Abstract
Purpose
To review variations regarding the branching patterns of the superficial fibular nerve (SFN) concerning the deep fascia of leg and to the ankle joint level.
Methods
Searches were conducted in PubMed, Scopus, Lilacs, and Web of Science databases on October 14th, 2021. We followed the PRISMA guidelines to report this review. Articles with data on SFN variations prevalence were included. The data were extracted and pooled into a meta-analysis. We also dissected 60 formalin-fixed Brazilian fetuses (n = 120 lower limbs).
Results
Twenty-five studies (n = 1272 lower limbs) comprised this review. Concerning the SFN branching at the deep fascia, Type 1 variation (in which the SFN pierces the fascia as a single nerve trunk) had a pooled prevalence of 86.4% (95% CI 84.5–88.2), while Type 2 had a pooled prevalence of 13.6% (95% CI 11.8–15.5). At the ankle joint level, Type 2 variation (in which the SFN branches off below the joint level) was the most common anatomical pattern, with a pooled prevalence of 78.7% (95% CI 74.5–82.7).
Conclusion
Typically, the SFN branches off between its exit from the deep fascia and the ankle joint level. The SFN variations have great importance for surgeries, such as arthroscopies and fascia release surgeries, regional anesthesia, and clinical evaluation of SFN entrapment syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The superficial fibular nerve (SFN) provides motor inputs to the fibularis longus and fibularis brevis muscles [16] and sensibility outputs of the anterolateral leg and dorsum of the foot [9]. The SFN arises from the branching of the common fibular nerve [38], travels through the lateral compartment of the leg [34], and reaches the dorsum of the foot after piercing the deep fascia of the leg to divide into two branches: the medial dorsal cutaneous (MDCN) and intermediate dorsal cutaneous (IDCN) nerves.
Regarding SFN variations, previous studies have reported many variations in SFN branching at the deep fascia and ankle joint level, which affect leg and foot surgeries. Knowing the SFN anatomy is essential to avoid SFN injury during ankle arthroscopy [3, 39], and injury to one of the terminal branches of SFN can lead to loss of leg skin sensation and chronic pain in the dorsum of foot [9]. In addition, possible unexpected nerve variations may impair regional anesthesia in the foot and leg; hence, incomplete or unsuccessful nerve blockades may occur, which inflict pain on the patients and prolong recovery time [6].
The branching patterns of SFN are relevant for clinical and surgical purposes; therefore, the present paper aims to provide a comprehensive, evidence-based systematic review with a meta-analysis and an original cadaver study on this topic.
Materials and methods
Meta-analysis
Register and guidelines
Our review protocol review was approved by the International Prospective Register of Systematic Reviews (registry code: CRD42020207050). We conducted the present review in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [21] and the guidelines by the International Evidence-Based Anatomy Working Group (iEBA-WG) [12].
Search strategy
The data were obtained from a literature survey on October 14th, 2021, in the PubMed, Scopus, Lilacs, and Web of Science databases. The searches in all electronic databases comprised combinations of the keywords “superficial peroneal nerve”, “superficial fibular nerve”, “anatomy”, and “anatomical variation”. No restrictions were imposed on the publication year, language, and study design. Reference lists of relevant articles were also searched.
Eligibility assessment
Two review authors examined the retrieved records for eligibility and solved disagreements via consensus. Anatomical studies on the SFN anatomy with no distinction of design or anatomical evaluation method (e.g., magnetic resonance imaging, ultrasound, intraoperative, and dissection) were deemed eligible for inclusion. Reviews, book chapters, conference abstracts, case reports or case series, and studies outside the review’s scope were excluded after the reading of abstracts and full-text texts.
Data extraction
Two review authors extracted the following data from the primary studies: first authors’ surname, location where the study was conducted, publication year, sample size, and amount of variations found in the study. In the present review, we evaluated the SFN branching in the leg (first variable) and ankle (second variable).
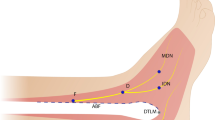
With respect to the SFN branching patterns in the leg, we classified the variations in the following way: Type 1, the SFN branches off after piercing the deep fascia; Type 2, the SFN branches off before piercing the deep fascia (Fig. 1).
With regard to the SFN branching patterns at the ankle joint level, the following classification system by Takao et al. [33] was adopted: Type 1, both the MDCN and IDCN branch off distal to the joint level; Type 2, the SFN branches off proximal to the joint, but its terminal nerves branches off distal to it; Type 3, the IDCN branches off proximal to the joint, but the MDCN branches off distal to it; Type 4, the MDCN branches off proximal to the joint, but the IDCN branches off distal to it; Type 5, both the MDCN and IDCN branch off proximal to the joint level (Fig. 1).
Statistical analysis
The present meta-analysis of prevalence was performed based on the random-effects model, with a 95% confidence interval (95% CI) and Freeman–Tukey double arcsine transformation [10, 19]. We used MetaXL software to analyze the data [4].
Cochran’s Q test and Higgins’s I2 statistic were adopted to measure the heterogeneity among the primary studies. Subgroup analyses were performed by means of the Chi-square test to assess whether the geographical location influences SFN anatomy. P values of less than 0.05 were deemed statistically significant.
Anatomical study
Sample characteristics
We included fetuses aged from the fourth to the ninth months of conception without neural or non-neural deformities in their lower limbs. The fetuses were obtained from cadaver donation programs for anatomy research at our university. Sixty formalin-fixed Brazilian fetal cadaver specimens (n = 120 lower limbs), of which 30 were male and 30 were female, were used in this anatomical study. The race of the included fetuses could not be determined because of the tissue wasting caused by formaldehyde.
Dissection method
We dissected the anterior aspect of the leg and foot to expose the SFN branching (Fig. 2). We used No. 15 surgical scalpel blades and Metzenbaum scissors. The data were later collected and classified for further analysis, as well as stored by means of a photographic record.
Ethical considerations
We state every effort was made to follow all local and international ethical guidelines and laws regarding using human cadaveric donors in anatomical research, as recommended by Iwanaga et al. [15]. Ethical approval from the local Human Research Ethics Committee is included at the end of the paper.
Results
Identification of studies
Figure 3 displays the article identification process. A total of 827 records were retrieved from the searched electronic databases. After removing duplicates, 720 records were analyzed, of which 57 were deemed potentially eligible after reading titles. Thirty-three studies were excluded in compliance with the exclusion criteria. Twenty-four studies were included after the selection process.
Characteristics of included studies
Twenty-four studies were selected by means of the article identification process [1, 2, 5,6,7,8,9, 13, 17, 18, 22,23,24,25,26,27,28,29,30,31, 33, 35,36,37]. Considering the current cadaveric study, 25 studies composed the meta-analysis (n = 1272 lower limbs). The characteristics of the included studies are summarized in Table 1.
Results of the current cadaveric study
There was no statistically significant association between the side of the lower limb (p = 0.327) or sex of the fetuses (p = 0.142), with the variations in SFN branching when this nerve pierces the deep fascia. With regard to the SFN branching at the ankle joint level, no statistically significant association was found in terms of lower limb side (p = 0.834) and sex of the fetuses (p = 0.545). The prevalence of the variations was pooled in the meta-analysis displayed on forest plots. Results of the dissections are presented in Table 2.
SFN branching patterns concerning the deep fascia
Twenty-five studies reported data on the SFN branching at the deep fascia (n = 1272 lower limbs). In the overall analysis, Type 1 was the most common pattern (86.4%; 95% CI 84.5–88.2; I2 = 92.3%; p < 0.0001). Type 2 was the least common (13.6%; 95% CI 11.8–15.5; I2 = 92.3%; p < 0.0001). Table 3 shows the subgroup analysis for this variable. A statistically significant association was found between geographical subgroups and variations for the SFN branching patterns (p < 0.001), demonstrating unequal distribution among the geographical subgroups.
SFN branching patterns concerning the ankle joint level
Six studies reported data on the SFN branching at the ankle joint level (n = 389 lower limbs). In the overall analysis, Type 2 was the most common variation (61.0%; 95% CI 56.0–65.7; I2 = 49%; p = 0.08), followed by Type 1 (21.4%; 95% CI 17.3–25.5; I2 = 0%; p = 0.43) and Type 3 (9.4%; 95% CI 6.6–12.4, I2 = 0%; p = 0.47). Type 4 (5.5%; 95% CI 3.3–7.8, I2 = 78%; p < 0.01) and Type 5 (2.7%; 95% CI 1.2–4.4, I2 = 59%; p = 0.03) were the least commons. Table 4 shows the subgroup analysis. No significant differences were found among the geographical subgroups (p < 0.212).
Discussion
The present systematic review study aimed to assess the SFN anatomy. The existence and pooled prevalence of two SFN branching patterns in relation to the deep fascia and five branching patterns concerning the ankle joint level have been reported throughout this study. Knowing these anatomical variations have great importance to avoid iatrogenic injuries to this nerve in ankle and leg surgeries and for the proper performance of regional anesthesia on the leg and foot.
The SFN is the most commonly injured structure in ankle arthroscopy because of its high anatomical variability [3, 20, 39]. Considering the ankle joint level, Type 1 and Type 3 anatomies were more prevalent in Asian populations (26% and 12.4%, respectively), while Type 2 was more common in South American populations (69%). Type 4 was most prevalent in populations from Oceania (17.5%), and Type 5 was most common in populations from North America (10.2%). We found significant differences among the geographical groups. These data may show the need for caution when performing surgical procedures since the SFN anatomy may vary by geography.
Variations in SFN anatomy can lead to SFN entrapment syndrome, which may occur when the SFN is compressed by the deep fascia when piercing it to become subcutaneous in the distal leg [14, 18, 32]. The SFN anatomy influences the symptomatology and therapy of SFN entrapment. Subgroup analysis showed Type 1 was more prevalent in all geographical subgroups, with significant differences among all subgroups. These data may alert to the surgical precautions for patients from different geographical subgroups undergoing fascia release surgery.
Although SFN is still underused for nerve grafts [37], this is one of the best clinical and surgical uses of this nerve [18, 26]. SFN provides a lengthy graft and also has a relatively foreseeable course. Further, the SFN may be harvested without major problems for the donor because the lack of its sensory portion only affects the sensitivity of the dorsum of foot [26]. Knowing the different SFN branching types ensures better use of the nerve and may prevent injuries in the branches involved in the harvest of SFN [26]. Electroneuromyography tests may be used as non-invasive clinical assessment of possible SFN variations [11]. The preoperative use of these tests can avoid iatrogenic injuries to SFN.
Imaging examinations may be used to assess the SFN anatomy, and ultrasonography is particularly useful [6, 7]. However, some comorbidities, such as morbid obesity, arteriopathies, or heart failure may cause image obstruction by excess tissue or subcutaneous fluid. Knowing the SFN branching variations becomes more relevant in these cases. The principal use of this ultrasound-applied information is during SFN blocks. Patients with these comorbidities derive the greatest benefit from using regional anesthesia, which avoids the potential complications of general anesthesia. Clinical and surgical experience has shown the relevance of knowing the SFN location and branching to treat diseases, syndromes, or injuries [6].
The absence of detailed descriptions of the ethnicities of the primary study subjects limited the present study. This restricted us to a geographical subgroup analysis, which is not as important clinically or surgically as an ethnicity-based analysis. Moreover, detailed descriptions with regard to sex and side were not provided, which also limited our analyses.
The present review found statistically significant differences in the distribution of nerve variations, which are important from a clinical and surgical viewpoint. Due to the possibility of unforeseen variations, the surgeon and anesthesiologist need to carefully analyze the SFN branching.
Data availability
Not applicable.
References
Adkison DP, Bosse MJ, Gaccione DR, Gabriel KR (1991) Anatomical variations in the course of the superficial peroneal nerve. J Bone Jt Surg 73:112–114
Agthong S, Huanmanop T, Sasivongsbhakdi T, Ruenkhwan K, Piyawacharapun A, Chentanez V (2008) Anatomy of the superficial peroneal nerve related to the harvesting for nerve graft. Surg Radiol Anat 30:145–148. https://doi.org/10.1007/s00276-007-0296-z
Ahn JH, Park D, Park YT, Park J, Kim YC (2019) What should we be careful of ankle arthroscopy? J Orthop Surg 27:1–9. https://doi.org/10.1177/2309499019862502
Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T (2013) Meta-analysis of prevalence. J Epidemiol Community Health 67:974–978. https://doi.org/10.1136/jech-2013-203104
Blair JM, Botte MJ (1994) Surgical anatomy of the superficial peroneal nerve in the ankle and foot. Clin Orthop Relat Res 1:229–238
Bowness J, Turnbull K, Taylor A, Halcrow J, Chisholm F, Grant C, Varsou O (2019) Identifying the emergence of the superficial peroneal nerve through deep fascia on ultrasound and by dissection: Implications for regional anesthesia in foot and ankle surgery. Clin Anat 32:390–395. https://doi.org/10.1002/ca.23323
Canella C, Demondion X, Guillin R, Boutry N, Peltier J, Cotten A (2009) Anatomic study of the superficial peroneal nerve using sonography. Am J Roentgenol 193:174–179. https://doi.org/10.2214/AJR.08.1898
Canovas F, Bonnel F, Kouloumdjian P (1996) The superficial peroneal nerve at the foot. Organisation, surgical applications. Surg Radiol Anat 18:241–244
Darland AM, Kadakia AR, Zeller JL (2015) Branching patterns of the superficial peroneal nerve: implications for ankle arthroscopy and for anterolateral surgical approaches to the ankle. J Foot Ankle Surg 54:332–337. https://doi.org/10.1053/j.jfas.2014.07.002
Freeman MF, Tukey JW (1950) Transformations Related to the Angular and the Square Root. Ann Math Stat 21:607–611. https://doi.org/10.1214/aoms/1177729756
Hemmi S, Kurokawa K, Nagai T, Kushida R, Okamoto T, Murakami T, Sunada Y (2017) Variations in the distal branches of the superficial fibular sensory nerve. Muscle Nerve 55:74–76. https://doi.org/10.1002/mus.25196
Henry BM, Tomaszewski KA, Walocha JA (2016) Methods of evidence-based anatomy: a guide to conducting systematic reviews and meta-analysis of anatomical studies. Ann Anat 205:16–21. https://doi.org/10.1016/j.aanat.2015.12.002
Herron M, Langkamer VG, Atkins RM (1993) The anatomical variations of the distal course of the superficial peroneal nerve: recommendations to avoid injury during surgical procedures. Foot 3:38–42. https://doi.org/10.1016/0958-2592(93)90029-3
Hirose CB, McGarvey WC (2004) Peripheral nerve entrapments. Foot Ankle Clin 9:255–269. https://doi.org/10.1016/j.fcl.2004.02.001
Iwanaga J, Singh V, Takeda S, Ogeng’o J, Kim H-J, Moryś J, Ravi KS, Ribatti D, Trainor PA, Sañudo JR, Apaydin N, Sharma A, Smith HF, Walocha JA, Hegazy AMS, Duparc F, Paulsen F, Del Sol M, Adds P, Louryan S, Fazan VPS, Boddeti RK, Tubbs RS (2022) Standardized statement for the ethical use of human cadaveric tissues in anatomy research papers: Recommendations from Anatomical Journal Editors-in-Chief. Clin Anat 35:526–528. https://doi.org/10.1002/ca.23849
Karykowska A, Rohan-Fugiel A, Mączka G, Grzelak J, Gworys B, Tarkowski V, Domagała Z (2021) Topography of muscular branches of the superficial fibular nerve based on anatomical preparation of human foetuses. Ann Anat - Anat Anzeiger 237:151728. https://doi.org/10.1016/j.aanat.2021.151728
Kosinski C (1926) The Course, Mutual Relations and Distribution of the Cutaneous Nerves of the Metazonal Region of Leg and Foot. J Anat 60:274–297
Kurtoglu Z, Aktekin M, Uluutku MH (2006) Branching patterns of the common and superficial fibular nerves in fetus. Clin Anat 19:621–626. https://doi.org/10.1002/ca.20235
Lin L, Xu C (2020) Arcsine-based transformations for meta-analysis of proportions: Pros, cons, and alternatives. Heal Sci Reports 3:e178. https://doi.org/10.1002/hsr2.178
Malagelada F, Vega J, Guelfi M, Kerkhoffs G, Karlsson J, Dalmau-Pastor M (2020) Anatomic lectures on structures at risk prior to cadaveric courses reduce injury to the superficial peroneal nerve, the commonest complication in ankle arthroscopy. Knee Surgery, Sport Traumatol Arthrosc 28:79–85. https://doi.org/10.1007/s00167-019-05373-x
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Ogüt T, Akgün I, Kesmezacar H, Türker T, Uzün I, Demirci S, Marur T, Can G, Akkin SM (2004) Navigation for ankle arthroscopy: anatomical study of the anterolateral portal with reference to the superficial peroneal nerve. Surg Radiol Anat 26:268–274. https://doi.org/10.1007/s00276-004-0231-5
Olave E, Galaz C, Retamal P, Cruzat C (2011) División Alta del Nervio Fibular Superficial: Origen Precoz de los Nervios Cutáneos Dorsales del Pie. Int J Morphol 29:436–440
Pacha D, Carrera A, Llusa M, Permanyer E, Molona O, Morro R (2003) Clinical anatomy of the superficial peroneal nerve in the distal leg. Eur J Anat 7:15–20
Prakash BAK, Singh DK, Rajini T, Jayanthi V, Singh G (2010) Anatomic variations of superficial peroneal nerve: clinical implications of a cadaver study. Ital J Anat Embryol 115:223–228
Ribak S, Fonseca JR, Tietzmann A, Gama SAM, Hirata HH (2016) The anatomy and morphology of the superficial peroneal nerve. J Reconstr Microsurg 32:271–275. https://doi.org/10.1055/s-0035-1568881
Rodríguez-Lorenzo A, Gago B, Pineda AF, Bhatti M, Audolfsson T (2011) Superficial peroneal and sural nerve transfer to tibial nerve for restoration of plantar sensation after complex injuries of the tibial nerve: cadaver feasibility study. J Plast Reconstr Aesthetic Surg 64:1512–1516. https://doi.org/10.1016/j.bjps.2011.05.027
Saito A, Kikuchi S (1998) Anatomic relations between ankle arthroscopic portal sites and the superficial peroneal and saphenous nerves. Foot Ankle Int 19:748–752. https://doi.org/10.1177/107110079801901107
Şayli U, Tekdemyr Y, Çubuk HE, Avci S, Tüccar E, Elhan HA, Uz A (1998) The course of the superficial peroneal nerve: An anatomical cadaver study. Foot Ankle Surg 4:63–69. https://doi.org/10.1046/j.1460-9584.1998.00085.x
Solomon LB, Ferris L, Henneberg M (2006) Anatomical study of the ankle with view to the anterior arthroscopic portals. ANZ J Surg 76:932–936. https://doi.org/10.1111/j.1445-2197.2006.03909.x
Solomon LB, Ferris L, Tedman R, Henneberg M (2001) Surgical anatomy of the sural and superficial fibular nerves with an emphasis on the approach to the lateral malleolus. J Anat 199:717–723. https://doi.org/10.1046/j.1469-7580.2001.19960717.x
Sridhara CR, Izzo KL (1985) Terminal sensory branches of the superficial peroneal nerve: an entrapment syndrome. Arch Phys Med Rehabil 66:789–791
Takao M, Uchio Y, Shu N, Ochi M (1998) Anatomic bases of ankle arthroscopy: study of superficial and deep peroneal nerves around anterolateral and anterocentral approach. Surg Radiol Anat 20:317–320. https://doi.org/10.1007/BF01630612
Tzika M, Paraskevas G, Natsis K (2015) Entrapment of the superficial peroneal nerve: an anatomical insight. J Am Podiatr Med Assoc 105:150–159. https://doi.org/10.7547/0003-0538-105.2.150
Ucerler H, Ikiz ’Z Asli Aktan, (2005) The variations of the sensory branches of the superficial peroneal nerve course and its clinical importance. Foot Ankle Int 26:942–946. https://doi.org/10.1177/107110070502601108
Ucerler H, Ikiz AA, Uygur M (2007) A cadaver study on preserving peroneal nerves during ankle arthroscopy. Foot Ankle Int 28:1172–1178. https://doi.org/10.3113/FAI.2007.1172
Wahee P, Aggarwal A, Harjeet K, Sahni D (2010) Surgical anatomy of sensory portion of superficial fibular nerve for harvesting nerve grafts from fetuses. Clin Anat 23:726–731. https://doi.org/10.1002/ca.21005
Watt T, Hariharan AR, Brzezinski DW, Caird MS, Zeller JL (2014) Branching patterns and localization of the common fibular (peroneal) nerve: an anatomical basis for planning safe surgical approaches. Surg Radiol Anat 36:821–828. https://doi.org/10.1007/s00276-013-1242-x
Yammine K, Assi C (2018) Neurovascular and tendon injuries due to ankle arthroscopy portals: a meta-analysis of interventional cadaveric studies. Surg Radiol Anat 40:489–497. https://doi.org/10.1007/s00276-018-2013-5
Acknowledgements
We thank the human cadaveric donors, who made this research possible.
Funding
No funding to declare.
Author information
Authors and Affiliations
Contributions
All the authors significantly contributed to the performance of this study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no competing interests.
Ethical approval
This study was approved by the Human Research Ethics Committee of the Federal University of Sergipe (no. 79260417.0.0000.5546).
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Correia, A.G.d., Vieira, J.G.S., Rodrigues, B.C.M. et al. Branching patterns of the superficial fibular nerve: an anatomical study with meta-analysis. Surg Radiol Anat 44, 1419–1425 (2022). https://doi.org/10.1007/s00276-022-03039-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-022-03039-x