Abstract
We prospectively assessed by magnetic resonance imaging (MRI) the advantages of desferrioxamine (DFO) with respect to the absence of chelation therapy in non transfusion-dependent thalassaemia (NTDT) patients. We considered 18 patients non-chelated and 33 patients who received DFO alone between the two MRI scans. Iron overload was assessed by the T2* technique. Biventricular function parameters were quantified by cine sequences. No patient treated with DFO had cardiac iron. At baseline, only one non-chelated patient showed a pathological heart T2* value (< 20 ms) and he recovered at the follow-up. The percentage of patients who maintained a normal heart T2* value was 100% in both groups. A significant increase in the right ventricular ejection fraction was detected in DFO patients (3.48 ± 7.22%; P = 0.024). The changes in cardiac T2* values and in the biventricular function were comparable between the two groups. In patients with hepatic iron at baseline (MRI liver iron concentration (LIC) ≥ 3 mg/g/dw), the reduction in MRI LIC values was significant only in the DFO group (− 2.20 ± 4.84 mg/g/dw; P = 0.050). The decrease in MRI LIC was comparable between the groups. In conclusion, in NTDT patients, DFO therapy showed no advantage in terms of cardiac iron but its administration allowed an improvement in right ventricular function. Moreover, DFO reduced hepatic iron in patients with significant iron burden at baseline.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, there has been growing interest on chelation practice among patients with non transfusion-dependent thalassaemia (NTDT). In fact, NTDT patients, even in the absence of a stable transfusional iron, gradually accumulate iron and experience, if not treated, a progressive increase in serum ferritin levels and in liver iron concentration (LIC) [1]. The elevated LIC (above 5 mg/g dw) and iron burden these patients can reach have been associated directly and indirectly with morbidity [2]. Despite such an evidence and the consequent need of chelation therapy, very few studies have evaluated the efficacy of chelating agents in treating and preventing complications of iron overload among NTDT.
Recently, data from both THALASSA and extension studies have definitively validated the use of deferasirox (DFX) in the treatment of liver iron overload and in the normalization of iron index [3, 4]. However, while the profile of DFX in the treatment of NTDT iron overload has becoming more and more ascertained [5], the activity of the older chelator desferrioxamine (DFO) has not yet fully elucidated and relies mostly on the wide experience reached from studies performed on population with transfusion-dependent thalassaemia (TDT). Paradoxically, administration of DFO was the first therapy to be studied for the treatment of acquired hemochromatosis in patients with NTDT: the decline in ferritin levels and/or the increase in iron excretion were the main parameters evaluated [6, 7]. Recently, in a five-year long-term randomized clinical trial comparing the effectiveness of DFO vs deferiprone (DFP) in patients with thalassemia intermedia (TI), it was reported that long-term iron chelation therapy with DFO is similarly effective as DFP in terms of ferritin reduction, but no data appeared about LIC trend under both treatments [8]. Ultimately, the use of DFO for the removal of iron overload in NTDT still continues in the real life in absence of specific guidelines and dose indications and also in presence of nearly normal LIC levels.
There are no studies reporting long-term observational prospective data on the effects of DFO therapy on cardiac iron and function and liver iron in NTDT patients. The aim of this multi-center study was to assess prospectively in a large clinical setting of NTDT patients the efficacy of DFO versus no therapy over a follow-up (FU) of 18 months.
Materials and methods
Study population
The MIOT (Myocardial Iron Overload in Thalassemia) project is an Italian network constituted by 68 thalassemia and 9 validated magnetic resonance imaging (MRI) centers linked by a web-based network, configured to collect and share patients’ data [9].
Among the first 185 TI patients who performed a MRI FU study at 18 ± 3 months according to the protocol, we selected the 68 who were non transfusion dependent (32 females; mean age, 39.17 ± 10.50 years; age range, 9–67 years). Twenty-eight patients (41.2%) have never been transfused while 40 (58.8%) have received only sporadic transfusions. We excluded the remaining 117 patients regularly transfused by a mean age of 16.91 ± 16.46 years.
Eight patients changed the chelation regimen during the FU time due to clinical reasons. Eighteen patients did not receive any chelation therapy during the entire FU and 42 maintained the same chelation regimen: DFO for 33 patients, DFP for 4 patients, DFX for 3 patients, and combination DFO + DFP for 2 patients.
The study complied with the Declaration of Helsinki. All patients gave written informed consent to the protocol. The institutional review board approved this study.
Magnetic resonance imaging
MRI exams were performed using a 1.5-T scanner (GE Signa/Excite HD, Milwaukee, WI, USA). An eight-element cardiac phased-array receiver surface coil with breath holding in end expiration and ECG gating was used for signal reception.
The T2* technique was used for iron overload assessment. Its reproducibility and its transferability within the MIOT network had been previously demonstrated [10]. For the heart, a multislice multiecho T2* approach was used. Three parallel short-axis views (basal, medium, and apical) of the left ventricle (LV) were obtained at nine echo times (TEs) [11,12,13,14]. For the liver, a single mid-transverse slice was obtained at nine TEs using a T2* gradient–echo multiecho sequence [15]. T2* image analysis was performed using a custom-written, previously validated software program (HIPPO MIOT) [13]. The software provided the T2* value on each of 16 LV segments, according to the American Heart Association (AHA)/American College of Cardiology (ACC) standardized myocardial segmentation [16]. Global heart T2* value was obtained by averaging all segmental T2* values. The value of 20 ms was used as “conservative” normal value for all 16 segments and for the global T2* value [13]. For the liver, the T2* value was calculated in a large region of interest (ROI) of standard dimension, chosen in a homogeneous area of parenchyma without blood vessels [17]. As recommended [18], liver T2* values were converted into LIC values using the calibration curve introduced by Wood et al. [19]. A LIC higher than 3 mg/g dry weight indicated iron overload [20].
For the quantification of biventricular function parameters, steady-state free procession cine images were acquired during 8-s breath holds in sequential 8-mm short-axis slices (gap 0 mm) from the atrioventricular ring to the apex. Images were analyzed in a standard way [21] using MASS software (Medis, Leiden, The Netherlands). The inter-center variability for the quantification of cardiac function had been previously reported [22].
Serum ferritin estimation
The assessment of serum ferritin levels was done within 1 month from the MRI scan.
About 3 ml of patient’s blood sample was collected by a clean venepuncture. The blood was allowed to clot and was centrifuged to obtain serum samples. The ferritin was then determined by commercially available kits.
Statistical analysis
All data were analyzed using SPSS version 13.0 statistical package. Continuous variables were described as mean ± standard deviation (SD). Categorical variables were expressed as frequencies and percentages.
A receiver operating characteristic (ROC) analysis was conducted to determine the best serum ferritin cutoff for discriminating the patients with MRI LIC ≥ 5 mg/g dw (threshold for treatment initiation) and with MRI LIC ≥ 3 mg/g dw (presence of hepatic iron). The probability cutoff points for the optimal combination of sensitivity and specificity were determined by the Youden index.
For the intra-treatment and the inter-treatment comparisons, the changes between final and basal values were used for each quantitative variable. The intra-treatment comparison was performed by univariate analysis of variance (ANOVA) with repeated measures. The inter-treatment comparison for the baseline data and the changes between final and basal values was performed by independent-samples t test (normal distribution) or Wilcoxon’s signed rank test (non normal distribution).
χ2 test was performed for categorical baseline variables.
A P value < 0.05 was considered statistically significant.
Results
ROC analysis
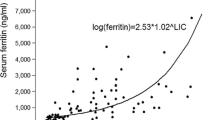
Using ROC curve analysis, a serum ferritin of 525 ng/ml was found to be the best threshold for predicting a LIC ≥ 5 mg/g dw, with an area under the curve (AUC) of 0.854 (95%CI = 0.759–0.949) (P < 0.0001) (Fig. 1a). The derived threshold corresponded to a sensitivity of 74% and to a specificity of 87%.
A serum ferritin of 468 ng/ml was found to be the best threshold for predicting a LIC ≥ 3 mg/g dw, with an AUC of 0.924 (95%CI = 0.861–0.988) (P < 0.0001) (Fig. 1b). The derived threshold corresponded to a sensitivity of 69% and to a specificity of 100%.
Characterization of patients treated with DFO or non-chelated
We focused our analysis on the 60 patients with no chelation or the same chelation regimen during the FU. However, due to numerical reasons, it was possible to evaluate the changes between baseline and FU values only for non-chelated patients and patients treated with DFO, and inter-treatment comparison was restricted to these two groups.
The mean FU was comparable between non-chelated patients and patients treated with DFO (18.89 ± 1.91 vs 18.98 ± 1.59 months; P = 0.906).
The mean administered dosage of DFO was 40.18 ± 6.29 mg/kg body weight via subcutaneous route on 3.44 ± 1.52 days/week.
The clinically and instrumentally relevant baseline findings in the two groups are summarized in Table 1. Five patients (two non-chelated and three treated with DFO) did not complete the first MRI scan for claustrophobia reasons, making impossible to evaluate their biventricular function. The two groups were comparable for all parameters.
Intra-treatment changes and inter-treatment comparison
Changes of MRI parameters between the two MRI scans in non-chelated patients are shown in Table 2A. No change in global heart T2* values was detected. All patients remained free of cardiac iron also at the FU MRI. Biventricular function parameters remained almost unchanged. There was a little nonsignificant increase in MRI LIC values. Two patients with a baseline MRI LIC < 3 mg/g dw became pathological at the FU MRI (patient 1 moved from 2.12 to 9.27 mg/g dw; patient 2 moved from 2.12 to 3.63 mg/g dw) while one patient with hepatic iron at the baseline MRI (MRI LIC = 3.26 mg/g dw) showed no iron at the FU MRI (MRI LIC = 2.90 mg/g dw).
Changes of MRI parameters between the two MRI scans in DFO patients are shown in Table 2B. No change in global heart T2* values was detected. All 32 patients without significant MIO at the baseline MRI maintained the same status at the FU MRI and the single patients with baseline significant MIO (global heart T2* = 15.23 ms) improved at the FU MRI (global heart T2* = 26.93 ms). Among the biventricular function parameters, a significant increase in right ventricular ejection fraction was detected. There was a little nonsignificant increase in MRI LIC values. Two patients with a baseline MRI LIC < 3 mg/g dw became pathological at the FU MRI (patient 1 moved from 1.69 to 3.59 mg/g dw; patient 2 moved from 2.17 to 3.78 mg/g dw). Out of the 21 patients with hepatic iron at the baseline MRI, 6 (28.6%) showed no iron at the FU MRI.
All changes in MRI parameters and in serum ferritin levels were comparable between the two groups (Table 3).
Patients with basal MRI LIC ≥ 3 mg/g/dw
At baseline 33 patients showed a MRI LIC ≥ 3 mg/g/dw: 12 non-chelated and 21 treated with DFO.
The mean administered dosage of DFO was 40.58 ± 5.63 mg/kg body weight via subcutaneous route on 3.71 ± 1.59 days/week. No side effects were recorded from MIOT centers in patients undertaking DFO.
The characteristics of these subgroups at baseline are reported in Table 4A. No significant differences were detected.
In no subgroup, there was a significant change in serum ferritin levels (non-chelated: mean difference between follow-up and baseline − 68.71 ± 147.80 ng/ml, P = 0.264 and DFO: mean difference between follow-up and baseline − 7.40 ± 166.79 ng/ml, P = 0.866). The decrease in serum ferritin level was comparable between the two subgroups (P = 0.481).
MRI LIC increased in a nonstatistically significant way in non-chelated patients (mean difference between follow-up and baseline 0.86 ± 6.39 mg/g dw, P = 0.651). Conversely, in DFO patients, there was a significant decrease in MRI LIC values (mean difference between follow-up and baseline − 2.20 ± 4.84 mg/g dw, P = 0.050). The change in MRI LIC values was not significantly different between the two subgroups (P = 0.155).
Patients with basal MRI LIC < 3 mg/g dw
At baseline, 18 patients showed no hepatic iron: 6 non-chelated and 12 treated with DFO.
The mean administered dosage of DFO was 39.44 ± 7.72 mg/kg body weight via subcutaneous route on 2.91 ± 1.30 days/week.
No side effects were recorded from MIOT centers in patients undertaking DFO.
The characteristics of these subgroups at baseline are reported in Table 4B. No significant difference was detected.
In both groups, there was an increase, although not statistically significant, in serum ferritin levels (non-chelated: mean difference between follow-up and baseline 192.50 ± 150.05 ng/ml, P = 0.083 and DFO: mean difference between follow-up and baseline 13.67 ± 131.75 ng/ml, P = 0.750). The increase in serum ferritin level was significantly higher in non-chelated patients (P = 0.047).
MRI LIC slightly increased in both groups (non-chelated: mean difference between follow-up and baseline 1.49 ± 2.85 mg/g dw, P = 0.257) and DFO: mean difference between follow-up and baseline 0.10 ± 1.04 mg/g dw, P = 0.734). The change in MRI LIC values was not significantly different between the two subgroups (P = 0.146).
Discussion
The MIOT network is a robust and scalable system in which T2* MRI-based iron overload assessment is available, accessible, and reachable for a significant and increasing number of thalassemia patients in Italy [9].
Currently, there is large consensus for the need of chelation therapy among patients with NTDT and significant iron overload (LIC ≥ 5 mg/g dw) [23]. However, in NTDT patients, it has been previously estimated by quantitative MRI R2* that LIC and serum ferritin levels have an acceptable relationship that may be used to guide the start of chelation therapy [24]. In Europe to date, the use of DFX is approved in NTDT patients with LIC ≥5 mg Fe/g dw or serum ferritin levels consistently over 800 ng/ml with inadequate response or a contraindication to DFO. Thus, both the need to accurately define the response achievable with DFO and the possibility to encounter patients intolerant and/or not effectively managed with DFX make mandatory to find accurate information on the activity of DFO and on the reciprocal relationship between iron overload parameters using the T2* technique. Firstly, we identified serum ferritin thresholds for predicting a LIC ≥ 5 mg/g dw and a LIC ≥ 3 mg/g dw. The identified LIC thresholds were fairly comparable to those found at R2*, but very similar between each other (525 and 468 ng/ml, respectively), suggesting that it may be hard to monitor chelation therapy in this range only on the basis of ferritin levels, probably due to the presence of confounders of the correlation between ferritin and LIC values such as liver steatosis [25]. On the other hand, it is also important to notice that our results about the ferritin thresholds are similar to those of Karimi et al. who showed that the best cutoff value for ferritin for the early diagnosis of liver iron overload (MRI LIC ≥ 3.2 mg/g dw) was 412 ng/ml [26]. Therefore, our results may also confirm that the cutoff point of serum ferritin of 800 ng/ml [23] could be late for starting iron chelation in NTDT patients.
Despite the relatively advanced age, our data of the whole study population at baseline are indicative of mild-to-moderate iron-overloaded population. We confirmed the absence of clinically significant myocardial iron overload among NTDT patients [27, 28] where a slight, but not statistically, increase in ferritin level and in LIC concentration was assessed in not treated patients. Interestingly, at final evaluation, an increase in RVEF was noticed in treated patients. No other similar observations were reported on right ventricular parameters following chelation therapy in a NTDT population. Further studies are needed to clarify how these data could be consistent and/or related with those previously observed at echocardiography either in the “OPTIMAL CARE” study where a protective effect of iron chelation therapy against pulmonary hypertension (PHT) was reported [29] or in the study of Isma’eel et al. where a correlation between LIC and PHT was found [30].
Some additional data came from the subgroup analysis of patients with and without significant hepatic iron overload at baseline. In fact, we firstly found that among iron-overloaded patients, DFO at 40.58 ± 5.63 mg/kg body weight on 3.71 ± 1.59 days/week was able to significantly reduce LIC (a decrease of − 2.20 ± 4.84 from a baseline of 10.91 ± 9.61 mg/g dw). It could be argued that a higher dose and/or number of days of DFO administration could have strengthen the increase in LIC observed among our patients to an extent comparable to that obtained in THALASSA trial (a decrease of 3.80 mg/g dw from a baseline of 14.6 mg Fe/g dw) with DFX used at 10 mg/kg per day. According to the identified relationships between ferritin levels and LIC in our ROC curves, such a result was observed in presence of almost unchanged ferritin levels. Conversely, no statistically significant difference at inter-treatment analysis was detected in LIC changes; it is conceivable that a more protracted follow-up would have revealed higher LIC changes among treated and not treated patients and, consequently, significant differences.
No data are available in the literature about the use of chelation therapy among NTDT patients with basal MRI LIC < 3 mg/g dw. In fact, for patients receiving deferasirox, interruption of treatment is recommended if serum ferritin levels decline below 300 ng/ml or if LIC drops below 3 mg Fe/g dw to avoid over-chelation. Our data highlight the possibility of subcutaneous DFO therapy at 39.44 ± 7.72 mg mg/kg body weight on 2.91 ± 1.30 days/week to be used to maintain patients at nearly normal levels of iron stores. No data of toxicity, side effects, and/or over-chelation of iron were reported from MIOT centers in patients undertaking such chelation treatment. Interestingly, regarding the statistically significant change in ferritin levels observed among not treated patients, it could be affirmed that ferritin levels in this scantily iron-overloaded population more accurately mark the iron loading and the iron store.
In conclusion, our data from MIOT network showed that iron chelation with DFO is able to significantly reduce hepatic iron in NTDT patients with significant burden at baseline.
This study has the limitations of a non-randomized trial including potential selection bias. But, given the“ real life nature” of this prospective study, presumably, it occurred that the non-chelated patients were those with less severe form of NTDT and therefore those accumulating less iron as reflected by the little nonsignificant increase in MRI LIC values observed in this population, and that patients with more severe NTDT were those receiving DFO treatment. Nevertheless, such a selection bias would have attenuated but not increased the significance of the effect of DFO on LIC reduction at the prospective comparison with not treated patients.
Despite prolonged injectable chelation may be inconvenient and cumbersome, it could be of utility for patients who for any reason cannot receive DFX or in countries where the DFX availability is restricted mainly due to the significantly higher costs in comparison to DFO [31]. Recently, it has been shown that DFX can be safely used in NTDT patients approaching the lower, near-normal iron burden and chelation interruption target of LIC < 3 mg/g/dw [32]. Our data provide first evidence of the feasibility and effectiveness of an ongoing clinical practice based on the use of reduced frequency of DFO administration to maintain iron in NTDT patients at normal levels. Further studies are needed to verify if this approach should be carried out particularly among defined populations of NTDT, such as those receiving occasional red blood cell transfusions and/or with high rate of body of iron loading. Additional prospective assessments of the ongoing MIOT data base are needed to verify if such chelation practice is feasible in long term and if it is associated to a further reduction of the incidence of complications linked to iron overload in NTDT without side effects from over-chelation.
References
Musallam KM, Cappellini MD, Daar S, Karimi M, El-Beshlawy A, Graziadei G, Magestro M, Wulff J, Pietri G, Taher AT (2014) Serum ferritin level and morbidity risk in transfusion-independent patients with beta-thalassemia intermedia: the ORIENT study. Haematologica 99(11):e218–e221
Musallam KM, Cappellini MD, Wood JC, Motta I, Graziadei G, Tamim H, Taher AT (2011) Elevated liver iron concentration is a marker of increased morbidity in patients with beta thalassemia intermedia. Haematologica 96(11):1605–1612
Taher AT, Porter J, Viprakasit V, Kattamis A, Chuncharunee S, Sutcharitchan P, Siritanaratkul N, Galanello R, Karakas Z, Lawniczek T, Ros J, Zhang Y, Habr D, Cappellini MD (2012) Deferasirox reduces iron overload significantly in nontransfusion-dependent thalassemia: 1-year results from a prospective, randomized, double-blind, placebo-controlled study. Blood 120(5):970–977
Taher AT, Porter JB, Viprakasit V, Kattamis A, Chuncharunee S, Sutcharitchan P, Siritanaratkul N, Galanello R, Karakas Z, Lawniczek T, Habr D, Ros J, Zhu Z, Cappellini MD (2013) Deferasirox effectively reduces iron overload in non-transfusion-dependent thalassemia (NTDT) patients: 1-year extension results from the THALASSA study. Ann Hematol 92(11):1485–1493
Ricchi P, Marsella M (2015) Profile of deferasirox for the treatment of patients with non-transfusion-dependent thalassemia syndromes. Drug Des Devel Ther 9:6475–6482
Cossu P, Toccafondi C, Vardeu F, Sanna G, Frau F, Lobrano R, Cornacchia G, Nucaro A, Bertolino F, Loi A, De Virgiliis S, Cao A (1981) Iron overload and desferrioxamine chelation therapy in beta-thalassemia intermedia. Eur J Pediatr 137(3):267–271
Pippard MJ, Weatherall DJ (1988) Iron balance and the management of iron overload in beta-thalassemia intermedia. Birth Defects Orig Artic Ser 23(5B):29–33
Calvaruso G, Vitrano A, Di Maggio R, Lai E, Colletta G, Quota A, Gerardi C, Rigoli LC, Sacco M, Pitrolo L, Maggio A (2015) Deferiprone versus deferoxamine in thalassemia intermedia: results from a 5-year long-term Italian multicenter randomized clinical trial. Am J Hematol 90(7):634–638
Meloni A, Ramazzotti A, Positano V, Salvatori C, Mangione M, Marcheschi P, Favilli B, De Marchi D, Prato S, Pepe A, Sallustio G, Centra M, Santarelli MF, Lombardi M, Landini L (2009) Evaluation of a web-based network for reproducible T2* MRI assessment of iron overload in thalassemia. Int J Med Inform 78(8):503–512
Ramazzotti A, Pepe A, Positano V, Rossi G, De Marchi D, Brizi MG, Luciani A, Midiri M, Sallustio G, Valeri G, Caruso V, Centra M, Cianciulli P, De Sanctis V, Maggio A, Lombardi M (2009) Multicenter validation of the magnetic resonance t2* technique for segmental and global quantification of myocardial iron. J Magn Reson Imaging 30(1):62–68
Pepe A, Positano V, Santarelli F, Sorrentino F, Cracolici E, De Marchi D, Maggio A, Midiri M, Landini L, Lombardi M (2006) Multislice multiecho T2* cardiovascular magnetic resonance for detection of the heterogeneous distribution of myocardial iron overload. J Magn Reson Imaging 23(5):662–668
Pepe A, Lombardi M, Positano V, Cracolici E, Capra M, Malizia R, Prossomariti L, de Marchi D, Midiri M, Maggio A (2006) Evaluation of the efficacy of oral deferiprone in beta-thalassemia major by multislice multiecho T2*. Eur J Haematol 76(3):183–192
Positano V, Pepe A, Santarelli MF, Scattini B, De Marchi D, Ramazzotti A, Forni G, Borgna-Pignatti C, Lai ME, Midiri M, Maggio A, Lombardi M, Landini L (2007) Standardized T2* map of normal human heart in vivo to correct T2* segmental artefacts. NMR Biomed 20(6):578–590
Meloni A, Positano V, Pepe A, Rossi G, Dell'Amico M, Salvatori C, Keilberg P, Filosa A, Sallustio G, Midiri M, D'Ascola D, Santarelli MF, Lombardi M (2010) Preferential patterns of myocardial iron overload by multislice multiecho T*2 CMR in thalassemia major patients. Magn Reson Med 64(1):211–219
Positano V, Salani B, Pepe A, Santarelli MF, De Marchi D, Ramazzotti A, Favilli B, Cracolici E, Midiri M, Cianciulli P, Lombardi M, Landini L (2009) Improved T2* assessment in liver iron overload by magnetic resonance imaging. Magn Reson Imaging 27(2):188–197
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105(4):539–542
Meloni A, Luciani A, Positano V, De Marchi D, Valeri G, Restaino G, Cracolici E, Caruso V, Dell'amico MC, Favilli B, Lombardi M, Pepe A (2011) Single region of interest versus multislice T2* MRI approach for the quantification of hepatic iron overload. J Magn Reson Imaging 33(2):348–355
Meloni A, Rienhoff HY Jr, Jones A, Pepe A, Lombardi M, Wood JC (2013) The use of appropriate calibration curves corrects for systematic differences in liver R2* values measured using different software packages. Br J Haematol 161(6):888–891
Wood JC, Enriquez C, Ghugre N, Tyzka JM, Carson S, Nelson MD, Coates TD (2005) MRI R2 and R2* mapping accurately estimates hepatic iron concentration in transfusion-dependent thalassemia and sickle cell disease patients. Blood 106(4):1460–1465
Angelucci E, Brittenham GM, McLaren CE, Ripalti M, Baronciani D, Giardini C, Galimberti M, Polchi P, Lucarelli G (2000) Hepatic iron concentration and total body iron stores in thalassemia major. N Engl J Med 343(5):327–331
Aquaro GD, Camastra G, Monti L, Lombardi M, Pepe A, Castelletti S, Maestrini V, Todiere G, Masci P, di Giovine G, Barison A, Dellegrottaglie S, Perazzolo Marra M, Pontone G, Di Bella G (2016) Reference values of cardiac volumes, dimensions, and new functional parameters by MR: a multicenter, multivendor study. J Magn Reson Imaging 45(4):1055–1067
Marsella M, Borgna-Pignatti C, Meloni A, Caldarelli V, Dell'Amico MC, Spasiano A, Pitrolo L, Cracolici E, Valeri G, Positano V, Lombardi M, Pepe A (2011) Cardiac iron and cardiac disease in males and females with transfusion-dependent thalassemia major: a T2* magnetic resonance imaging study. Haematologica 96(4):515–520
Taher A, Vichinsky E, Musallam K, Cappellini MD, Viprakasit V (2013) Guidelines for the management of non transfusion dependent thalassaemia (NTDT) [Internet]. Thalassaemia International Federation, Nicosia, Cyprus
Taher AT, Porter JB, Viprakasit V, Kattamis A, Chuncharunee S, Sutcharitchan P, Siritanaratkul N, Origa R, Karakas Z, Habr D, Zhu Z, Cappellini MD (2014) Defining serum ferritin thresholds to predict clinically relevant liver iron concentrations for guiding deferasirox therapy when MRI is unavailable in patients with non-transfusion-dependent thalassaemia. Br J Haematol 168(2):284–290
Ricchi P, Meloni A, Spasiano A, Costantini S, Pepe A, Cinque P, Filosa A (2018) The impact of liver steatosis on the ability of serum ferritin levels to be predictive of liver iron concentration in non-transfusion-dependent thalassaemia patients. Br J Haematol 180(5):721–726
Karimi M, Amirmoezi F, Haghpanah S, Ostad S, Lotfi M, Sefidbakht S, Rezaian S (2017) Correlation of serum ferritin levels with hepatic MRI T2 and liver iron concentration in nontransfusion beta-thalassemia intermediate patients: a contemporary issue. Pediatr Hematol Oncol 34(5):292–297
Roghi A, Cappellini MD, Wood JC, Musallam KM, Patrizia P, Fasulo MR, Cesaretti C, Taher AT (2010) Absence of cardiac siderosis despite hepatic iron overload in Italian patients with thalassemia intermedia: an MRI T2* study. Ann Hematol 89(6):585–589
Origa R, Barella S, Argiolas GM, Bina P, Agus A, Galanello R (2008) No evidence of cardiac iron in 20 never- or minimally-transfused patients with thalassemia intermedia. Haematologica 93(7):1095–1096
Taher AT, Musallam KM, Karimi M, El-Beshlawy A, Belhoul K, Daar S, Saned MS, El-Chafic AH, Fasulo MR, Cappellini MD (2010) Overview on practices in thalassemia intermedia management aiming for lowering complication rates across a region of endemicity: the OPTIMAL CARE study. Blood 115(10):1886–1892
Isma'eel H, Chafic AH, El Rassi F, Inati A, Koussa S, Daher R, Gharzuddin W, Alam S, Taher A (2008) Relation between iron-overload indices, cardiac echo-Doppler, and biochemical markers in thalassemia intermedia. Am J Cardiol 102(3):363–367
Pepe A, Rossi G, Bentley A, Putti MC, Frizziero L, D'Ascola DG, Cuccia L, Spasiano A, Filosa A, Caruso V, Hanif A, Meloni A (2017) Cost-utility analysis of three iron chelators used in monotherapy for the treatment of chronic iron overload in beta-thalassaemia major patients: an Italian perspective. Clin Drug Investig 37(5):453–464
Taher AT, Porter JB, Viprakasit V, Kattamis A, Chuncharunee S, Sutcharitchan P, Siritanaratkul N, Origa R, Karakas Z, Habr D, Zhu Z, Cappellini MD (2014) Approaching low liver iron burden in chelated patients with non-transfusion-dependent thalassemia: the safety profile of deferasirox. Eur J Haematol 92(6):521–526
Acknowledgements
We would like to thank all the colleagues involved in the MIOT project (https://miot.ftgm.it/).
We thank Claudia Santarlasci for her skillful secretarial work. We finally thank all patients for their cooperation.
Funding
The MIOT project receives “no-profit support” from industrial sponsorships (Chiesi Farmaceutici S.p.A. and ApoPharma Inc.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ricchi, P., Meloni, A., Pistoia, L. et al. The effect of desferrioxamine chelation versus no therapy in patients with non transfusion-dependent thalassaemia: a multicenter prospective comparison from the MIOT network. Ann Hematol 97, 1925–1932 (2018). https://doi.org/10.1007/s00277-018-3397-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-018-3397-3