Abstract
Purpose
The main goal of the present study was to verify the presence, spatial location, the end of the canalis sinuosus (CS) trajectory and size of CS using cone beam computed tomography (CBCT) to characterise it as either a structure or an anatomical variation.
Methods
A trained examiner specialist in dental radiology and imagenology selected 200 CBCT images of the maxilla from 107 (53.5%) female and 93 (46.5%) male individuals aged between 18 and 85 years.
Results
A total of 133 (66.5%) patients had CS, being 61 (45.86%) unilateral and 72 (54.14%) bilateral. A higher frequency of CS was observed in males (P < 0.05) and no relationship was found between its presence and age. The end of the CS trajectory was more frequent in the regions of central incisor (n = 91; 44.39%), followed by lateral incisor (n = 45; 21.95%) and canine (n = 29; 14.15%). In our sample, the majority of these canals had a diameter of up to 1 mm (n = 198/205; 96.6%). No statistically significant relationship between diameter and the end of the CS trajectory, with location (i.e. bilateral or unilateral) was found. Gender and age had no influence on diameter, spatial location and the end of the CS trajectory (P > 0.05%).
Conclusion
As CS was frequently found in our sample, it can be considered an anatomical structure, and as such, it is fundamental that the dentist requests a CBCT examination before performing any invasive procedure in the maxillary region to preserve this important structure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The maxillary nerve is one of the branches of the trigeminal nerve, being exclusively sensitive and ramifying into superior posterior alveolar nerves, nasopalatine nerve, major palatine nerve and infra-orbital nerve. The infra-orbital nerve passes along the infra-orbital foramen and has a lateral branch called canalis sinuosus (CS), through which the anterior superior alveolar nerve passes. The CS is a neurovascular bundle that emerges from the posterior portion of the infra-orbital foramen and descends below the inferior wall of the orbit and medially towards the anterior wall of the maxillary sinus, bypassing the lateral and inferior limits of the nasal fossa, with the canal opening laterally to the nasal septum in front of the nasopalatine canal or in the anterior region of the maxilla. The insertion point is anterior to the incisive canal, and at this point, the CS commonly presents anatomical variations in the anterior palate, called accessory canals [4, 5, 12, 13]. Figure 1 shows the CS leaving the bilateral infra-orbital canals with some accessory canals at the end of their trajectory.
Bilateral canalis sinuosus leaving the bilateral infra-orbital canals, with some accessory canals at the end of their trajectory (by Machado et al. [9])
The neurovascular branches in the CS form the dental plexus in the canine region. CS enables sensibility of anterior teeth, nasal fossa floor and maxillary sinuses. The lack of knowledge of the positioning of CS can bring risks during dental surgical procedures and may cause pain, local infection and even paresthesia [12].
Some studies show that the presence of CS can mimic a periapical lesion and lead the dentist to perform inappropriate endodontic treatment [3], causes pain due to injuries to nerves during the placement of dental implants [4] or to have even paresthesia following a surgical procedure [1].
Cone beam computed tomography (CBCT) has been the most used examination to investigate and diagnose the presence of anatomical variations and structures, such as CS, because periapical and panoramic radiographs often cannot delineate and show this structure in detail [1, 2, 9, 10, 12]. In this way, CBCT is fundamental for diagnosing the presence of CS and the relationship between this structure and symptoms found [1, 9, 17].
The study of anatomical variations is important not only to collect anthropometric data but also to improve clinical protocols. CS has been little explored and many practitioners have no knowledge of its presence and location. In addition, the objective of the present study was to verify the presence, spatial location, the end of the CS trajectory and size of CS using CBCT to characterise it as either a structure or an anatomical variation.
Materials and methods
After approval by the Research Ethics Committee of the School of Dentistry of the City of São Paulo University (UNICID), 206 CBCT images of the maxilla of patients aged 18–85 years corresponding to the period from April to August 2018 were randomly selected from a clinical radiology (Itajai, Santa Catarina, Brazil) and prospectively evaluated.
All CBCT images were acquired with a scanner (Prexion® Corporation, Tokyo, Japan) operating with FOV of 8.1 × 7.5 cm, 90 KVp, 4.0 mA, focal distance of 0.15 mm and voxel size of 0.16 mm. All individuals submitted to CBCT examination whose field of vision (FOV) covered the maxillary sinuses entirely (i.e. from the upper border above the inferior ridge of the orbit to the lower border beneath the superior alveolar ridge, including dental arches in the posterior region of the maxilla) were included.
The tomographic examinations were interpreted by a trained examiner specialist in dental radiology and imagenology with more than 10 years of experience with CBCT. Images with patient motion, artefacts, bone lesions in the maxillary region and unsatisfactory quality or images suggesting surgery or trauma, presence of plates or screws, syndromes or malformations and bone graft material in the anterior maxilla were excluded.
The images were analysed by the examiner in the scanner’s workstation on a dynamic basis using the Prexion 3D viewer software. Axial, coronal and sagittal sections were analysed to verify presence or absence of CS and whether it was unilateral or bilateral, the end of the CS trajectory (i.e. regions of central and lateral incisors, nasopalatine canal, canine and first pre-molar) and measure the size of CS at the level of its mouth as viewed in the axial sections.
The resulting data were descriptively analysed and correlated using Fischer’s exact and Chi-square tests. GraphPad software (GraphPad Prism version 5.0 for Windows, GraphPad Software, San Diego, California USA) was used for statistical analyses at a significance level of 5% (P < 0.05).
Results
A total of 206 CBCT images were assessed, but six were discarded according to the exclusion criteria. Of these 200 images of the maxilla, 107 (53.5%) were from female and 93 (46.5%) from male individuals aged between 18 and 85 years, with median age of 53 years. CS was found in 133 (66.5%) patients, being more frequently observed in males (P < 0.05), as seen in Table 1. No relationship between the presence of CS and patient’s age was found (P > 0.05%), as seen in Table 2.
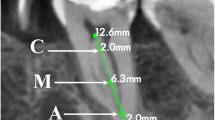
Of the 133 patients with CS, 72 (54.14%) had it bilaterally and 61 (45.86%) unilaterally. In Figs. 2 and 3, one can observe the presence of bilateral and unilateral CS, respectively. The end of the CS trajectory was more frequently found in the regions of central incisor (n = 91; 44.39%) (Fig. 2), followed by lateral incisor (n = 45; 21.95%) and canine (n = 29; 14.15%) (Fig. 3). Figure 4 shows the end of the CS trajectory of the 205 canals. No statistically significant relationship was found between the end of the CS trajectory and its location (i.e. bilateral or unilateral).
The diameter of CS was found to be homogeneous along its entire trajectory to the region of the mouth and whose size was measured, showing that the majority of CS had a diameter of up to 1 mm (n = 198/205; 96.6%) and only seven (3.4%) were greater than 1 mm. No statistically significant relationship was found between the diameter of CS and its location (i.e. bilateral or unilateral). Also, both gender and age had no influence on diameter, spatial location and mouth of the canal (P > 0.05%).
Discussion
The knowledge of structures and anatomical variations is crucial for invasive dental procedures to prevent complications and improve prognosis. Despite being little studied, there are some works showing complications resulting from the lack of anatomical knowledge of CS, mainly in dental implant surgeries involving the anterior maxillary region, such as pain and paresthesia [1, 11].
The function of CS is to assist in the sensitivity of anterior teeth, nasal fossa floor and maxillary sinus, according to their anatomical spatial location. Damage to any part of the CS trajectory will inevitably lead to problems in the affected region. Thus, it is very important to know its existence and location to prevent possible injuries to this structure.
CBCT is the best examination to determine the location of CS, thus being very useful for the diagnosis and evaluation of patients [3, 15]. Because periapical and panoramic radiographs cannot often delineate and show this structure in detail [10, 12, 17], we have chosen to evaluate CS using CBCT. The CBCT allows individualization and visualisation of the CS throughout its trajectory in three dimensions: axial, coronal and sagittal.
In our search for studies on CS, we have found 19 works on the PubMed database, where 11 were case reports, 6 were prospective studies and 2 were retrospective studies (Table 3). The prospective studies assessed the presence of CS using CBCT and the number of individuals ranged from 100 to 1000. The presence of CS was also very variable, ranging from 15.7% to 100%. Our study assessed 200 CBCT images, where 133 (66.5%) showed presence of CS. Some studies reporting a few findings considered only those cases of CS with diameter greater than 1 mm [13, 19].
We have found a higher frequency of CS in males in the present study, a finding also corroborated by Von Arx et al. [19] and Machado et al. [9]. On the other hand, no relationship between the presence of CS and patient’s age was found, as in the studies by Oliveira-Santos et al. [13] and Wanzeler et al. [20].
With regard to the location of CS, 72 (54.14%) patients had it bilaterally and 61 (45.86%) unilaterally, totalling 205 cases in our sample. However, several findings are reported in the literature: Oliveira-Santos et al. [13] found 6/28 bilateral (21.4%) and 22/28 unilateral cases, whereas Ghandourah et al. [3] and Guler et al. [4] reported 219 (100%) and 111 (100%) cases of bilateral CS, respectively.
The end of the CS trajectory was found in several sites, being more frequent in the regions of central incisor (n = 91; 44.39%), followed by lateral incisor (n = 45; 21.95%) and canine (n = 29; 14.15%). These findings are similar to those reported by Oliveira-Santos et al. [13], Von Arx et al. [19], Machado et al. [9] and Ghandourah et al. [3], who found higher frequencies of CS in the anterior region of the maxilla.
Only seven (3.4%) patients had CS with diameter greater than 1 mm. The majority of the studies in the literature describe cases of CS with diameter greater than or equal to 1 mm [4, 9], whereas only Ghandourah et al. [3] found results similar to ours, that is, 82.1% of the cases had a diameter less than or equal to 1 mm.
We have found no relationship between gender and diameter of CS, which was also corroborated by Von Arx et al. [19], although Machado et al [9] and Gurler et al. [4] showed greater diameters in male individuals.
Conclusion
The results from the present study have shown that CS is an anatomical structure as most (66.5%) of the study population had CS. In addition, it was observed that there was a higher frequency of CS in male individuals, but no relationship with age. Gender and age had no influence on diameter, location and the end of the CS trajectory either. Therefore, the use of CBCT to identify CS before invasive dental procedures in the region of anterior maxilla can prevent many complications and provide a better prognosis for the patient.
References
Arruda JA, Silva P, Silva L, Álvares P, Silva L, Zavanelli R, Rodrigues C, Gerbi M, Sobral AP, Silveira M (2017) Dental implant in the canalis sinuosus: a case report and review of the literature. Case Rep Dent 8:1–5
De Chacón VERG, Becerra JMM (2017) Canalis sinuosus: report de cuatro casos y revisión de la literatura. Rev Estomatol Herediana 27:39–43
Ghandourah AO, Rashad A, Heiland M, Hamzi BM, Friedrich RE (2017) Cone-beam tomographic analysis of canalis sinuosus accessory intraosseous canals in the maxilla. Ger Med Sci 15:1–12
Gurler G, Delilbasi C, Ogut EE, Aydin K, Sakul U (2017) Evaluation of the morphology of the canalis sinuosus using cone beam computed tomography in patients with maxillary impacted canines. Imaging Sci Dent 47:69–74
Jones FW (1939) The anterior superior alveolar nerve and vessels. J Anat 73:583–591
Kim JH, Abdala R Jr, Aoki EM, Baladi MG, Cortes ARG, Watanabe PCA, Arita ES (2015) Canalis sinuosus and radiographic procedures in the region of anterior maxilla. Clin Lab Res Dent 21:180–184
Kose EMRE, Sekerci AE, Soylu E, Nazlim S (2014) An extremely rare anatomical variation bilateral canalis sinuosus and nasopalatine duct cyst and role of TCCB in diagnosis. Int J Sci Res 23:361–363
Leven AJ, Sood B (2018) Pathosis or additional maxillary neurovascular channel? A case report. J Endod 44:1048–1051
Machado VC, Chrcanovic BR, Felippe MB, Manhães LRC Jr, Carvalho PSP (2016) Assessmet of accessory canals of the canalis sinuosus: a study of 1000 cone beam computed tomography examinations. Int J Oral Maxillofacc 45:1586–1591
Manhães LRC Jr, Villaça-Carvalho MF, Moraes ME, Lopes SL, Silva MB, Junqueira JL (2016) Location and classification of canalis sinuosus for cone beam computed tomography: avoiding misdiagnosis. Bras Oral Res 30:e49
McCrea SJJ (2017) Aberrations causing neurovascular damage in the anterior maxilla during dental implant placement. Case rep Dent 2017:5969643
Neves FS, Crusoé-Souza M, Franco LCS, Caria PHF, Bonfim-Almeida P, Crusoé-Rebello I (2012) Canalis sinuosus: a rare anatomical variation. Surg Radiol Anat 34:563–566
Oliveira-Santos C, Rubira-Bullen IRF, Monteiro SAC, León JE, Jacobs R (2013) Neurovascular anatomical variations in the anterior palate observed on CBCT images. Clin Oral Implants Res 24:1044–1048
Orhan K, Gorurgoz C, Akyol M, Ozarslanturk S, Avsever H (2018) An anatomical variant: evaluation of accessory canals of the canalis sinuosus using cone beam computed tomography. Folia Morphol 77:551–557
Rusu MC, Sãndulescu M, Bichir C, Muntianu LAS (2017) Combined anatomical variations: the mylohyoid bridge, retromolar canal and accessory palatine canals branched from the canalis sinuosus. Ann Anat 214:75–79
Shah PN, Arora AV, Kapoor SV (2017) Accessory branch of canalis sinuosus mimicking external root resorption: a diagnostic dilemma. J Conserv Dent 20:479–481
Shelley AM, Rushton VE, Horner K (1999) Canalis sinuosus mimicking a periapical inflammatory lesion. Br Dent J 186:378–379
Torres MGG, Valverde LF, Vidal MT, Crusoe-Rebello IM (2015) Branch of the canalis sinuosus: a rare anatomical variation—a case report. Surg Radiol Anat 37:879–881
Von Arx VT, Lozanoff S, Sendi P, Bornstein MM (2013) Assessment of bone channels other than the nasopalatine canal in the anterior maxilla using limited cone beam computed tomography. Surg Radiol Anat 35:783–790
Wanzeler AMV, Marinho CG, Alves SM Jr, Manzi F, Tuji FM (2015) Anatomical study of canalis sinuosus in 100 cone beam computed tomography examinations. Oral Maxillofacc Surg 19:49–53
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aoki, R., Massuda, M., Zenni, L.T.V. et al. Canalis sinuosus: anatomical variation or structure?. Surg Radiol Anat 42, 69–74 (2020). https://doi.org/10.1007/s00276-019-02352-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-019-02352-2