Abstract
The anthracycline doxorubicin plays a major role in the treatment of lymphoproliferative disorders. However, its use is often limited due to cardiac toxicity, which seems to be much less in the liposomal non-pegylated formulation (Myocet®). The aim of this study was the evaluation of efficacy and toxicity of Myocet®-containing treatment regimens, with a focus on cardiotoxicity during treatment in lymphoma patients. A total of 326 consecutive patients, treated between March 2008 and December 2013 in 11 Austrian and 1 Italian cancer centers, were retrospectively assessed. Patients’ baseline and treatment-related parameters were obtained by reviewing hospital records. Median age was 74 years (range 26–93). The most common histology was DLBCL (60 %), followed by FL (13 %) and MCL (8 %). At least one cardiovascular comorbidity was present in 72 % of patients. Most common grade 3/4 toxicities were hematologic, namely, leukopenia, neutropenia, thrombocytopenia, and febrile neutropenia in 44, 40, 17, and 16 %. Overall, 43 patients suffered a cardiac event (any grade) with most patients developing congestive heart failure. Parameters significantly associated with severe cardiac events (grades 3–5) were the presence of cardiovascular comorbidities, chronic obstructive pulmonary disease, and elevated baseline NT-proBNP. Treatment response after first line Myocet®-containing therapy was ≥58 % among all entities (range 58–86 %) and therefore comparable to those of conventional therapeutic regimens. Herein, we provide a detailed toxicity profile of Myocet®-containing chemotherapy regimens. Despite the high rate of patients with preexisting comorbidities, the number of adverse events was encouraging. However, these results need to be confirmed in a prospective randomized trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-Hodgkin’s lymphoma (NHL) is the most common lymphoproliferative disorder. Since anthracyclines became available in 1969 with doxorubicin, the prognosis of many lymphomas has dramatically improved, especially when added to polychemotherapy regimens such as cyclophosphamide, vincristine and prednisolone (CHOP), and its variants (CHOP-like) [1]. However, especially in elderly patients, the use of doxorubicin is often limited due to anthracycline-induced cardiac toxicity [2–4]. These side effects often require dose reductions, treatment delays, or even omission of the anthracycline, leading to a dismal outcome [5]. Consequently, less toxic and equally potent options are needed.
Alternative formulations of doxorubicin, such as non-pegylated liposomal doxorubicin (Myocet®), with less cardiac side effects but preserved efficacy could represent an interesting alternative. Indeed, there is evidence that the ejection fraction, as a surrogate parameter for cardiac performance, is not affected by the administration of Myocet® [6–11]. A randomized controlled trial in patients affected by metastatic breast cancer showed comparable efficacy with less cardiac events when comparing Myocet® with doxorubicin (13 vs 29 %) [8]. Hence, Myocet® has also been administered off-label to many lymphoma and myeloma patients as a less toxic alternative to doxorubicin. Also, according to the guidelines of the European Society for Medical Oncology, substitution of doxorubicin by liposomal doxorubicin is recommended for patients with cardiac dysfunction or who are otherwise unfit [12]. Preliminary data regarding efficacy and toxicity in elderly patients with poor risk DLBCL showed a high response rate after the combination of rituximab, cyclophosphamide, Myocet®, and prednisone (R-COMP) with only a few treatment-related cardiac events [10, 11]. Even in patients with preexisting cardiac disorders, favorable results were observed [13]. However, real-live data of large patient cohorts assessing the efficacy and tolerability of Myocet®-containing treatment regimens is lacking. Therefore, we performed the so far largest multicenter observational study evaluating the spectrum and frequency of side effects and the efficacy of Myocet®-based chemotherapy in a real-life setting.
Patients and methods
Patients
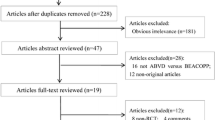
Eleven Austrian and one Italian cancer center retrospectively assessed all patients affected by a lymphoproliferative disease, who underwent a Myocet®-based treatment between March 2008 and December 2013. This resulted in a cohort of 326 consecutive, unselected patients. Patients’ characteristics at diagnosis (Table 1), chemotherapy details, toxicities (Tables 2 and 3, Supplementary Table 1), and outcome (Table 4, Figs. 1 and 2) were registered. Follow-up data was obtained from hospital files and primary physicians. The final data update was performed in January 2014. This study was approved by the Ethics Committee of the Medical University of Innsbruck.
This Kaplan–Meier plots illustrates progression-free survival (PFS) in five different lymphoma entities treated in first line with R-COMP (or COMP regimen in T-NHL). The median PFS and 3-year PFS were 44.3 months and 50 % in DLBCL (n = 166), respectively; 57.7 months and 62 % in follicular lymphoma grade 3 (FL G3, n = 21), respectively; not reached and 92 % in follicular lymphoma grades 1 and 2 respectively; 42.8 months and 68 % in mantle cell lymphoma (MCL, n = 18), respectively; and 6.9 months and 11 % in peripheral T cell lymphoma (T-NHL, n = 19)
This Kaplan–Meier plots illustrates overall survival (OS) in five different lymphoma entities treated in first line with R-COMP (or COMP regimen in T-NHL). The median OS and 3-year OS were not reached and 66 % in DLBCL (n = 166), respectively; 68.5 months and 75 % in follicular lymphoma grade 3 (FL G3, n = 21), respectively; not reached and 83 % in follicular lymphoma grades 1 and 2, respectively; not reached and 68 % in mantle cell lymphoma (MCL, n = 18), respectively; and 11.3 months and 23 % in peripheral T cell lymphoma (T-NHL, n = 19)
Treatment
All patients who received at least one Myocet®-containing therapy and met the above-mentioned criteria were included into this analysis. Most patients underwent R-COMP (cyclophosphamide 750 mg/m2, vincristine 2 mg, Myocet® 50 mg/m2, prednisone 40 mg/m2, and rituximab 375 mg/m2; n = 287). 19 T-NHL patients received COMP without rituximab. While a curative approach was intended in all cases, dose modifications, treatment delays, switches to another treatment regimen, and premature treatment termination were often necessary. Other treatment regimens containing Myocet® were the following: alemtuzumab plus COMP (three patients); bortezomib plus COMP (one patient); cyclophosphamide, vincristin, procarbazine, prednisone alternating with Myocet®, bleomycin, vinblastine, and dacarbazine (COPP-MBVD, one patient); ofatumumab plus COMP (one patient); bortezomib, Myocet®, and dexamethasone (ten patients); and cyclophosphamide, navelbine, Myocet®, prednisone (four patients). In accordance with the European Organisation for Research and Treatment of Cancer guidelines [14], granulocyte colony-stimulating factor (G-CSF) support was given in most cases.
Evaluation of toxicity
Toxicities, documented within the time interval between administration of first Myocet® dose and 2 months after the last dose of the respective therapy line, were graded according to the NCI Common Terminology Criteria for Adverse Events (CTCAE, version 4.0). Cardiotoxicity was documented during Myocet®-based therapy and at any time point thereafter. In order to better distinguish early from late onset cardiotoxicity, we categorized whether cardiotoxicity was experienced “during Myocet®-based therapy” (including the time interval of 2 months after last dose) or in the subsequent period (Table 3, Supplementary Table 1). To identify possible risk factors, the association of baseline characteristics and laboratory parameters with all cardiac events and cardiac events of grades 3–5 was analyzed. The following parameters were evaluated: sex, age (<60 vs ≥60 years), histology, stage of disease, performance status (ECOG ≤1 vs ≥2), presence or absence of B symptoms, international prognostic index (IPI), and comorbidities at times of diagnosis such as cardiovascular diseases, diabetes, chronic obstructive pulmonary disease (COPD), gastrointestinal disorders, rheumatic diseases, renal impairment, impaired cardiac function (ejection fraction [LVEF] <55 %), and prior cancers with or without prior antitumor therapies. Moreover, the following laboratory parameters were evaluated: hemoglobin level, count of leukocytes, neutrophils and thrombocytes, troponin T, NT-proBNP, C-reactive protein.
Evaluation of response and survival
Complete remission (CR) and partial remission (PR) were assessed according to the disease-specific response criteria [15–18]. In all cases, response had to persist for at least 2 months. Progression-free survival (PFS) was measured from first day of the Myocet®-based therapy to disease progression or death, whatever occurred first, and overall survival (OS) was measured from initiation of Myocet® therapy to last follow-up or death of any cause.
Statistical analyses
Chi-square test was performed to assess the significance of differences between categorical variables. The significance of distribution differences between subgroups was assessed with the Mann–Whitney U test. PFS and OS were plotted as a curve using the Kaplan–Meier method. Log-rank test was employed to assess the impact of categorical variables on survival. A P value of <0.05 was considered as statistically significant. All statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS) software v.17.0.1 (SPSS, Chicago, IL, USA).
Results
Patient characteristics at start of Myocet®-based therapy
Patient characteristics at start of Myocet®-based therapy are summarized in Table 1. Overall, most patients were of advanced age (median 74 years, range 26–93 years) and of male gender (58 %). Only the minority had a poor performance status (90/314 informative cases, 29 %). The most common lymphoproliferative disorder was DLBCL (n = 194; 60 %), followed by FL grade 3 (25; 8 %), MCL (24; 7 %), peripheral T-NHL (19; 6 %), and other lymphoma entities. Most patients presented with advanced stage of disease and adverse prognosticators (Table 1).
Treatment
Overall, the median cumulative Myocet® dose was 225 mg/m2 (20–400 mg/m2), and the median number of chemotherapy cycles containing Myocet® was 5 (range 1–8 cycles). In detail, in first line therapy, a median of 6 cycles of Myocet®-containing chemotherapy was administered (range 1–8) with an overall median cumulative dose of 240 mg/m2 (range 20–400 mg/m2). Seventy patients (21 %) received previous chemotherapy while 22 (7 %) were pretreated with radiotherapy (RT). In patients treated in higher lines, number of cycles (median 4, range 1–6) and cumulative Myocet® doses (150 mg/m2, 37.5–300 mg/m2) were significantly lower compared to the first line therapy (P < 0.001 for each comparison). There was no difference in numbers of cycles and cumulative dose in the different tumor entities, both in the first and higher line setting, respectively. In 21/326 patients (6 %), a switch from doxorubicin to Myocet® within a treatment line (after a median of 3 cycles, range 1–5 cycles) was performed. Of 1581 anthracycline-containing chemotherapies, 1494 contained Myocet® (95 %). RT within the same therapy line (mostly with intent of consolidation) was delivered to 31 patients (11 %).
Toxicity of Myocet®-based treatment
Hematologic and extrahematologic toxicities during Myocet®-based therapy and within 2 months after last dose, according to the CTC grades, are detailed in Table 2. As expected, the most common grade 3/4 toxicities were hematologic consisting mainly of leukopenia, neutropenia, thrombocytopenia, as well as febrile neutropenia in 142/326 (44 %), 131/326 (40 %), 55/326 (17 %), and 51/326 cases (16 %), respectively. Severe hematologic toxicities, including febrile neutropenia, were significantly more often observed in patients who had undergone a previous treatment line (neutropenia, 58 vs 36 %, P = 0.001; thrombocytopenia, 39 vs 12 %, P < 0.001; febrile neutropenia, 25 vs 13 %, P = 0.022). Non-hematologic toxicities were less frequent, but more often led to fatal events (n = 20).
A major focus was set on the detailed analysis of cardiac events occurring during treatment period (after the first dose of Myocet® until 2 months after the last dose). In Supplementary Table 1, the most important characteristics of patients who suffered cardiac events during a Myocet®-based therapy are described, including long-term follow-up information. Briefly, in 43/326 patients (13 %) a cardiac event was documented within the above-mentioned time period. Four patients experienced grade 3 toxicities, namely, clinically manifest congestive heart failure, accompanied with acute coronary syndrome in two cases, and 12 patients suffered from grade 4 toxicities consisting of severe congestive heart failure in 10 cases, myocardial infarction in one, and arrhythmia accompanied with an atrioventricular block of grade 3 in one patient. Therapy-associated cardiac deaths were documented in seven patients of whom four experienced a myocardial infarction leading to fatal congestive heart failure, two a sudden cardiac arrest, and one a fatal congestive heart failure during first cycle of a Myocet®-based therapy. All therapy-associated events of any grade are summarized in Table 3.
Parameters associated with elevated incidence of cardiac adverse events irrespective of grade were the presence of COPD (in 33 vs 10 % in patients without COPD, P < 0.001) and elevated NT-proBNP (20 vs 4 %, P = 0.05). Parameters associated with severe cardiac toxicity (grades 3–5) were the presence of cardiovascular comorbidity (9 vs 2 %, P = 0.035), COPD (19 vs 5 %, P = 0.002), and elevated NT-proBNP (15 vs 0 %, P = 0.04). The most homogeneous cohort in our observational trial was the group of DLBCL patients treated with R-COMP in first line (n = 149). A comparison of this cohort to historical cohorts who received conventional doxorubicin has recently been published [19]. Of note, the proportion of cardiotoxicity and severe cardiotoxicty in this group (including cardiac deaths) was not different when compared to the rest of patients (n = 177), who were characterized by varying patients’ characteristics, were partly pretreated, and often received different Myocet-based regimens.
Finally, cardiac events occurring >2 months after the last dose of Myocet® were documented in 18 cases (6 %), as detailed in Supplementary Table 1 and Table 3. In three of these patients, cardiotoxicitiy was also observed during Myocet®-based therapy. However, it is likely that in a relevant number of patients, cardiac events in the time after Myocet®-based therapy were not documented due to less frequent hospital visits after completion of chemotherapeutic treatment. Thus, no further analyses were perfomed in this cohort.
Response upon Myocet®-based therapy
Treatment response upon a Myocet®-based first line therapy according to the different histologic subtypes is summarized in Table 4. High overall response rates (ORR) were observed among all entities and were comparable to those of conventional therapies (e.g. of (R)-CHOP).
Overall, a response was achieved in 226/326 patients (ORR 69 %). Response in first line and higher line of therapy was achieved in 76 and 47 %, respectively (P < 0.001). Non-responders had significantly more often an elevated LDH (P < 0.001), poor performance status (P < 0.001), LVEF < 50 % (P = 0.001), elevated NT-proBNP (P = 0.014), and thrombocytopenia <150 G/L (P = 0.028) at time of treatment initiation.
Survival after start of Myocet®-based therapy
Survival analysis was performed in patients with Myocet®-based treatment in first line setting (n = 262). PFS was calculated only for the major histologic entities, namely, DLBCL (n = 166, 3 year PFS 50 %), FL grade 3 (n = 21, 3-year PFS 62 %), peripheral T-NHL (n = 19, 3-year PFS 11 %), MCL (n = 18, 3-year PFS 68 %), and FL grades 1–2 (n = 14, 3-year PFS 92 %) (Fig. 1). Apart from the type of lymphoproliferative disease, PFS was also negatively influenced by an elevated C-reactive protein (P < 0.001), unfavorable IPI in the case of aggressive B cell NHL (P < 0.001), low hemoglobin (P < 0.001), presence of B symptoms (P = 0.005), elevated ß2-microglobuline (P = 0.023), NT-proBNP (P = 0.029) above the upper normal value, and LVEF < 55 % (P = 0.047).
OS, again calculated in patients with Myocet® in first line, varied according to the different entities, and 3-year OS was 66 % for DLBCL (n = 166), 75 % for FL grade 3 (n = 21), 23 % for peripheral T-NHL (n = 19), 68 % for MCL (n = 18), and 83 % for FL grades 1–2 (n = 14) (Fig. 2). Survival was significantly influenced by an elevated C-reactive protein (P < 0.001), low hemoglobin (P < 0.001), unfavorable IPI in the case of aggressive B cell NHL (P < 0.001), LVEF < 55 % (P = 0.003), elevated NT-proBNP (P = 0.011), and the presence of B symptoms (P = 0.002).
Discussion
In our previous work, we retrospectively showed that R-COMP as first line chemo-immune therapy in DLBCL is efficacious and well tolerated when compared with R-CHOP; together with the Austrian prospective phase II data by Fridrik et al. [19, 20], it is convincingly demonstrated that R-COMP is able to cure patients with DLBCL, and its potential is comparable with the standard R-CHOP regimen. The reason for substituting classic doxorubicin by Myocet® is mainly to protect the heart from doxorubicin-associated acute and long-term cardiotoxicity. Nevertheless, Myocet® is licensed in combination with cyclophosphamide in metastatic breast cancer, and two large phase III studies as well as one meta-analysis evidenced that liposomal doxorubicin is less cardiotoxic than classic doxorubicin [7, 8]. Nevertheless, the authors of the meta-analysis concluded that the definitive recommendation in favor of liposomal formulations cannot be given so far [21]. On the other hand, the ESMO guidelines [12] suggest the substitution of doxorubicin with liposomal doxorubicin as option for patients with DLBCL and cardiac dysfunction. Apart from biological issues, several clinical questions still have to be answered: Can the favorable tolerability of Myocet® also be taken for granted in lymphoma? Should Myocet®-based therapy be reserved for the elderly and/or patients with preexisting cardiac comorbidities [22, 23]? Should it also be administered to the young patients facing a long lifetime after cure? Should Myocet® be given to all patients requiring a Doxorubicin-containing (immuno-) chemotherapy?
In this observational study, we put the focus on detailed analyses of toxicity and efficacy of Myocet®-based therapies in the so far largest cohort of patients affected by a hematologic neoplasia (n = 326). This enabled us to provide detailed subgroup analyses. However, due to the retrospective nature and the lack of a direct comparison to analogous therapies using classic doxorubicin, it cannot definitely be stated whether a Myocet®-based therapy is less cardiotoxic or not.
The pattern of acute, non-severe, and severe cardiac events in the present analysis reflected the expected spectrum of adverse events of an anthracycline-based therapy, such as congestive heart failure, arrhythmia, acute coronary syndrome, and even sudden cardiac death. Indeed, the quantity of cardiac events appears significant in our study. Nevertheless, it must be considered that the present study population is highly selected for preexisting cardiac comorbidities, representing patients in whom administration of conventional doxorubicin would have been contraindicated. Indeed, this might be an explanation for the high percentage of cardiovascular events occurring during Myocet® treatment. Long-term cardiovascular events in our study probably are underreported due to the retrospective study design with a considerable proportion of patients lost to follow-up. Anyhow, such an analysis certainly should be performed prospectively and demands a long, closely monitored observational period [24].
Maybe the most important finding in this study is the identification of factors predicting the occurrence of cardiac events. Herein, for the first time, baseline clinical parameters associated with Myocet®-associated cardiotoxicity were identified. Of all evaluated factors, cardiac comorbidities of any kind, elevated NT-proBNP and preexisting COPD, appeared to represent a state of elevated risk for cardiotoxicity under Myocet®-based therapy. Unexpectedly, impaired LVEF at treatment start did not unambiguously predict cardiotoxicity, in line with the observation by Jurzak et al. [25]. Nevertheless, early decline in LVEF was reported to predict cardiotoxicity in lymphoma patients [26]. The remaining parameters suggestive for a poor outcome, namely, increased age, poor performance status, anemia, and parameters indicative of advanced disease, such as high stage of disease or elevated LDH, did not favor the occurrence of cardiac events. Finally, cardiotoxicity was not increased in patients who were treated with a Myocet®-containing therapy in a higher line, i.e., after relapse in salvage therapy. Therefore, we recommend a complete cardiac workup including electrocardiography, echocardiography, spirometry, and determination of NT-proBNP before starting any kind of anthracycline-based therapy. Despite the herein reported favorable toxicity profile in patients with preexisting cardiac comorbidities, studies with a long-term follow-up to investigate whether this drug should be reserved to similar patients or if also others without such disorders might profit from Myocet® are urgently warranted. Indeed, data from breast cancer studies proved that liposomal doxorubicin is less cardiotoxic when compared prospectively to classic doxorubicin. Therefore, the use of Myocet®-based therapy would be of major importance in younger patients who have the chance of cure and an estimated rather long survival.
Other severe toxicities such as cytopenia, severe infections, and febrile neutropenia were frequent, but manageable in most cases. The number of adverse events was within the expected range, when compared to a phase II trial evaluating R-COMP in elderly DLBCL patients [27]. This observation certainly reflects the quality of our retrospective toxicity assessment.
Considering the accumulation of comorbidities in the presented cohort, response and cure rates are encouraging, suggesting that this treatment is a valid option for doxorubicin-unfit patients (Table 4; Figs. 1 and 2). Although this analysis was not powered to evaluate the response rate, the ORR of DLBCL patients after first line therapy was similar to the one reported by Luminari et al. [27] (ORR 71 % as compared to 75 % in our study) and others [19, 22]. However, PFS and OS seem slightly inferior in our cohort, certainly explained due to the inferior basic characteristics. Nevertheless, patients who received ≥300 mg/m2 Myocet® had a 3-year OS close to 80 % (not shown in detail).
In conclusion, in this real-life patient setting, we characterized in detail the spectrum of cardiotoxicities which can occur during a Myocet®-based therapy in lymphoma, identified prognosticators for such events, and showed that these treatments offer a reasonable chance of cure. However, a definite superiority of Myocet® in terms of toxicity and/or efficacy can only be demonstrated in prospective trials comparing Myocet®-containing regimens to the actual standard of care for each entity.
References
Fisher RI, Gaynor ER, Dahlberg S, Oken MM, Grogan TM, Mize EM, Glick JH, Coltman CA Jr, Miller TP (1993) Comparison of a standard regimen (CHOP) with three intensive chemotherapy regimens for advanced non-Hodgkin’s lymphoma. N Engl J Med 328(14):1002–1006. doi:10.1056/NEJM199304083281404
Coiffier B, Thieblemont C, Van Den Neste E, Lepeu G, Plantier I, Castaigne S, Lefort S, Marit G, Macro M, Sebban C, Belhadj K, Bordessoule D, Ferme C, Tilly H (2010) Long-term outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the Groupe d’Etudes des Lymphomes de l’Adulte. Blood 116(12):2040–2045. doi:10.1182/blood-2010-03-276246
Green M (1998) Anthracycline cardiotoxicity, no longer an issue? Ann Oncol Off J Eur Soc Med Oncol / ESMO 9(7):691–693
Limat S, Demesmay K, Voillat L, Bernard Y, Deconinck E, Brion A, Sabbah A, Woronoff-Lemsi MC, Cahn JY (2003) Early cardiotoxicity of the CHOP regimen in aggressive non-Hodgkin’s lymphoma. Ann Oncol Off J Eur Soc Med Oncol / ESMO 14(2):277–281
Dixon DO, Neilan B, Jones SE, Lipschitz DA, Miller TP, Grozea PN, Wilson HE (1986) Effect of age on therapeutic outcome in advanced diffuse histiocytic lymphoma: the Southwest Oncology Group experience. J Clin Oncol Off J Am Soc Clin Oncol 4(3):295–305
Allen TM, Martin FJ (2004) Advantages of liposomal delivery systems for anthracyclines. Semin Oncol 31(6 Suppl 13):5–15
Batist G, Ramakrishnan G, Rao CS, Chandrasekharan A, Gutheil J, Guthrie T, Shah P, Khojasteh A, Nair MK, Hoelzer K, Tkaczuk K, Park YC, Lee LW (2001) Reduced cardiotoxicity and preserved antitumor efficacy of liposome-encapsulated doxorubicin and cyclophosphamide compared with conventional doxorubicin and cyclophosphamide in a randomized, multicenter trial of metastatic breast cancer. J Clin Oncol Off J Am Soc Clin Oncol 19(5):1444–1454
Harris L, Batist G, Belt R, Rovira D, Navari R, Azarnia N, Welles L, Winer E, Group TDS (2002) Liposome-encapsulated doxorubicin compared with conventional doxorubicin in a randomized multicenter trial as first-line therapy of metastatic breast carcinoma. Cancer 94(1):25–36
van Dalen EC, Michiels EM, Caron HN, Kremer LC (2010) Different anthracycline derivates for reducing cardiotoxicity in cancer patients. Cochrane Database Syst Rev 5, CD005006. doi:10.1002/14651858.CD005006.pub4
Dell’Olio M, Scalzulli RP, Sanpaolo G, Nobile M, Mantuano FS, La Sala A, D’Arena G, Miraglia E, Lucania A, Mastrullo L, Nicola C (2011) Non-pegylated liposomal doxorubicin (Myocet(R)) in patients with poor-risk aggressive B-cell non-Hodgkin lymphoma. Leuk Lymphoma 52(7):1222–1229. doi:10.3109/10428194.2011.572321
Corazzelli G, Frigeri F, Arcamone M, Lucania A, Rosariavilla M, Morelli E, Amore A, Capobianco G, Caronna A, Becchimanzi C, Volzone F, Marcacci G, Russo F, De Filippi R, Mastrullo L, Pinto A (2011) Biweekly rituximab, cyclophosphamide, vincristine, non-pegylated liposome-encapsulated doxorubicin and prednisone (R-COMP-14) in elderly patients with poor-risk diffuse large B-cell lymphoma and moderate to high ‘life threat’ impact cardiopathy. Br J Haematol 154(5):579–589. doi:10.1111/j.1365-2141.2011.08786.x
Tilly H, Vitolo U, Walewski J, da Silva MG, Shpilberg O, Andre M, Pfreundschuh M, Dreyling M, Group EGW (2012) Diffuse large B-cell lymphoma (DLBCL): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol Off J Eur Soc Med Oncol / ESMO 23(Suppl 7):vii78–vii82. doi:10.1093/annonc/mds273
Heintel D, Skrabs C, Hauswirth A, Eigenberger K, Einberger C, Raderer M, Sperr WR, Knobl P, Mullauer L, Uffmann M, Dieckmann K, Gaiger A, Jager U (2010) Nonpegylated liposomal doxorubicin is highly active in patients with B and T/NK cell lymphomas with cardiac comorbidity or higher age. Ann Hematol 89(2):163–169. doi:10.1007/s00277-009-0796-5
Aapro MS, Bohlius J, Cameron DA, Dal Lago L, Donnelly JP, Kearney N, Lyman GH, Pettengell R, Tjan-Heijnen VC, Walewski J, Weber DC, Zielinski C, European Organisation for R, Treatment of C (2011) 2010 update of EORTC guidelines for the use of granulocyte-colony stimulating factor to reduce the incidence of chemotherapy-induced febrile neutropenia in adult patients with lymphoproliferative disorders and solid tumours. Eur J Cancer 47(1):8–32. doi:10.1016/j.ejca.2010.10.013
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, Lister TA, Vose J, Grillo-Lopez A, Hagenbeek A, Cabanillas F, Klippensten D, Hiddemann W, Castellino R, Harris NL, Armitage JO, Carter W, Hoppe R, Canellos GP (1999) Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J Clin Oncol Off J Am Soc Clin Oncol 17(4):1244
Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Dohner H, Hillmen P, Keating MJ, Montserrat E, Rai KR, Kipps TJ, International Workshop on Chronic Lymphocytic L (2008) Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood 111(12):5446–5456. doi:10.1182/blood-2007-06-093906
Kyle RA, Rajkumar SV (2014) Criteria for diagnosis, staging, risk stratification and response assessment of multiple myeloma. Leukemia 28(4):980. doi:10.1038/leu.2014.11
Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, Coiffier B, Fisher RI, Hagenbeek A, Zucca E, Rosen ST, Stroobants S, Lister TA, Hoppe RT, Dreyling M, Tobinai K, Vose JM, Connors JM, Federico M, Diehl V, International Harmonization Project on L (2007) Revised response criteria for malignant lymphoma. J Clin Oncol Off J Am Soc Clin Oncol 25(5):579–586. doi:10.1200/JCO.2006.09.2403
Mian M, Wasle I, Gamerith G, Mondello P, Melchardt T, Jager T, Linkesch W, Fiegl M (2014) R-CHOP versus R-COMP: are they really equally effective? Clin Oncol. doi:10.1016/j.clon.2014.05.012
Fridrik MA, Petzer AL, Keil F, Willenbacher W, Jaeger U, Lang A, Burgstaller S, Andel J, Krieger O, Oberaigner W, Greil R (2011) Non-pegylated liposomal encapsulated doxorubicin reduces cardiotoxicity in 1st line treatment of diffuse large B-Cell lymphoma (DLBCL). Final results of a randomized trial. ASH annual. Meet Abstr 118(21):2676
Smith LA, Cornelius VR, Plummer CJ, Levitt G, Verrill M, Canney P, Jones A (2010) Cardiotoxicity of anthracycline agents for the treatment of cancer: systematic review and meta-analysis of randomised controlled trials. BMC Cancer 10:337. doi:10.1186/1471-2407-10-337
Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, Morel P, Van Den Neste E, Salles G, Gaulard P, Reyes F, Lederlin P, Gisselbrecht C (2002) CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346(4):235–242. doi:10.1056/NEJMoa011795
Hershman DL, McBride RB, Eisenberger A, Tsai WY, Grann VR, Jacobson JS (2008) Doxorubicin, cardiac risk factors, and cardiac toxicity in elderly patients with diffuse B-cell non-Hodgkin’s lymphoma. J Clin Oncol Off J Am Soc Clin Oncol 26(19):3159–3165. doi:10.1200/JCO.2007.14.1242
Bovelli D, Plataniotis G, Roila F, Group EGW (2010) Cardiotoxicity of chemotherapeutic agents and radiotherapy-related heart disease: ESMO Clinical Practice Guidelines. Ann Oncol Off J Eur Soc Med Oncol / ESMO 21(Suppl 5):v277–v282. doi:10.1093/annonc/mdq200
Jurczak W, Szmit S, Sobocinski M, Machaczka M, Drozd-Sokolowska J, Joks M, Dzietczenia J, Wrobel T, Kumiega B, Zaucha JM, Knopinska-Posluszny W, Spychalowicz W, Prochwicz A, Drohomirecka A, Skotnicki AB (2013) Premature cardiovascular mortality in lymphoma patients treated with (R)-CHOP regimen—a national multicenter study. Int J Cardiol 168(6):5212–5217. doi:10.1016/j.ijcard.2013.08.033
Nousiainen T, Jantunen E, Vanninen E, Hartikainen J (2002) Early decline in left ventricular ejection fraction predicts doxorubicin cardiotoxicity in lymphoma patients. Br J Cancer 86(11):1697–1700. doi:10.1038/sj.bjc.6600346
Luminari S, Montanini A, Caballero D, Bologna S, Notter M, Dyer MJ, Chiappella A, Briones J, Petrini M, Barbato A, Kayitalire L, Federico M (2010) Nonpegylated liposomal doxorubicin (MyocetTM) combination (R-COMP) chemotherapy in elderly patients with diffuse large B-cell lymphoma (DLBCL): results from the phase II EUR018 trial. Ann Oncol Off J Eur Soc Med Oncol / ESMO 21(7):1492–1499. doi:10.1093/annonc/mdp544
Acknowledgments
The authors thank Stephan Gritsch (Innsbruck), August Zabernigg (Kufstein), Reinhard Stauder (Innsbruck), Wolfgang Willenbacher (Innsbruck), Michael Steurer (Innsbruck), Günther Gastl (Innsbruck), Günther Zangerl (Zams), Michael Schnallinger (St. Johann) and Stephan Schreieck (Reutte), for providing patient data and advice.
Conflict of interest
This study was supported by the “Verein für Tumorforschung.” Ines Wasle, PhD student, received an unrestricted research grant by the Austrian Ratiopharm Arzneimittel Vertriebs-GmbH. Michael Fiegl received honoraria for lectures (Roche, TEVA). Michael Fiegl and Michael Mian are consultants of TEVA.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
(DOCX 33 kb)
Rights and permissions
About this article
Cite this article
Wasle, I., Gamerith, G., Kocher, F. et al. Non-pegylated liposomal doxorubicin in lymphoma: patterns of toxicity and outcome in a large observational trial. Ann Hematol 94, 593–601 (2015). https://doi.org/10.1007/s00277-014-2250-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-014-2250-6