Abstract
A persistent trigeminal artery is the most common persistent carotid-vertebrobasilar anastomosis, while persistent trigeminal artery variants involve termination at the cerebellar artery without connecting to the basilar artery. Internal carotid artery hyperplasia is also a rare congenital anomaly. To the best of our knowledge, there are no reports of persistent trigeminal artery variant associated with ipsilateral hypoplasia of the internal carotid artery. Herein, we report a case of a 44 year-old woman who visited a neurosurgical clinic because of chronic headaches. Magnetic resonance angiography showed impaired delineation of the left internal carotid artery, and she was referred to our hospital for catheter angiography. Angiogram revealed left internal carotid artery hypoplasia and a left persistent trigeminal artery variant that terminated at the left anterior inferior cerebellar artery. Computed tomography bone images showed a narrow left carotid canal. We diagnosed congenital hypoplasia of the left internal carotid artery concomitant with ipsilateral persistent trigeminal artery variant. Careful imaging assessment is important for identifying persistent trigeminal artery variant when associated with ipsilateral internal carotid artery hypoplasia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A persistent trigeminal artery (PTA) is a type of carotid-vertebrobasilar anastomosis [4]. PTA variants (PTAV) are rare and are characterized by termination at the cerebellar artery without connecting to the basilar artery. Hypoplasia of the internal carotid artery (ICA) is also a rare congenital anomaly. To the best of our knowledge, there are no reports of their simultaneous coexistence. Herein, we report a case of PTAV associated with ipsilateral hypoplasia of the ICA.
Case report
A 44 year-old woman with a history of congenital hearing loss and migraine without aura visited a neurosurgical clinic because of chronic headaches. She underwent magnetic resonance imaging and magnetic resonance angiography (MRA) at the clinic. MRA (1.5 T Magnetom Essenza, Siemens, Erlangen, Germany) showed impaired delineation of the left ICA, and she was referred to our hospital for catheter angiography (digital subtraction angiography [DSA]). MRA (3 T Magnetom Skyra, Siemens) performed at our institution also showed luminal narrowing of the left ICA. Additionally, an anomalous artery originating from the left ICA, which was not confirmed by 1.5 T MRA, was observed (Fig. 1a).
Magnetic resonance angiography showing hypoplasia of the left internal carotid artery and a persistent trigeminal artery variant (arrows). a Maximum intensity projection image. b Source image. The persistent trigeminal artery variant was tiny and its course could not be identified, even on the source image
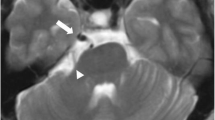
The anomalous artery was tiny and its course could not be identified, even on MRA source images (Fig. 1b). Left internal carotid angiogram revealed hypoplasia of the ICA and a PTAV terminating into the left anterior inferior cerebellar artery (AICA) (Fig. 2a). Right internal carotid angiogram demonstrated a fenestration at the A1 portion of the right anterior cerebral artery, and bilateral anterior cerebral artery blood flow. Vertebral angiogram showed adequate blood flow transiting from the left posterior communicating artery to the left middle cerebral artery (Fig. 2b). Computed tomography bone images showed that the left carotid canal was narrower than the right carotid canal (Fig. 3). Thus, we diagnosed her with congenital hypoplasia of the left ICA concomitant with ipsilateral PTAV.
Left internal carotid angiogram (a lateral view) revealed hypoplasia of the internal carotid artery and a persistent trigeminal artery variant terminating into the left anterior inferior cerebellar artery (arrow). Left vertebral angiogram (b lateral view) demonstrated adequate blood flow transiting from the left posterior communicating artery to the left middle cerebral artery, and no blood flow delineation of the left anterior inferior cerebellar artery
Discussion
Herein, we presented an extremely rare case of PTAV associated with ipsilateral ICA hypoplasia, which was found incidentally. To the best of our knowledge, there are no previous reports of PTAV associated with ipsilateral congenital hypoplasia of the ICA. Aplasia and hypoplasia of the ICA are rare congenital anomalies. ICA hypoplasia presents with a narrow caliber ICA. Bone images of the carotid canal can differentiate whether ICA hypoplasia is congenital (i.e., a narrower carotid canal diameter; as in the present case) or acquired (i.e., a normal carotid canal diameter). Congenital hypoplasia of the ICA is typically asymptomatic but may rarely present with cerebral ischemia [9].
PTA is the most common persistent carotid-vertebrobasilar anastomosis. Among PTA, PTAV is connected to the cerebellar artery without passing through the basilar artery, with a reported incidence of 0.18–0.76% [4]. PTAV includes those that terminate to the superior cerebellar artery, AICA (e.g., as in our case), and the posterior inferior cerebellar artery, with AICA termination being the most common [3, 8]. Although the exact embryogenesis mechanism for PTAV is not well understood, incomplete fusion of the paired longitudinal neural arteries may be involved [4]. PTAV is most often detected incidentally, as in the present case, although it can cause trigeminal neuralgia, PTA aneurysms (subarachnoid hemorrhage), and trigeminal cavernous fistulas [4, 5, 7, 10].
PTAV can usually be detected with MRA, with two previous studies demonstrating detection rates of 0.17 and 0.34% [6, 8]. However, in the present case, PTAV terminating at the AICA was confirmed by DSA rather than MRA. Thus, MRA may be unable to detect a PTAV with a small cerebellar artery size. Furthermore, an ipsilateral hypoplastic ICA (as in our case) has a reduced PTAV blood flow, which may also make PTAV identification by MRA difficult. Thus, DSA appears to be superior to MRA for identifying PTAV associated with ipsilateral ICA hypoplasia (Fig. 2).
A few cases of ICA hypoplasia with a PTA as a collateral pathway or ICA agenesis with PTAV have been reported [1, 2, 5]. However, to our knowledge, there are no reports of PTAV associated with ipsilateral congenital hypoplasia of the ICA. Although the simultaneous existence of both of these conditions is extremely rare, our findings provide important information for use in diagnostic and interventional neuroradiology in such cases.
Conclusion
Herein, we report an extremely rare case of PTAV associated with ipsilateral hypoplasia of the ICA. Careful imaging assessment is important for identifying PTAV when associated with ipsilateral ICA hypoplasia, because the PTAV is poorly visualized.
Data availability
Not applicable.
Code availability
Not applicable.
References
Kim D, Baek JW, Heo YJ, Jeong HW (2018) Congenital absence of the internal carotid artery with a persistent primitive trigeminal artery as a collateral pathway: a report of an anatomic variation. Surg Radiol Anat 40:811–813. https://doi.org/10.1007/s00276-018-2025-1
Lyu DP, Wang Y, Wang K, Yao M, Wu YF, Zhou ZH (2019) Acute cerebral infarction in a patient with persistent trigeminal artery and homolateral hypoplasia of internal carotid artery distal anastomosis: a case report and a mini review of the literature. J Stroke Cerebrovasc Dis 28:104388. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104388
Manabe H, Oda N, Ishii M, Ishii A (1991) The posterior inferior cerebellar artery originating from the internal carotid artery, associated with multiple aneurysms. Neuroradiology 33:513–515. https://doi.org/10.1007/BF00588043
Meckel S, Spittau B, McAuliffe W (2013) The persistent trigeminal artery: development, imaging anatomy, variants, and associated vascular pathologies. Neuroradiology 55:5–16. https://doi.org/10.1007/s00234-011-0995-3
Medhi G, Pendharkar H, terBrugge K, Prasad C, Gupta AK (2017) Trigeminal neuralgia caused by a new variant of persistent trigeminal artery associated with agenesis of internal carotid artery. Interv Neuroradiol 23:566–570. https://doi.org/10.1177/1591019917715955
O’uchi E, O’uchi T (2010) Persistent primitive trigeminal arteries (PTA) and its variant (PTAV): analysis of 103 cases detected in 16,415 cases of MRA over 3 years. Neuroradiology 52:1111–1119. https://doi.org/10.1007/s00234-010-0669-6
Shin YS, Kim SY, Kim BM, Park SI (2005) Ruptured aneurysm of the anomalous cerebellar artery originating from internal carotid artery presenting with carotid cavernous fistula: a case report. AJNR Am J Neuroradiol 26:1849–1851
Uchino A, Saito N, Okada Y, Kozawa E, Mizukoshi W, Inoue K, Takahashi M (2012) Persistent trigeminal artery and its variants on MR angiography. Surg Radiol Anat 34:271–276. https://doi.org/10.1007/s00276-011-0848-0
Uchino A, Ehara T, Kurita H (2019) Hypoplasia of the internal carotid artery with associated fenestration and extremely long P1 segment of the ipsilateral posterior cerebral artery diagnosed by MR angiography. Surg Radiol Anat 41:707–711. https://doi.org/10.1007/s00276-019-02212-z
Yang Z, Liu J, Zhao W, Xu Y, Hong B, Huang Q, He S (2010) A fusiform aneurysm of a persistent trigeminal artery variant: case report and literature review. Surg Radiol Anat 32:401–403. https://doi.org/10.1007/s00276-009-0537-4
Acknowledgements
We are grateful to Dr. Mitsuteru Oikawa (Hiragishi Brain and Nerve Clinic) for his support. We thank Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
W: data analysis, manuscript editing. E: project development, protocol development, data collection, data management, data analysis, manuscript writing, manuscript editing. N: data management, manuscript editing, supervision. Hideki Endo contributed to the study conception and design. Material preparation, data collection and analysis were performed by all authors. The first draft of the manuscript was written by Hideki Endo and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of Nakamura Memorial Hospital (No. 2022031801).
Consent to participate
Informed consent was obtained from the patient.
Consent for publication
The participant has consented to the submission of the case report to the journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Watanabe, D., Endo, H. & Nakamura, H. Persistent trigeminal artery variant associated with ipsilateral hypoplasia of the internal carotid artery. Surg Radiol Anat 44, 947–950 (2022). https://doi.org/10.1007/s00276-022-02964-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-022-02964-1