.045), but no differences were observed for the different age ranges (p = 0.734) or different cutoffs of blast cells at baseline (p = 0.611) (Suppl. Fig. 1b). According to the IPSS-R, 22 (20%), 46 (42.8%), and 42 (38.2%) patients were classified as intermediate, high, and very high-risk patients, respectively. The very high-risk group had a significantly inferior 2-year OS (17%) compared with intermediate-group patients (64%, p < 0.001). IPSS-R identified also a 30% probability of an acute leukemia evolution in very high-risk patients (p = 0.051) (Suppl. Fig. 2). No significant differences were observed according to the IPSS stratification in terms of 2-year OS (intermediate 42% vs high-risk 22%, p = 0.253) and PFS (p = 0.826) (Suppl. Fig. 3). The 2-year OS according to the IPSS cytogenetic stratification showed a significantly worse outcome for patients carrying high-risk aberrations (p = 0.037) (Suppl. Fig. 4). According to the IWG response, the 2-year OS was 68% in patients who obtained a CR/PR, 20% in patients with SD, and 16% in patients with progression disease (PD)/failure (p < 0.001). Patients with a stable response after four cycles had an increased PFS, similar to that of patients in CR/PR, and separated sharply from that of patients who failed treatment (p = 0.001) (Fig. 3). Transfusion independence at baseline was identified as a favorable prognostic factor on 1-year (66.8%) and 2-year OS (43.4%) compared with patients with transfusion dependency (36.4% and 22.2% if they required 1 unit/month or more than 1 unit at baseline at 2 years, p < 0.001). We also evaluated the value of transfusion dependency during treatment, and again patients who required transfusion had a lower OS (< 0.001) (Suppl. Fig. 5). We also stratified patients according to the MDS-CI and found no differences in OS between patients stratified in low (53 patients or 48.1%), intermediate (38 patients or 34.5%), and high (19 patients or 17.4%) risk (p = 0.064) (Suppl. Fig. 6). After four cycles, the persistence of bone marrow blasts > 10% identified patients with a worse outcome, with a 2-year OS of 9.4% compared with 60.3% for patients with 0–5% blasts and 44.7% for patients with 5–10% blasts (p = 0.002) (Suppl. Fig. 7). The occurrence of an infection during the first four cycles had also an impact on the 2-year OS (31.6% vs 58.3% in patients without infections, p = 0.032) (Suppl. Fig. 8). Moreover, a subgroup analysis was conducted in 21 patients treated long term that received at least 24 cycles of 5-AZA. Median duration of therapy was 34 cycles (range 24–77) (Suppl. Table 1). Most patients were classified as IPSS intermediate 2 risk (85.7%) with a good cytogenetic risk (81%), with no transfusion requirement. The overall response rate was 85.7% (CR 71.4% and PR 14.3%). OS and PFS were, respectively, 38.2% (95% CI 19.9–73.3) and 58.4% (95% CI 19.9–73.3) at 5 years and 12.7% (95% CI 2.3–71.7) and 38.9% (95% CI 15–100) at 7 years (Suppl. Fig. 9).
Discussion
In view of the contrasting results obtained in MDS patients treated with AZA outside of clinical trials, we hereby report the results obtained at our center in a series of MDS patients treated with AZA in a real-life setting. We observed a 2-year OS of 38.8%, inferior to that reported in the AZA-001 randomized trial (50.8%, 24.5 months), reflecting a possible patient selection in clinical trials. Comparing our results with similar experiences reported in the real-life setting, we observed analogous outcomes. The GFM (Group Francophone des Myelodysplasies) analyzed 282 high-risk MDS patients treated with AZA and described, after a median of 6 cycles of treatment, an OS of 13.5 months, with rates of CR and PR, respectively, of 38% and 9% [13]. In this study, the transfusion dependence during treatment, a poor performance status, and the IPSS cytogenetic risk were indicated as poor prognostic factors for OS [13]. Bernal et al. [14] reported the GESDM (Grupo Espanol de Sindromes Mielodisplasicos) experience in 251 patients, showing a median OS of 13.4 months. The Spanish group proposed a different explanation that could help to clarify the apparent discrepancies between the results of their retrospective comparative study and the AZA-MDS-001 clinical trial. First, the incidence of IPSS poor-risk cytogenetic was higher in this report than that in the AZA-MDS-001 trial (40% vs 28%, respectively). Furthermore, most of the chromosome 7 abnormalities were found in the context of a complex karyotype. Another factor that could have influenced the results of real-life experiences has been the inclusion of patients with therapy-related MDS and the median number of AZA cycles administered that was inferior to that reported in the AZA001 clinical trial (6 vs 9). Another experience was reported by the Canadian registry on a large cohort of 1101 patients affected by high-risk MDS and low blast count AML, treated in Ontario, that showed an OS of 11.6 months and rates of CR and PR of 49% and 31%, respectively [15]. A large analysis collected through SEER-Medicare linked database on 2025 patients treated with hypomethylating agents (AZA and decitabine) showed a median OS of 15 months, substantially shorter if compared with AZA-001 trial and of 12 months if limited to RAEB patients [16].
In our study, no differences in terms of OS were observed with regard to gender, age, and bone marrow blast percentage at baseline. Comorbidities have an important role at baseline to tailor treatment strategies also in MDS: a prognostic score, the MDS-CI, which has been recently validated in order to provide information on OS and on risk of nonleukemic mortality, identified three different risk groups. Very few analyses have been performed on the impact of the comorbidity burden in patients treated with AZA. We applied the MDS-CI score on our patient population and did not observe differences in terms of OS, results in line with those reported by the Rete Ematologica Lombarda (REL), that indeed included also patients with 20–30% of bone marrow blasts [17], confirming that AZA treatment appears feasible even in the presence of well-known comorbidities recognized as influencing the OS in MDS patients. In our study, a better outcome has been observed in the good and intermediate cytogenetic risk groups according to IPSS. The adverse OS of patients with poor-risk karyotype suggests that these patients may have a clinical response to AZA, but they still have a poor prognosis and probably require an intensified treatment with combinations of drugs. Both our results and previously published data by the French group [10] show that the relatively favorable outcome of patients with 7/del7q cytogenetic aberrations is restricted to patients without a complex karyotype, suggesting, whenever possible, AZA as a bridge-to-transplant in this setting.
Unlike the real-life experiences reported in the literature, we also explored the weight of transfusion dependency at baseline. We identified that transfusion independency at baseline was a favorable prognostic factor on 1- (66.8%) and 2-year OS (43.4%) compared with 36.4% and 22.2% in patients who required 1 unit/month or more than 1 unit/month at baseline (p < 0.001).
With regard to response evaluated according to the IWG criteria, the 2-year OS was 68% in patients who obtained a CR/PR, 20% in patients with SD, and 16% in patients with PD/failure (p < 0.001). Indeed, a SD seems to correlate with prolonged PFS, suggesting that continuing therapy in this category of patients may prolong the evolution to acute leukemia.
An intermediate bone marrow blast determination appears in our series to bear prognostic implications. We suggest bone marrow evaluation after four cycles and propose a cutoff of 10% of bone marrow blasts to identify patients with a good long-term outcome after four cycles of treatment: the 2-year OS was 9.4% in patients with > 10% blasts compared with 60.3% for patients with 0–5% blasts and 44.7% for patients with 5–10% blasts (p = 0.002). This information has so far not been reported, and only the GFM group [10] showed a possible poor outcome associated with 15% blasts in the peripheral blood. No bone marrow data were provided. We believe that our proposed cutoff may help physicians to stratify patients after four cycles with a poor prognosis and candidate them, whenever possible, to a more intensive therapy, including eventually an allogeneic transplantation or combination approaches.
In our study, the occurrence of one infective episode during the first four cycles negatively impacted on the 2-year OS (31.6% vs 58.3% in patients without, p = 0.032). A German retrospective cohort of patients treated with AZA was reported, and infectious complications were more frequently reported during the first 3 cycles, but preexisting comorbidities and IPSS-R stratification seem to have no influences as compared indeed with age and achieved hematologic responses [18]. In another study on 184 patients treated with AZA, unfavorable cytogenetics and low platelet and neutrophil count (less than 0.5 × 109/l) seem to be predictive of infection risk. The authors suggested to evaluate the risk before each cycle and a prophylaxis only for unfavorable cytogenetics at baseline [19]. In our experience, even patients without high-risk cytogenetics at baseline experienced infective episodes during the fourth cycle; therefore, in the absence of randomized comparison, we cannot suggest antiinfective prophylaxis.
Lastly, we conducted a subanalysis on 21 long-term-treated patients who received at least 24 cycles of AZA. With a median of 34 cycles of treatment, the overall response rate was 85.7% (CR 71.4% and PR 14.3%). OS and PFS were respectively 38.2% and 58.4% at 5 years and 12.7% and 38.9% at 7 years. It appears that a good karyotype and the absence of transfusion requirement at baseline are associated with a long-term treatment possibility. A limitation of our study is in the retrospective nature and the absence of other genetic information, such as molecular characteristics at baseline. About molecular characterization, other contrasting results were reported by Kuendgen et al.: they showed that AZA efficacy is independent of molecular and clinical features at baseline in 128 patients and suggested that other results reported in literature demonstrating the increased or decreased effect of the drug by molecular stratification are inconsistent and did not translate into improved survival [20].
In conclusion, our data confirm that AZA treatment in an unselected MDS population is well tolerated. Owing to the lack of definitive results that can define molecular features associated with good/poor clinical outcome in MDS patients treated with AZA, this real-life analysis allowed to define clinicohematologic features at baseline and during treatment with AZA associated with clinical response and survival and to identify patients who require treatment intensification. Further real-life studies aimed at validating these features are warranted.
References
Tefferi A, Vardiman JW (2009) Myelodysplastic syndromes. N Engl J Med 361:1872–1885
Montalban-Bravo G, Garcia-Manero G (2018) Myelodysplastic syndromes: 2018 update on diagnosis, risk-stratification and management. Am J Hematol 93:129–147
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, Sanz M, Vallespi T, Hamblin T, Oscier D, Ohyashiki K, Toyama K, Aul C, Mufti G, Bennett J (1997) International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 89:2079–2088
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, Bennett JM, Bowen D, Fenaux P, Dreyfus F, Kantarjian H, Kuendgen A, Levis A, Malcovati L, Cazzola M, Cermak J, Fonatsch C, le Beau MM, Slovak ML, Krieger O, Luebbert M, Maciejewski J, Magalhaes SMM, Miyazaki Y, Pfeilstocker M, Sekeres M, Sperr WR, Stauder R, Tauro S, Valent P, Vallespi T, van de Loosdrecht AA, Germing U, Haase D (2012) Revised international prognostic scoring system for myelodysplastic syndromes. Blood 120(12):2454–2465
Malcovati L, Germing U, Kuendgen A, Della Porta MG, Pascutto C, Invernizzi R, Giagounidis A, Hildebrandt B, Bernasconi P, Knipp S, Strupp C, Lazzarino M, Aul C, Cazzola M (2007) Time-dependent prognostic scoring system for predicting survival and leukemic evolution inmyelodysplastic syndromes. J Clin Oncol 25(23):3503–3510
Silvermann LR (2004) DNA methyltransferase inhibitors in myelodysplastic syndrome. Best Pract Res Clin Haematol 17(4):585–594
Aimiuwu J, Wang H, Chen P, Xie Z, Wang J, Liu S, Klisovic R, Mims A, Blum W, Marcucci G, Chan KK (2012 31) RNA-dependent inhibition of ribonucleotide reductase is a major pathway for 5-azacytidine activity in acute myeloid leukemia. Blood. 119(22):5229–5238
Beguin Y, Selleslag D, Meers S, Graux C, Bries G, Deeren D, Vrelust I, Ravoet C, Theunissen K, Voelter V, Potier H, Trullemans F, Noens L, Mineur P (2015) Safety and efficacy of azacytidine in Belgian patients with high-risk myelodysplastic syndromes, acute myeloid leukaemia, or chronic myelomonocytic leukaemia: results of a real-life, non-interventional post-marketing survey. Acta Clin Belg 70(1):34–43
Voso MT, Niscola P, Piciocchi A et al (2016) Standard dose and prolonged administration of azacitidine are associated with improved efficacy in a real-world group of patients with myelodysplastic syndrome or low blast count acute myeloid leukemia. Eur J Haematol 96(4):344–351
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A, Schoch R, Gattermann N, Sanz G, List A, Gore SD, Seymour JF, Bennett JM, Byrd J, Backstrom J, Zimmerman L, McKenzie D, Beach C, Silverman LR, International Vidaza High-Risk MDS Survival Study Group (2009) International Vidaza High-Risk MDS Survival Study Group Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol 10(3):223–232
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, le Beau MM, Bloomfield CD, Cazzola M, Vardiman JW (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 127:2391–2405
Cheson BD, Bennett JM, Kantarjian H, Pinto A, Schiffer CA, Nimer SD, Löwenberg B, Beran M, de Witte TM, Stone RM, Mittelman M, Sanz GF, Wijermans PW, Gore S, Greenberg PL, World Health Organization(WHO) international working group (2000) Report of an international working group to standardize response criteria for myelodysplastic syndromes. Blood. 96:3671–3674
Itzykson R, Thepot S, Quesnel B (2011) Prognostic factors for response and overall survival in 282 patients with higher-risk myelodysplastic syndromes treated with azacitidine. Blood 117(2):403–411
Bernal T, Martínez-Camblor P, Sánchez-García J et al (2015) Effectiveness of azacitidine in unselected high-risk myelodysplastic syndromes: results from the Spanish registry. Leukemia 29(9):1875–1881
Mozessohn L, Cheung MC, Fallahpour S, Gill T, Maloul A, Zhang L, Lau O, Buckstein R (2018) Azacitidine in the ‘real-world’: an evaluation of 1101 higher-risk myelodysplastic syndrome/low blast count acute myeloid leukaemia patients in Ontario, Canada. Br J Haematol 181(6):803–815
Zeidan AM, Davidoff AJ, Long JB, Hu X, Wang R, Ma X, Gross CP, Abel GA, Huntington SF, Podoltsev NA, Hajime U, Prebet T, Gore SD (2016) Comparative clinical effectiveness of azacitidine versus decitabine in older patients with myelodysplastic syndromes. Br J Haematol 175:829–840
Molteni A, Riva M, Borin L, Bernardi M, Pelizzari AM, Freyrie A, Porta MD, Nichelatti M, Ravano E, Quaresmini G, Mariotti J, Caramazza D, Ubezio M, Guarco S, Gigli F, Greco R, Cairoli R, Morra E (2016) The influence of disease and comorbidity risk assessment on the survival of MDS and oligoblastic AML patients treated with 5-azacitidine: a retrospective analysis in ten centers of the “Rete Ematologica Lombarda”. Leuk Res 42:21–27
Schuck A, Goette MC, Neukirchen J, Kuendgen A, Gattermann N, Schroeder T, Kobbe G, Germing U, Haas R (2017) A retrospective study evaluating the impact of infectious complications during azacitidine treatment. Ann Hematol 96:1097–1104
Merkel D, Filanovsky K, Gafter-Gvili A, Vidal L, Aviv A, Gatt ME, Silbershatz I, Herishanu Y, Arad A, Tadmor T, Dally N, Nemets A, Rouvio O, Ronson A, Herzog-Tzarfati K, Akria L, Braester A, Hellmann I, Yeganeh S, Nagler A, Leiba R, Mittelman M, Ofran Y (2013) Predicting infections in high-risk patients with myelodysplastic syndrome/acute myeloid leukemia treated with azacitidine: a retrospective multicentre study. Am J Hematol 88:130–134
Kuendgen A, Muller-Thomas C, Lauseker M et al (2018) Efficacy of azacitidine is independent of molecular and clinical characteristics-an analysis of 128 patients with myelodysplastic syndromes or acute myeloid leukemia and a review of the literature. Oncotarget 9:27882–22789
Author information
Authors and Affiliations
Contributions
MB designed the study and wrote and revised the manuscript; ES wrote the manuscript; MM collected the data; DAF and FE analyzed the data; LR, RL, GC, and MMa followed the patients; RF critically revised the paper and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
MB received honoraria by Novartis, Pfizer, and Incyte; FE received personal fees from Bristol Myers Squibb, Incyte, Orsenyx, and Amgen. All other authors declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 692 kb)
Rights and permissions
About this article
Cite this article
Scalzulli, E., Molica, M., Alunni Fegatelli, D. et al. Identification of predictive factors for overall survival at baseline and during azacitidine treatment in high-risk myelodysplastic syndrome patients treated in the clinical practice. Ann Hematol 98, 1919–1925 (2019). https://doi.org/10.1007/s00277-019-03724-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-019-03724-9