Abstract
Previous studies showed that, in chronic lymphocytic leukemia (CLL) patients with isolated 13q deletion (13q-), those carrying higher percentage of leukemic cells with 13q- had more aggressive diseases. However, the prognostic value of the percentage of leukemic cells with 13q- in Chinese CLL patients with isolated 13q- remained to be determined. Using interphase fluorescence in situ hybridization (FISH), we identified 82 patients (25.4%) with isolated 13q deletion from a cohort of 323 untreated CLL patients. Among patients with isolated 13q deletion, cases of 13q- cells ≥ 80% (13q-H) had significantly shorter time to first treatment (TTT) than those of < 80% 13q- cells (13q-L) (median 11 vs. 92 months, p = 0.0016). A higher lymphocyte count (p = 0.0650) was associated with 13q-H, while other clinical, immunophenotypic, or molecular features did not differ between patients with 13q-H and 13q-L. Although 13q-H only showed marginal significance in multivariate analysis of TTT (hazards ratio 2.007; 95% confidence interval 0.975–4.129; p = 0.059), it helped refine the risk stratification based on Binet stage or immunoglobulin heavy chain variable gene (IGHV) status. In cases in Binet A or B stage, patients with 13q-H had a significantly shorter TTT (median TTT 18 months vs. undefined, p = 0.0101). And in IGHV mutated patients, 13q-H was also associated with reduced TTT (median TTT 13q-H. 18 months vs. 13q-L undefined, p = 0.0163). In conclusion, the prognosis of CLL patients with isolated 13q deletion was heterogeneous with 13q-H identifying patients with worse outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic lymphocytic leukemia (CLL) is the most prevalent leukemia in adults in western countries [1]. CLL has a highly variable clinical course, with some patients progressing rapidly within several months of diagnosis and others living without treatment for years [2]. The study by Döhner et al. has proposed a hierarchical model of classification of CLL patients based on cytogenetics [3]. Isolated 13q deletion (13q-) is the most common cytogenetic aberration detected by fluorescence in situ hybridization (FISH) with favorable prognosis. However, more aggressive diseases with shorter time to first treatment (TTT) and worse overall survival (OS) can be seen in CLL patients with higher percentage of cells harboring 13q14 deletion in recent reports [1, 4,5,6]. However, in these studies, TP53, SF3B1, and NOTCH1 mutations were not investigated. Moreover, it remains unclear whether or not the negative impact of higher percentage of 13q- cells could be attributed to its association with other prognostic factors.
CLL is relatively rare in Asians [7]. Previous studies revealed that Chinese patients with CLL displayed different clinical and molecular features from CLL patients in western countries [8, 9]. A prospective multicenter study reported that 13q- was the most frequent cytogenetic abnormality (47.6%) in Chinese patients with CLL, which was also associated with early stage disease [10]. One study from our center demonstrated that patients with isolated 13q- had significantly better outcome than others [11]. However, whether the percentage of leukemic cells with 13q- has a clinical impact in Chinese patients with isolated 13q- is still elusive. In this study, we systemically described the frequency of 13q- as well as isolated 13q- in a cohort of untreated patients with CLL in China; further, the prognostic role of the percentage of cells with 13q- and its relationship to other prognostic markers were examined in patients with isolated 13q-.
Materials and methods
Patients
Three hundred twenty-three patients with CLL diagnosed between January 2001 and April 2017 who have available pretreatment cytogenetic statuses [del (13q14), +12, del (11q22.3) and del (17p13)] from the First Affiliated hospital of Nanjing Medical University were included in this study. The diagnosis of CLL was established based on the International Workshop on CLL-National Cancer Institute (IWCLL-NCI) [12]. Among 323 patients, 198 (61.3%) received treatments for CLL with 91 being treated immediately after diagnosis, and 107 received treatments during follow-up. The most common first-line regimens included fludarabine and cyclophosphamide (N = 41; 20.7%); chlorambucil (N= 38; 19.2%); fludarabine, cyclophosphamide and rituximab (N = 32; 16.2%), and bendamustine (N = 24; 12.1%), and other regimens were summarized in supplemental Table 1. All the samples were collected prior to treatment. Follow-up data were retrieved from medical records or by interviewing (directly or by phone) the patients, their family members, or their physicians in the local hospitals.
Fluorescence in situ hybridization (FISH)
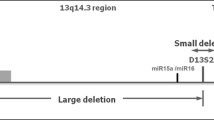
Interphase FISH was analyzed in peripheral blood (PB)/bone marrow (BM) samples using commercially available probes for del (13q14), + 12, del (11q22.3), and del (17p13), and the results were interpreted following Döhner H′ hierarchical model [3]. The methods and probes used for FISH analysis of our study have been described elsewhere [9, 13]. The probes included LSI ATM for detection of del (11q22.3), CEP12 (centromere 12) for detection of + 12, LSI D13S319 for detection of del (13q14), and LSI p53 for detection of del (17p13) with the cutoffs for positivity 7.7, 3.0, 10, and 5.2%, respectively.
Analyses of NOTCH1, SF3B1, and TP53 mutations and IGHV gene sequencing
Sanger sequencing of TP53 (exons 4–9), NOTCH1 (pest domain), and SF3B1 (exons 14–16) was conducted as previously described [9, 13]. Sequence analysis of IGHV was performed as previously reported and germline IGHV was defined as ≥ 98% germline homology [8].
Immunophenotyping
Immunophenotyping of CD38 and ZAP70 was performed as previously described [1, 14]. The cutoffs for CD38 positivity and ZAP-70 positivity were 30 and 20%, respectively.
Statistical analysis
The Student’s t test or Mann-Whitney U test was carried out to compare continuous variables between two groups. D’Agostino-Pearson omnibus normality test was used to examine if the values came from Gaussian distribution. If the values passed normality test, we used Student’s t test, or Mann-Whitney U test was used. Categorical variables were compared by Fisher’s exact test. Survival was defined as time from diagnosis until death or last follow-up. TTT was calculated as time from diagnosis until first treatment. Survival curves were constructed using Kaplan-Meier method and log-rank test was used for comparison. Multivariate analysis was done by multivariate Cox model. All statistical analyses were performed using Graphpad Prism 6 (GraphPad Software, San Diego, CA) software, SPSS (version 19.0) software (IBM Corporation, Armonk, NY, USA), and Microsoft Office 2010 software for Windows. p values were two-sided, and p < 0.05 was defined as significant.
Results
Clinical and biological characteristics of CLL patients carrying 13q-
The clinical characteristics of the 323 patients are summarized in Table 1. There was a predominance of males (67.2%), and the median age was 61 (range 16–92 years), and the the median follow-up was 45.0 months (interquartile range [IQR] 24.0–70.0 months). According to the Binet clinical staging system, 140 (43.8%) patients were in Binet A, 97 (30.3%) in Binet B, and 83 (25.9%) in Binet C.
Using 10% as the cutoff for 13q-, we identified 122 patients (37.8%) with 13q-. Eighty-two patients (25.4%) had 13q- as the sole cytogenetic aberration, while 40 patients (12.4%) had 13q- accompanied by other cytogenetic abnormalities (10 cases had a 11q deletion, 13 had trisomy 12, and 27 showed 17p deletion). In ten cases with 13q-, three aberrations were identified. 17p deletion, 11q deletion, and + 12 were detected in 48 (14.9%), 38 (11.8%), and 65 cases (20.1%), respectively. No aberrations were found in 116 (35.9%) cases. In 82 cases with isolated 13q-, 66 cases had data describing monoallelic or biallelic loss of 13q. In the 66 patients, 7 patients (10.6%) displayed biallelic 13q- including 5 cases showing both biallelic 13q- and monoallelic 13q-.
The clinical and laboratory characteristics were compared between patients with isolated 13q- and non-isolated 13q-. Absolute white blood cell count (p = 0.0037), absolute lymphocyte count (p = 0.0023), and lactate dehydrogenase (p = 0.0005) were significantly higher in patients with non-isolated 13q-, when compared with those with isolated 13q- (Table 2). Patients with non-isolated 13q- showed higher β2-microglobulin level, although without statistical significance (p = 0.0541). TP53 mutation (p < 0.0001), NOTCH1 mutation (p = 0.0425), and unmutated IGHV (p = 0.0004) were less frequent in patients with isolated 13q-. Based on CLL-international prognostic index (CLL-IPI), CLL with non-isolated 13q- were remarkably enriched with low-risk or intermediate-risk patients (p < 0.0001). These two groups of patients did not differ in other clinical or laboratory features. In cases with isolated 13q-, baseline features were also compared between cases with monoallelic 13q- and those with biallelic 13q-. Cases with biallelic 13q- displayed a higher percentage of 13q- than those with monoallelic 13q- (80 vs. 50%, p=0.0127), and these two groups did not show significant differences in other baseline characteristics (Supplemental Table 2).
CLL patients with a higher percentage of isolated 13q- cells have a shorter TTT
X-title analysis conducted to determine the prognostic impact of the percentage of cells with 13q- on TTT identified 80% as a cutoff. Based on this cutoff, these cases could be divided into two groups with 19/82 (23.2%) patients having a higher percentage of isolated 13q- cells (13q-H) (≥ 80%) and 63/82 (76.8%) having a lower percentage of isolated 13q- cells (13q-L) (< 80%). Patients with 13q-H had a significant shorter TTT than those with 13q-L (median TTT 11 vs. 92 months, p = 0.0016, Fig. 1a). However, there was no significant difference in OS between the two groups (median OS: not reached vs. 134 months, p = 0.5977, Fig. 1b). Moreover, the TTT of cases with 13q-H was similar to those with 17p- or 11q- (median TTT 12 months, p = 0.9847, Fig. 1c), but shorter than cases with + 12 or normal karyotype (median TTT 31 months, p = 0.0844, Fig. 1d).
Association of the percentage of 13q- cells with clinical, immunophenotypic, and molecular characteristics of CLL patients with isolated 13q-
Clinical, immunophenotypic, and molecular data were collected and were compared between patients with 13q-H and patients with 13q-L (Table 3). A higher lymphocyte count at diagnosis (median: 35.8 × 109/L vs. 19.2 × 109/L, p = 0.0650) was associated with higher percentage of cells with 13q-, although the result was not statistically significant (Table 3). Patients with 13q-H also showed lower platelet counts (median 131 × 109/L vs. 153 × 109/L, p = 0.0944). Although more frequent high-risk or very high-risk patients were in cases with 13q-H (33.3% vs. 13.3%, p = 0.1219) according to CLL-IPI, this difference was not of statistical significance. There were no significant differences between two groups in other clinical, immunophenotypic, and molecular features.
Univariate analysis and multivariate Cox analysis of TTT
We then incorporated 13q- percentage, IGHV mutation status, Binet stage, TP53 mutation, CD38 expression, and ZAP-70 expression into univariate analysis of TTT. We found that 13q-H, unmutational IGHV, and advanced Binet stage predicted significantly shorter TTT in patients with isolated 13q- (Table 4). Multivariate Cox analysis revealed that, unmutational IGHV (p = 0.020) and advanced Binet stage (p = 0.012) independently predicted shorter TTT, while 13q-H only showed marginal significance (p = 0.059).
The percentage of 13q- cells refined the prognostification of CLL patients with isolated 13q-
As unmutational IGHV and advanced Binet stage were independent prognostic factors in predicting TTT, we thereby determined if the percentage of 13q- cells could improved the prognostification of patients with isolated 13q- based on these two factors. We found that in cases in Binet A/B stage, 13q-H identified patients with significantly shorter TTT (median TTT 18 months vs. undefined, p = 0.0101, Fig. 2a). Additionally, in 60 cases with mutated IGHV, patients with 13q-H displayed remarkably shorter TTT, when compared with others. (median TTT 18 months vs. undefined, p = 0.0163, Fig. 2b).
Discussion
In the past years, several studies have demonstrated that cytogenetic changes are closely related to the clinical outcome of patients with CLL. Cytogenetic aberrations such as loss of ATM or TP53 genes portend a poor prognosis, while isolated 13q- and normal karyotype indicating a good prognosis [3]. However, the clinical course of CLL patients with isolated 13q- was heterogeneous; some patients with sole-13q- do not require treatment for several years or decades while others develop aggressive disease with shorter TTT [1, 4,5,6, 15]. In our cohort of 323 untreated patients with CLL, the incidence of 13q- and isolated 13q- was 37.8 and 25.4%, respectively. Previous studies have shown that, in western countries, 13q- detected by FISH occurred in more than 50% of patients with CLL [3, 6, 15, 16], which was more frequent than that of our cohort. This might be due to more cases in advanced stage in our cohort (Binet B/C, 56.2%). And isolated 13q- was present in 14–45% of patients with CLL in previously studies, and the incidence of isolated 13q- in our cohort was within this range. In patients with isolated 13q-, our study indicated a relationship between higher percentage of cells showing 13q- and shorter TTT. However, no difference in OS was observed between the 13q-H group and the 13q-L group, probably due to relatively short follow-up.
In 2009, in a study of 109 patients, Hernandez et al. reported that patients with isolated 13q- in more than 80% abnormal cells had a shorter TTT and OS [4]. And the study by Van Dyke et al. found that patients with ≥ 65.5% isolated 13q- nuclei had a shorter TTT but not OS in a cohort of 323 patients [6]. Our study further confirmed that patients with more than 80% cells showing isolated 13q- had a significantly shorter TTT. Furthermore, we identified a possible association between a higher lymphocyte count and higher percentage of cells carrying isolated 13q-, which suggested a higher burden of neoplastic B cells might contribute to the higher percentage of leukemic cells showing 13q-. However, Dal Bo et al. found that there was no correlation between percentage of 13q- cells and percentage of neoplastic B cells, which argued against this possible association [5].
The mechanism underlying the heterogeneity of patients remains to be elucidated. Gene expression profiling revealed cases with more than 80% cells harboring 13q- and those with less than 80% displayed significantly different gene expression, with genes involved in apoptosis and cell cycle arrest downregulated and proliferation-promoting genes upregulated [4]. The study by Baliakas et al. revealed that TP53, NOTCH1, and SF3B1 were mutated in 5.0, 6.5, and 9.9% of patients of isolated 13q-, and these gene mutations conferred a significantly poor prognosis in these patients [17]. Furthermore, incorporation of gene mutations into the cytogenetics-based model proposed by Dohner et al. refined the prognostification in CLL [17]. As a result, we analyzed these mutations in our cohort. The frequencies of each gene mutation did not differ between patients with 13q-H and cases with 13q-L, which may be due to the small size of patients with 13q- in our study. Additionally, the distribution of IGHV mutation did not vary significantly between these two groups. Therefore, the biological factors accounting for the aggressiveness of cases with 13q-H remained to be explored.
We also performed multivariate Cox analysis of TTT in patients with isolated 13q-, which identified advanced Binet and IGHV mutation status as independent prognostic factors in predicting TTT. Although the percentage of 13q- only showed marginal significance as an independent factor, subsequent analysis showed that it can improve the risk stratification based on Binet stage or IGHV status, emphasizing it as a complementary prognostic marker in patients with isolated 13q-.
However, our study had several limitations. This was a single-center retrospective study and we did not analyze therapeutic implications of the percentage of cells carrying isolated 13q-. Besides, 13q14 deletion size, which had potential prognostic value, was not evaluated in our study.
In conclusion, our results suggest that in patients with CLL with isolated 13q-, the frequencies of 13q- cells influenced the clinical outcome, and a higher percentage of abnormal nuclei carrying 13q- was associated with a shorter TTT and required treatment rapidly. Our results provide additional value in the prognosis of CLL. Our findings highlight the importance of quantification of the number of cells with 13q- in FISH testing. Furthermore, future studies are warranted to better define the genomic landscape of patients with cells showing isolated 13q- and precisely predict the outcome of these patients.
References
Puiggros A, Delgado J, Rodriguez-Vicente A, Collado R, Aventin A, Luno E, Grau J, Hernandez JA, Marugan I, Ardanaz M, Gonzalez T, Valiente A, Osma M, Calasanz MJ, Sanzo C, Carrio A, Ortega M, Santacruz R, Abrisqueta P, Abella E, Bosch F, Carbonell F, Sole F, Hernandez JM, Espinet B (2013) Biallelic losses of 13q do not confer a poorer outcome in chronic lymphocytic leukaemia: analysis of 627 patients with isolated 13q deletion. Br J Haematol 163(1):47–54. https://doi.org/10.1111/bjh.12479
Nabhan C, Rosen ST (2014) Chronic lymphocytic leukemia: a clinical review. JAMA 312(21):2265–2276. https://doi.org/10.1001/jama.2014.14553
Dohner H, Stilgenbauer S, Benner A, Leupolt E, Krober A, Bullinger L, Dohner K, Bentz M, Lichter P (2000) Genomic aberrations and survival in chronic lymphocytic leukemia. N Engl J Med 343(26):1910–1916. https://doi.org/10.1056/NEJM200012283432602
Hernandez JA, Rodriguez AE, Gonzalez M, Benito R, Fontanillo C, Sandoval V, Romero M, Martin-Nunez G, de Coca AG, Fisac R, Galende J, Recio I, Ortuno F, Garcia JL, de las Rivas J, Gutierrez NC, San Miguel JF, Hernandez JM (2009) A high number of losses in 13q14 chromosome band is associated with a worse outcome and biological differences in patients with B-cell chronic lymphoid leukemia. Haematologica 94(3):364–371. https://doi.org/10.3324/haematol.13862
Dal Bo M, Rossi FM, Rossi D, Deambrogi C, Bertoni F, Del Giudice I, Palumbo G, Nanni M, Rinaldi A, Kwee I, Tissino E, Corradini G, Gozzetti A, Cencini E, Ladetto M, Coletta AM, Luciano F, Bulian P, Pozzato G, Laurenti L, Forconi F, Di Raimondo F, Marasca R, Del Poeta G, Gaidano G, Foa R, Guarini A, Gattei V (2011) 13q14 deletion size and number of deleted cells both influence prognosis in chronic lymphocytic leukemia. Genes Chromosom Cancer 50(8):633–643. https://doi.org/10.1002/gcc.20885
Van Dyke DL, Shanafelt TD, Call TG, Zent CS, Smoley SA, Rabe KG, Schwager SM, Sonbert JC, Slager SL, Kay NE (2010) A comprehensive evaluation of the prognostic significance of 13q deletions in patients with B-chronic lymphocytic leukaemia. Br J Haematol 148(4):544–550. https://doi.org/10.1111/j.1365-2141.2009.07982.x
Yang SM, Li JY, Gale RP, Huang XJ (2015) The mystery of chronic lymphocytic leukemia (CLL): why is it absent in Asians and what does this tell us about etiology, pathogenesis and biology? Blood Rev 29(3):205–213. https://doi.org/10.1016/j.blre.2014.12.001
Marinelli M, Ilari C, Xia Y, Del Giudice I, Cafforio L, Della Starza I, Raponi S, Mariglia P, Bonina S, Yu Z, Yang W, Qiu L, Chan T, Piciocchi A, Kwong YL, Tse E, Li J, Guarini A, Xu W, Foa R (2016) Immunoglobulin gene rearrangements in Chinese and Italian patients with chronic lymphocytic leukemia. Oncotarget 7(15):20520–20531. https://doi.org/10.18632/oncotarget.7819
Xia Y, Fan L, Wang L, Gale RP, Wang M, Tian T, Wu W, Yu L, Chen YY, Xu W, Li JY (2015) Frequencies of SF3B1, NOTCH1, MYD88, BIRC3 and IGHV mutations and TP53 disruptions in Chinese with chronic lymphocytic leukemia: disparities with Europeans. Oncotarget 6(7):5426–5434. https://doi.org/10.18632/oncotarget.3101
Qiu HX, Xu W, Cao XS, Zhou M, Shen YF, Xu YL, Sun XM, Liu Q, Wang R, Qiu HR, Wang JS, Li JY (2008) Cytogenetic characterisation in Chinese patients with chronic lymphocytic leukemia: a prospective, multicenter study on 143 cases analysed with interphase fluorescence in situ hybridisation. Leuk Lymphoma 49(10):1887–1892. https://doi.org/10.1080/10428190802308710
Xu W, Li JY, Li L, Yu H, Shen QD, Fan L, Qiao C, Hong M, Qian SX, Qiu HX (2008) Fluorescent in situ hybridization with a panel of probes detects molecular cytogenetic abnormalities in patients with chronic lymphocytic leukemia. Zhonghua Yi Xue Za Zhi 88(36):2537–2540
Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Dohner H, Hillmen P, Keating MJ, Montserrat E, Rai KR, Kipps TJ (2008) Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the international workshop on chronic lymphocytic leukemia updating the National Cancer Institute-working group 1996 guidelines. Blood 111(12):5446–5456. https://doi.org/10.1182/blood-2007-06-093906
Miao Y, Fan L, Wu YJ, Xia Y, Qiao C, Wang Y, Wang L, Hong M, Zhu HY, Xu W, Li JY (2016) Low expression of CD200 predicts shorter time-to-treatment in chronic lymphocytic leukemia. Oncotarget 7(12):13551–13562. https://doi.org/10.18632/oncotarget.6948
Wu YJ, Wang H, Liang JH, Miao Y, Liu L, Qiu HR, Qiao C, Wang R, Li JY (2016) Using the geometric mean fluorescence intensity index method to measure ZAP-70 expression in patients with chronic lymphocytic leukemia. Onco Targets Ther 9:797–805. https://doi.org/10.2147/OTT.S94613
Gerrie AS, Bruyere H, Chan MJ, Dalal CB, Ramadan KM, Huang SJ, Toze CL, Gillan TL (2012) Immunoglobulin heavy chain (IGH@) translocations negatively impact treatment-free survival for chronic lymphocytic leukemia patients who have an isolated deletion 13q abnormality. Cancer Genet 205(10):523–527. https://doi.org/10.1016/j.cancergen.2012.05.011
Shanafelt TD, Witzig TE, Fink SR, Jenkins RB, Paternoster SF, Smoley SA, Stockero KJ, Nast DM, Flynn HC, Tschumper RC, Geyer S, Zent CS, Call TG, Jelinek DF, Kay NE, Dewald GW (2006) Prospective evaluation of clonal evolution during long-term follow-up of patients with untreated early-stage chronic lymphocytic leukemia. J Clin Oncol 24(28):4634–4641. https://doi.org/10.1200/JCO.2006.06.9492
Baliakas P, Hadzidimitriou A, Sutton LA, Rossi D, Minga E, Villamor N, Larrayoz M, Kminkova J, Agathangelidis A, Davis Z, Tausch E, Stalika E, Kantorova B, Mansouri L, Scarfo L, Cortese D, Navrkalova V, Rose-Zerilli MJ, Smedby KE, Juliusson G, Anagnostopoulos A, Makris AM, Navarro A, Delgado J, Oscier D, Belessi C, Stilgenbauer S, Ghia P, Pospisilova S, Gaidano G, Campo E, Strefford JC, Stamatopoulos K, Rosenquist R (2015) Recurrent mutations refine prognosis in chronic lymphocytic leukemia. Leukemia 29(2):329–336. https://doi.org/10.1038/leu.2014.196
Funding
This study was supported by National Natural Science Foundation of China (30971296, 81170485, 81170488, 81370657, 81470328, 81500125, 81522001, 81570141), Project of National Key Clinical Specialty, the National Science & Technology Pillar Program (2014BAI09B12), and a project funded by Jiangsu Provincial Special Program of Medical Science (BL2014086).
Author information
Authors and Affiliations
Contributions
J.Y.L, W.X, and Y.Q.M designed the study. Y.Q.M, Q.S, K.S, S.S.Z, Y.X, S.C.Q, H.R.Q, H.Y, H.X, H.Y.Z, J.Z.W, W.W, L.C, L.W, and L.F collected and analyzed the data. Y. M and Y.Q.M wrote the draft of the paper, and all authors contributed in writing and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
The study was approved by the Ethic Committee of the First Affiliated Hospital of Nanjing Medical University and conducted in accordance with the Declaration of Helsinki. Informed consent was provided by the subjects in the study.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Dr Jian-Yong Li is the first corresponding author.
Electronic supplementary material
ESM 1
(DOC 53 kb)
Rights and permissions
About this article
Cite this article
Miao, Y., Miao, Y., Shi, K. et al. A higher percentage of cells with 13q deletion predicts worse outcome in Chinese patients with chronic lymphocytic leukemia carrying isolated 13q deletion. Ann Hematol 97, 1663–1669 (2018). https://doi.org/10.1007/s00277-018-3359-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-018-3359-9