Abstract
Infections and infectious complications are the major cause of morbidity and mortality in febrile neutropenic patients after autologous stem cell transplantation. Laboratory biomarkers are helpful for early identification of critically ill patients and optimal therapy management. Several studies in adult non-neutropenic patients proposed sTREM-1 as a superior biomarker for identification of septic patients as well as a predictor for survival in these patients compared with procalcitonin (PCT), C-reactive protein (CRP), or interleukin-8 (IL-8). Here, to assess the utility of PCT, CRP, IL-8, and sTREM-1 in febrile neutropenia, 44 patients presenting with febrile neutropenia after autologous stem cell transplantation were recruited in a single-center prospective pilot study. We analyzed PCT and CRP as well as IL-8 and sTREM-1 levels pre- and post-transplantation at defined time points. In 20 of 44 patients, concentration of sTREM-1 was under the detection level at appearance of febrile neutropenia. Mean levels of PCT, IL-8, and CRP were significantly increased in infections of critically ill patients who by dysfunction or failure of one or more organs/system depend on survival from advanced instruments of monitoring and therapy. However, all tested biomarkers could not distinguish between presence and absence of bloodstream infection. The combination of the biomarkers PCT and IL-8 achieved a high sensitivity of 90% and specificity of 74% for the identification of serious complications in febrile neutropenia, whereas the combination of CRP and PCT or IL-8 achieved a high sensitivity of 100%, but with the addition of a low specificity of 47or 41%. In conclusion, we found that the measurement of sTREM-1 concentration at presentation of febrile neutropenia is not useful to identify bacterial bloodstream infections and critically ill patients. PCT and IL-8 are useful biomarkers for the early identification of critically ill patients, compared to CRP and sTREM-1 in febrile neutropenia. PCT or IL-8 in combination with clinical parameters should be considered in routine measurement to identify critically ill patients as early as possible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infections and infection-related complications remain one major cause of morbidity and mortality in patients with febrile neutropenia (FN) after high-dose chemotherapy and autologous stem cell transplantation (auto-SCT) [1]. Thus, standard care for patients with FN consists of frequent monitoring of vital signs and empirical treatment with intravenous broad-spectrum antibiotics. Especially in patients with severe neutropenia, defined as an absolute neutrophil count of less than 0.5 × 109/L (< 500/μl) [2], adequate management on presentation with FN and early identification of critically ill patients might be the most effective strategy to prevent the development of severe complications. Beside clinical scoring systems like the Multinational Association of Supportive Care in Cancer (MASCC) risk index score or the quick sepsis-related organ failure assessment (qSOFA), which may fail in patients with hematological malignancies or due to the presence of FN, the laboratory measurement of circulating markers of inflammation plays an important role in risk stratification [3].
On a routine basis, the hepatic acute phase reactant C-reactive protein (CRP) is the most commonly used biomarker and recommended by the FN guideline of the European Society of Medical Oncology (ESMO) [2]. Unfortunately, at onset of inflammation, low CRP levels do not exclude development of serious and significant inflammation, demonstrating a low specificity and positive predictive value in earlier FN studies [4].
Along the same line, procalcitonin (PCT) which is induced by bacterial endotoxins and exotoxins has emerged as a biomarker for guiding antibiotic treatment in septic, non-neutropenic adult patients and for distinguishing bacterial from non-bacterial infections [5, 6]. However, up to that point in only one prospective study, PCT-guided antibiotic treatment in neutropenic patients was not useful to reduce the use of antibiotics, but proved to be a marker of bacteremia [7]. Moreover, a correlation between disease severity and serum levels of PCT has been observed previously [8,9,10]. Nevertheless, the diagnostic accuracy of PCT for the diagnosis of bacterial infections in patients with FN varied in several studies [4]. Beside CRP and PCT, interleukin-8 (IL-8) has been recommended in pediatric and adult FN as an additional useful biomarker, especially for the early detection of a bacterial infection [11, 12]. The combination of PCT and IL-8 reached a sensitivity of 100% for bloodstream infections in pediatric patients [13].
During the last decade, soluble-triggering receptor expressed on myeloid cells-1 (sTREM-1) has been identified as a novel potential biomarker for the diagnosis of sepsis and/or development of serious infectious complications. TREM-1 has been discovered by Bouchon et al. in 2000 and is a cell-surface receptor expressed on monocytes, macrophages, and neutrophils [14]. TREM-1 expression is increased in infectious bacterial and fungal diseases and associated with the release of its soluble form. Soluble TREM-1 can be directly measured in several human body fluids, including serum, pleural effusion, sputum, and urine during infections [15,16,17]. The origin of sTREM-1 has been explained with two hypotheses. The first hypothesis relies on a splice variant of the mRNA of TREM-1 [18], whereas in the second hypothesis, sTREM-1 is generated through the proteolytic cleavage of mature cell surface-anchored TREM-1 [19]. Su et al. found that serum sTREM-1 levels at a cut-off value of 64.4 pg/ml yield a sensitivity of 91% and a positive predictive value of 0.989 for distinguishing septic from non-septic patients [20]. Despite the unknown source of sTREM-1, several studies focusing on patients with sepsis in non-neutropenic patients have additionally demonstrated that the value of plasma sTREM-1 is superior to CRP and PCT in early diagnosis and prognosis prediction [21, 22].
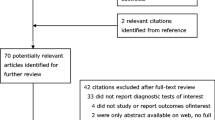
Thus, we performed a prospective single-center study to determine the usefulness of sTREM-1, CRP, PCT, and IL-8 for identification of bacterial infection and development of serious complications among patients with FN after auto-SCT (Fig. 1).
Patients and methods
Patient cohort
Patients treated with high-dose chemotherapy followed by auto-SCT from April 2015 to November 2016 at the Department of Hematology and Medical Oncology at the University Medical Center of Mainz, Germany, agreed to participate in the prospective study after reading and signing the written informed consent. The study was carried out in accordance to the principles outlined in the Declaration of Helsinki and was approved by the local ethics committee (Approval no: 837.455.14; Landesaerztekammer Rheinland-Pfalz, Mainz, Germany). Sample size of the control and study population has been calculated with a significance level of 0.05 and achieved a power > 80%. Clinical data of all patients were collected from their patient charts. High-dose chemotherapy and auto-SCT were performed in accordance with Joint Accreditation Committee-ISCT & EBMT (JACIE) standards. The patient characteristics relating to age, gender, type of hematological malignancy, remission status, absolute leukocyte counts, duration of febrile episode, and engraftment are shown in Table 1. Febrile neutropenia was defined as leukocytes lower than 0.5 × 109/l as well as either with an temperature of > 38.3 °C in a single measurement, or with > 38.0 °C in two consecutive measurements sustained over 1-h period; the temperature was obtained by placing a thermometer in the apex of the axilla with the arm pressed closely to the side of the body for the time recommended by the manufacturer of the thermometer. No prophylactic antibiotic treatment was administered and all patients received a broad-spectrum empirical antibiotic therapy during febrile neutropenia. Prior to the start of antibiotic treatment, standard bacterial cultures of appropriate samples have been taken to check for the presence or absence of bacterial infections. The patients were continuously monitored to determine the development of serious complications in FN including cardiac/respiratory/renal failure, hypotension, confused/altered mental state, intensive care unit (ICU) admission, arrhythmias requiring treatment, and survival [23]. Sera samples for measurement of PCT, IL-8, CRP, and sTREM-1 have been collected within 24 h after appearance of neutropenic fever.
Detection of PCT, CRP, sTREM-1, and IL-8
Serum concentrations of PCT were determined with TRACE™ Technology on a BRAHMS KRYPTOR compact PLUS. The assay has an analytical sensitivity of 0.02 ng/ml. CRP was measured on a latex-enhanced immunoturbidimetric assay on an Architect c8000 Analyzer from Abbott Core Laboratory. IL-8 concentration was analyzed using a commercial, solid phase sandwich ELISA kit (Quantikine R&D Systems, Inc. Minneapolis, MN, USA). Our self-made sTREM-1 ELISA has been established and described previously [24]. After adding standard dilutions (recombinant human TREM-1 in 7.5% BSA-PBS) and samples diluted 1:1.5, the plates were incubated for 1.5 h at room temperature (RT). All dilutions were carried out in blocking buffer and measured in triplicates on a Tecan GENios™ plate reader. Our in-house sTREM-1 ELISA has a limit of detection (LOD) of 4 pg/ml with a total variability of 15%. Patients with sTREM-1 concentration under 4 pg/ml were assessed as not detectable.
Statistical analysis
GraphPad Prism software v6 (GraphPad software, La Jolla, CA, USA) was used for data analysis. Results were expressed as the mean ± SD if not otherwise specified. Comparisons between groups for testing of statistical significance were calculated using the Mann-Whitney U test and Kruskal-Wallis test in combination with Dunn’s multiple comparison test for non-parametric data. A p value < 0.05 was considered as statistically significant. Receiver operating characteristic (ROC) curves including Youden’s index were employed to evaluate sTREM-1, PCT, IL-8, and CRP related to bloodstream infection, microbiologically documented infection (MDI), and development of serious complications in FN.
Results
A total of 44 neutropenic patients were enrolled in the study and blood sera were collected within 24 h after first presentation of fever. Additionally, sera from 27 patients were collected before and after high-dose chemotherapy as well as 1 day after auto-SCT and 48–72 h after first presentation with fever. First time of FN presented on average 6 days after auto-SCT and lasted about 3 days. In 28 of 44 patients (63.6%), proven bloodstream infection was documented. The majority of bloodstream infections were caused by gram-positive (57.1%), followed by gram-negative bacteria (32.2%). No yeast infections and only one viral bloodstream infection were detected. In the majority of patients, the clinically suspected focus of infection appeared to be abdominal (59.1%). Ten out of 44 patients (22.7%) developed serious complications, i. e., cardiac/respiratory/renal failure, hypotension, confused/altered mental state, ICU admission, arrhythmias requiring treatment, and death. Unfortunately, one patient died in ICU 8 days after auto-SCT based on acute respiratory failure. All patient characteristics are listed in Table 1.
In patients, before the start of high-dose chemotherapy, the concentration of sTREM-1 was 26.9 ± 25.7 pg/ml with corresponding levels of CRP < 5 mg/l and PCT < 0.1 ng/ml. The concentration of sTREM-1 after high-dose chemotherapy and auto-SCT decreased in a minor degree to 21.4 ± 27.8 and 15.5 ± 20.0 pg/ml, respectively. Neutropenic patients with the first presentation of fever had a sTREM-1 concentration of 24.9 ± 47.8 pg/ml. It needs to be pointed out that for 20 of 44 patients, sTREM-1 concentration was under the detection level of 4 pg/ml and altogether significantly reduced compared to patients before the start of high-dose chemotherapy (p < 0.05). In contrast, the corresponding levels of the other inflammatory markers were significantly elevated: CRP was 117.5 ± 93.1 mg/l, PCT was 3.7 ± 8.8 ng/ml, and IL-8 was 66.8 ± 227.4 pg/ml. Concentration of sTREM-1 after 48–72 h of fever was 2.3 ± 4.5 pg/ml and likewise significantly reduced (Fig. 2). For patients with or without bloodstream infection as well as MDI, no significant differences between the groups for concentrations of sTREM-1, IL-8, PCT, and CRP were observed. However, patients developing a serious complication showed significantly elevated levels of PCT (14.2 ± 14.3 ng/ml; p < 0.0001), IL-8 (230.6 ± 454.8 pg/ml; p = 0.0024), and CRP (175.3 ± 109.2 mg/l; p = 0.0388), whereby CRP demonstrated the lowest statistical significance. Mean sTREM-1 levels did not differ significantly (42.0 ± 76.9 pg/ml; p = 0.3951). All values are shown in Table 2.
Concentrations of sTREM-1 before and after HD-chemotherapy (HD-chemo). sTREM-1 levels in sera of patients 1 day after autologous stem cell transplantation (auto-SCT), within the first 24 h with presentation of febrile neutropenia (0–24 h) and 48–72 h after first presentation with febrile neutropenia. Statistical significance was calculated with Kruskal-Wallis test in combination with Dunn’s multiple comparisons test (*p < 0.05; ****p < 0.0001)
Table 3 shows the sensitivity and specificity for CRP, IL-8, and PCT for developing a serious complication at cut-off values of 65 mg/l for CRP, 60 pg/ml for IL-8, and 0.5 ng/ml for PCT. These cut-off values were calculated based on the best sensitivity and specificity (Youden’s index), as well as according to the literature [25, 26]. For sTREM-1, no reasonable cut-off value could be calculated. The area under the curve demonstrated good individual power for IL-8 and PCT (0.808, 95% CI 0.625 to 0.992; 0.916, 95% CI 0.805 to 1.02) for developing a serious complication in FN. CRP demonstrated lower discriminatory power (0.7162, 95% CI 0.5415 to 0.8908). ROC curves were generated for CRP, IL-8, sTREM-1, and PCT for development of serious complications (Fig. 1a) and absence or presentation of bloodstream infection (Fig. 1b) at presentation with FN.
The analyses were broadened by constructing combinations between CRP, IL-8, and PCT. IL-8 in combination with PCT documented highly sensitive and specific results. The sensitivity for this combination was 90%, whereas specificity was 74%. The combination of CRP with IL-8 showed the highest sensitivity with 100%, but modest specificity with 47% (Table 4).
Discussion
Several studies have examined biomarkers for the identification of bacterial infections and critically ill patients. Most studies have been performed in non-neutropenic, adult patients. Nevertheless, a number of studies have demonstrated that neutropenic patients can produce a sufficient inflammatory response to release CRP, IL-8, and PCT [27,28,29]. These results are in line with our findings. In the present study, we further demonstrated that in patients with deep FN, measurement of sTREM-1 concentration is not useful to identify bacterial infections and critically ill patients. Our results in adult febrile neutropenia patients appear to be contrary to the pilot study of Kwofie et al. in 2012, who reported elevated levels of sTREM-1 in high-risk FN patients and proposed sTREM-1 as an alternative biomarker to PCT [30]. On closer examination of the FN patient characteristics in the study of Kwofie et al., mean total leukocyte count was more than ten times higher compared to our FN patients. In pediatric FN patients with similar leukocyte counts to our study population, sTREM-1 was mainly under the detection limit and also not considered as a potential biomarker [13]. It might be reasonable that measuring of sTREM-1 concentration for identifying critically ill or septic patients is depending on total leukocyte count. Unfortunately, we have not collected blood samples of patients during recovering of ANC and cannot add this aspect to the manuscript. Therefore, further studies with different leukocyte counts could decipher a cut-off value for reasonable measurements of sTREM-1 in daily routine. Additionally, it has to be mentioned that there is a lack of standardization for different sTREM-1 assays and concentration levels of different sTREM-1 assays might be difficult to compare [24].
In our study, PCT and IL-8 were the most favorable biomarkers for discrimination of critically ill patients. This finding is supported by recently published studies in critically ill neutropenic patients [31, 32]. CRP is commonly used in clinical practice and recommended as the only biomarker in the ESMO FN guidelines. However, in our study, CRP demonstrated to be the weakest biomarker for identifying critically ill patients in comparison to PCT and IL-8. In addition, we found that the combination of the biomarkers IL-8 and PCT might provide an opportunity to receive a highly sensitive and specific test to identify patients developing a serious infection.
Unfortunately, all tested biomarkers could not distinguish between bloodstream and no bloodstream infection. Among the tested biomarkers, PCT still showed best discrimination. In our study, we detected more positive blood cultures (63.6%) in comparison to other FN studies (20–30%) [33, 34]. The differences might be related to usage of antibiotic prophylaxis in almost half of these study patients compared to the absence of antibiotic prophylaxis in our study. The present bloodstream infections were predominantly due to gram-positive coagulase-negative Staphylococcus (CNS). In general, CNS isolated from blood cultures are associated with lower levels of inflammation compared with bloodstream infections because of gram-negative bacteria and are comparable with levels in patients with negative cultures [35]. Thus, PCT, IL-8, and CRP seem to be not or slightly changed due to CNS bloodstream infection in FN.
In conclusion, PCT might be the best biomarker for identifying critically ill patients with febrile neutropenia. In combination with an additional biomarker like IL-8, high sensitivity and specificity are achieved, while sTREM-1 is not a useful marker for the identification of critically ill patients in deep FN. Testing of PCT and/or IL-8 with CRP is a biomarker tool to define which FN patients are at high risk of developing serious complications in FN and need continuous monitoring. Further studies with more patients and in multiple centers are needed to evaluate whether PCT or IL-8 should be considered to be included in future FN guidelines.
References
Jantunen E et al (2006) Early treatment-related mortality in adult autologous stem cell transplant recipients: a nation-wide survey of 1482 transplanted patients. Eur J Haematol 76(3):245–250
Klastersky J et al (2016) Management of febrile neutropaenia: ESMO Clinical Practice Guidelines. Ann Oncol 27(suppl 5):v111–v118
Klastersky J, Paesmans M (2013) The Multinational Association for Supportive Care in Cancer (MASCC) risk index score: 10 years of use for identifying low-risk febrile neutropenic cancer patients. Support Care Cancer 21(5):1487–1495
Wu CW et al (2015) Does procalcitonin, C-reactive protein, or interleukin-6 test have a role in the diagnosis of severe infection in patients with febrile neutropenia? A systematic review and meta-analysis. Support Care Cancer 23(10):2863–2872
Hochreiter M et al (2009) Procalcitonin to guide duration of antibiotic therapy in intensive care patients: a randomized prospective controlled trial. Crit Care 13(3):R83
Nobre V et al (2008) Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomized trial. Am J Respir Crit Care Med 177(5):498–505
Lima SS et al (2016) Procalcitonin-guided protocol is not useful to manage antibiotic therapy in febrile neutropenia: a randomized controlled trial. Ann Hematol 95(7):1169–1176
Clec’h C et al (2004) Diagnostic and prognostic value of procalcitonin in patients with septic shock. Crit Care Med 32(5):1166–1169
Schneider CP et al (2009) Accuracy of procalcitonin for outcome prediction in unselected postoperative critically ill patients. Shock 31(6):568–573
Hatzistilianou M et al (2010) Procalcitonin as an early marker of bacterial infection in neutropenic febrile children with acute lymphoblastic leukemia. Inflamm Res 59(5):339–347
Engel A et al (2005) Interleukin-8 serum levels at fever onset in patients with neutropenia predict early medical complications. Infection 33(5–6):380–382
Stryjewski GR et al (2005) Interleukin-6, interleukin-8, and a rapid and sensitive assay for calcitonin precursors for the determination of bacterial sepsis in febrile neutropenic children. Pediatr Crit Care Med 6(2):129–135
Miedema KG et al (2011) The diagnostic value of CRP, IL-8, PCT, and sTREM-1 in the detection of bacterial infections in pediatric oncology patients with febrile neutropenia. Support Care Cancer 19(10):1593–1600
Bouchon A, Dietrich J, Colonna M (2000) Cutting edge: inflammatory responses can be triggered by TREM-1, a novel receptor expressed on neutrophils and monocytes. J Immunol 164(10):4991–4995
Lemarie J, Barraud D, Gibot S (2015) Host response biomarkers in sepsis: overview on sTREM-1 detection. Methods Mol Biol 1237:225–239
Su L, Xie L, Liu D (2015) Urine sTREM-1 may be a valuable biomarker in diagnosis and prognosis of sepsis-associated acute kidney injury. Crit Care 19:281
Rohde G et al (2012) Levels of soluble triggering receptor expressed on myeloid cells 1 in infectious exacerbations of chronic obstructive pulmonary disease. Respiration 83(2):133–139
Palazzo SJ, Simpson T, Schnapp LM (2012) Triggering receptor expressed on myeloid cells type 1 as a potential therapeutic target in sepsis. Dimens Crit Care Nurs 31(1):1–6
Gomez-Pina V et al (2007) Metalloproteinases shed TREM-1 ectodomain from lipopolysaccharide-stimulated human monocytes. J Immunol 179(6):4065–4073
Su L et al (2013) Diagnostic value of dynamics serum sCD163, sTREM-1, PCT, and CRP in differentiating sepsis, severity assessment, and prognostic prediction. Mediat Inflamm 2013:969875
Charles PE et al (2016) Significance of soluble triggering receptor expressed on myeloid cells-1 elevation in patients admitted to the intensive care unit with sepsis. BMC Infect Dis 16(1):559
Su L et al (2012) Value of soluble TREM-1, procalcitonin, and C-reactive protein serum levels as biomarkers for detecting bacteremia among sepsis patients with new fever in intensive care units: a prospective cohort study. BMC Infect Dis 12:157
Klastersky J et al (2000) The Multinational Association for Supportive Care in Cancer risk index: a multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol 18(16):3038–3051
Hasibeder A et al (2015) Evaluation and validation of the detection of soluble triggering receptor expressed on myeloid cells 1 by enzyme-linked immunosorbent assay. Sci Rep 5:15381
Tromp YH et al (2009) The predictive value of interleukin-8 (IL-8) in hospitalised patients with fever and chemotherapy-induced neutropenia. Eur J Cancer 45(4):596–600
Meisner M (2014) Update on procalcitonin measurements. Ann Lab Med 34(4):263–273
Uys A et al (2007) Prediction of outcome in cancer patients with febrile neutropenia: comparison of the Multinational Association of Supportive Care in Cancer risk-index score with procalcitonin, C-reactive protein, serum amyloid A, and interleukins-1beta, -6, -8 and -10. Eur J Cancer Care (Engl) 16(6):475–483
Prat C et al (2008) Evaluation of procalcitonin, neopterin, C-reactive protein, IL-6 and IL-8 as a diagnostic marker of infection in patients with febrile neutropenia. Leuk Lymphoma 49(9):1752–1761
Meidani M et al (2013) Procalcitonin and quantitative C-reactive protein role in the early diagnosis of sepsis in patients with febrile neutropenia. South Asian J Cancer 2(4):216–219
Kwofie L et al (2012) Evaluation of circulating soluble triggering receptor expressed on myeloid cells-1 (sTREM-1) to predict risk profile, response to antimicrobial therapy, and development of complications in patients with chemotherapy-associated febrile neutropenia: a pilot study. Ann Hematol 91(4):605–611
Reilly JP et al (2016) Neutropenic sepsis is associated with distinct clinical and biological characteristics: a cohort study of severe sepsis. Crit Care 20(1):222
Hong TH et al (2014) Biomarkers of early sepsis may be correlated with outcome. J Transl Med 12:146
Klastersky J et al (2007) Bacteraemia in febrile neutropenic cancer patients. Int J Antimicrob Agents 30(Suppl 1):S51–S59
Pinana JL et al (2014) Incidence, risk factors, and outcome of bacteremia following autologous hematopoietic stem cell transplantation in 720 adult patients. Ann Hematol 93(2):299–307
Rewa O et al (2012) Coagulase-negative Staphylococcus, catheter-related, bloodstream infections and their association with acute phase markers of inflammation in the intensive care unit: an observational study. Can J Infect Dis Med Microbiol 23(4):204–208
Acknowledgments
We would like to thank Andrea Drescher for the excellent technical support and Dr. Irene Schmidtmann (IMBEI, Mainz) for the statistical consulting service as well as the University Cancer Center (UCT) Mainz and German Cancer Consortium (DKTK) Frankfurt/Mainz.
Funding
This project was supported by the “Forschungszentrum Immunologie” (FZI) of the University Medical Center Mainz. The study was supported by the Department of Hematology, Medical Oncology, & Pneumology, University Medical Center of the Johannes Gutenberg University, Mainz, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Michel, C.S., Teschner, D., Wagner, E.M. et al. Diagnostic value of sTREM-1, IL-8, PCT, and CRP in febrile neutropenia after autologous stem cell transplantation. Ann Hematol 96, 2095–2101 (2017). https://doi.org/10.1007/s00277-017-3128-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-017-3128-1