Abstract
Purpose
This study aims to: (a) quantify and evaluate normal relationships between neighboring spinal units using MR imaging indices, (b) propose an easy-to-apply-and-reproduce method of estimating the correct amount of distraction when surgically restoring a collapsed intervertebral disc, based on individualized measurements.
Methods
This is a retrospective cross-sectional MR imaging study of 119 adult subjects, aged 18–54, asymptomatic for low back pain. Each of the examinees should demonstrate two or more consecutive intervertebral discs classified as Pfirrmann grade I or II to be included. We measured and studied the relationships of disc height index, Dabbs index, Farfan index, disc convexity index and mean and posterior disc height per spinal level using multiple regression analysis. All measurements were tested for intra- and interobserver agreement by two raters.
Results
DHI, Dabbs, Farfan, and mean disc height had a statistically significant correlation with the spinal level and age. Our results were highly reproducible, with excellent inter- and intraobserver agreement and reliability between two raters (ICC = 0.992 and 0.994, respectively). Furthermore, we expressed each intervertebral space as a percentage of its adjacent space, introducing the coefficient α factor for every intervertebral space.
Conclusions
Our results suggest that a normal values’ database to refer during preoperative planning of correction of a degenerated intervertebral disc is feasible. Our study offers new anatomical and radiological insight in terms of spinal measurements and their potential correlation with current surgical techniques. A new approach for calculating disc space as an expression of its adjacent disc has been introduced with various potential applications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Degenerative alterations in spinal anatomy over time correlate with new-onset symptomatology that ranges from annoying to crippling. When conservative treatment no longer relieves pain, surgical therapeutic interventions have been developed that aim at restoring normal spinal relationships and function. Fusion is performed with structural constructs using mostly interbody cages in the disc space. Selecting an interbody cage with appropriate height is one of the key steps in lumbar interbody fusion, and has an important impact on clinical efficacy. An oversized cage leads to over distraction of intervertebral space and it might also increase possibility for injury to the nerve roots. Using a small fusion cage, on the other hand, will fail to restore the intervertebral height and lordosis, and may lead to severe complications such as cage migration and fusion failure, but the interbody cage height or perioperative distraction has long been determined by surgeons mostly based on their operational experience [30]. Another surgical option for patients with degenerative disc disease at a single level is total disc replacement (TDR), where intervertebral distraction is also part of the surgical technique. Postoperative complications due to insufficient anatomic corrections, such as adjacent segment disease (ASD) and flatback syndrome, can not only prolong patients’ agony, but also worry the treating surgeon. Perioperative over- or undercorrection of a degenerated spinal segment is an example of iatrogenic intervention that contributes to such complications [17].
The purpose of this study was to quantify normal anatomic intervertebral relationships in normal subjects by creating a database of magnetic resonance imaging (MRI) indices of the normal lumbar spinal unit. In addition, we propose that the correct amount of distraction required should be based on individualized measurements taking our results into account. Our approach could be useful for treatment planning when surgically restoring a collapsed intervertebral disc.
Materials and methods
Patient sample
We retrospectively reviewed lumbar MR imaging studies from a sample of 300 Greek patients, who had been investigated for spinal cord pathology for chronic neurological conditions and their lumbar MRI reported back as normal. We included asymptomatic patients for low back pain and/or sciatica, aged 18–54, with at least two consecutive normal spinal units (with Pfirrmann’s degeneration grade I or II) [22]. The exclusion criteria were: scoliosis, discs with Pfirrmann’s degeneration stage III or higher, any disc protrusion/herniation, Schmorl’s nodes, Modic changes, presence of congenital abnormalities, previous or recent vertebral fractures, tumors and previous spinal surgery. Our final sample consisted of 119 subjects, each with lumbar MR imaging examination showing two or more consecutive intervertebral discs Pfirrmann grade I or II, as rated by two researchers by consensus. A total of 528 discs from 119 subjects (4.44 per subject) were found to be eligible for inclusion. The 60 female and 59 male subjects had a mean age of 33.08 years with normal distribution of age (Shapiro–Wilk’s test) (Table 1).
Indices
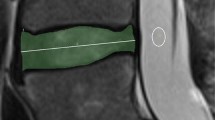
Our MR imaging metrics were: disc height index \(\left( {{\text{DHI}}=2 \times ~\frac{{a+b+c}}{{A+B+C+D+E+F}}} \right)\), Dabbs index \(\left( {=\frac{{a+c}}{2}} \right)\), Farfan index \(\left( {=\frac{{a+c}}{e}} \right)\), disc convexity index \(\left( {=\frac{{2b}}{{a+c}}} \right)\), mean disc height \(\left( {=\frac{{a+b+c}}{3}} \right)\)and posterior disc height (Fig. 1; Table 2). DHI helps minimize the inter-subject variations in overall size of the vertebral column, enabling inter-subject analyses [12]. Dabbs and Farfan indices were previously used for disc height measurements from radiographs, and previous data exist [4, 6, 21].
Midsagittal T2W MRI image of a lumbar spinal unit. A = anterior cephalad vertebral height, B = central cephalad vertebral height, C = posterior cephalad vertebral height, D = anterior caudal vertebral height, E = central caudal vertebral height, F = posterior caudal vertebral height, a = anterior disc height, b = central disc height, c = posterior disc height, d = disc diameter. Insertion positions on the corners of the vertebrae were defined as the lowest point for anterior and posterior corners
MR imaging protocol
All MR imaging examinations were performed at 1.5T scanner (PHILIPS, NL) and for the purposes of the present study, the sagittal T2W pulse sequence was used (TR-3000–4000 μs, TE-115 μs, slice thickness: 4 mm;/Gap-0.4, matrix-220 × 232 FOV-FH-275 mm). All measurements were performed in midsagittal T2W images on OsiriX suite software. All MR examinations took place during morning hours.
Statistical analysis
Multiple regression was performed to analyze the effect of sex, age and spinal segment on measurements on SPSS v21. Interobserver agreement for measurements was tested between two evaluators; an orthopedic spine surgeon/anatomist with a 10-year spine surgery experience and an orthopedic resident. Prior to the actual agreement study, each evaluator was provided with the original research by Pfirrmann and reviewed ten randomly selected cases independently, after which the cases were collectively reviewed and consensus reached on the measurement procedures [22]. Bias due to difference of equipment (e.g., different screen size and analysis) was eliminated using the same radiologist workstation. Each observer was blinded to the other observer’s measurements for the interobserver agreement analysis. In the intraobserver analysis, one observer was blinded to his own prior measurements and there was a 7-day interval between his first and second measurements. For the intraobserver agreement to be assessed, 406 length measurements were performed on 53(× 2) vertebral bodies and 50(× 2) intervertebral discs (ten subjects measured twice) by the same observer. To assess interobserver agreement, 360 length measurements were performed on 48(× 2) vertebral bodies and 43(× 2) intervertebral discs (ten subjects measured twice). Intraclass correlation coefficient (ICC) and Bland and Altman’s 95% limits of agreement (LOA) was used to determine both inter- and intraobserver agreement. All statistical analyses were performed on SPSS v21.
Results
The overall regression model was significant (p < 0.001) with R2 = 0.598 for DHI, R2 = 0.604 for Dabbs, R2 = 0.324 for Farfan, R2 = 0.198 for disc convexity index and R2 = 0.669 for mean disc height. Among the coefficients, the spinal level was statistically significant for all indices. To be more specific, DHI, Dabbs, Farfan, and mean disc height had a significant positive correlation with the spinal level. These metrics in L1–2, L2–3, L3–4 and L4–5 spinal levels were generally greater than in T12–L1 and increasing (p < 0.01) (Table 3; Fig. 2). As far as disc convexity index is concerned, there was a significant negative correlation with the spinal level. In particular, discs were less convex in the last two spinal levels L4–5 and L5–S1 (p < 0.01) compared to T12–L1. Age was also a significant coefficient for all calculated indices (p < 0.001). Gender did not appear to have any effect on disc height. We also expressed each intervertebral mean or posterior disc height as a fixed percentage of its caudal or cranial intervertebral height, the α factor, to create baseline values for future reference (Table 4).
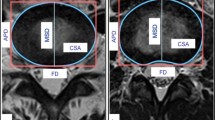
For intraobserver agreement, 95% LOA were calculated as 28.5% of mean values and ICC was 0.994 with 95% CI between 0.993 and 0.995. 95% LOA was calculated as 34% of mean values and ICC was measured 0.992 for interobserver agreement, with 95% CI between 0.990 and 0.994 (Table 5; Figs. 3, 4).
Discussion
In this study, we measured and expressed disc height using a variance of metrics. Dabbs method and Farfan index were initially chosen for comparison reasons, since they were previously calculated in an asymptomatic population, although comparison deemed in the end unnecessary since different methodology was used altogether. We integrated DHI in our calculations as a new means of expressing disc height by including the vertebral height in a manner that is easily reproduced and with previous results to compare. Baseline values for lumbar DHI and its correlation with degeneration have been previously measured [12]. We report slightly higher baseline values for DHI, probably due to a larger and different sample (Table 6). A database has been created of normal values for a variety of measurements and indices for all intervertebral spaces, except for L5–S1.
We decided to express each intervertebral space as a fixed percentage of its adjacent one, using either mean or posterior disc height. We named this fixed percentage α factor. Since we are considering our metrics as a database from a randomized population, we document our measurements for future reference and we believe that the α factor could be used as a means to restore normal intervertebral disc space height during perioperative distraction. For instance, if a degenerated L4–5 is operated on, by measuring the posterior or mean height of a healthy adjacent L3–4 and taking into account the α factor that we have already calculated on normal subjects, the desirable L4–5 spinal height can be estimated without over or undercorrecting. A sample equation is as follows: L3–4 = a3 × L4–5 ⟹ L4–5 = L3–4⁄⁄a3. Similar to our approach with an equation to express each intervertebral space, a stepwise regression equation was calculated by Wang et al. to select an interbody cage with appropriate height [30]. They used the fusion cage height as the dependent variable and two independent variables, the patient’s gender and the intervertebral height at the midpoint of the pathological segment.
Another way of interpreting our results is to consider the L4–5 space as the largest lumbar intervertebral disc space. Degenerative changes may occur on any spinal segment from very early on, with lumbar spine being the most prevalent one. The degenerative process begins from the second decade of life, followed by a period of stability until a second cycle of deterioration after the fourth decade [10]. A degenerated disc loses height with an annual rate of 3%, whereas a non-degenerated disc has a much slower annual rate of height reduction (0.6%) and bulging (1.7%) [11, 29]. Disc degeneration can be recognized on MR imaging approximately 4 years after an initial injury [16]. The previously mentioned 3% annual height loss suggests that the degeneration process may need 1–3 decades to run its full course, which is the potential of ASD progression as well. The disc height at the L4–5 level has been found to be affected the most after prolonged sitting [2]. Age and hours sitting were found to be significant risk factors for development of disc herniation at the L4–5 level [14]. The lumbar spinal unit most commonly affected by degeneration and most commonly operated on is L4–5 (men 69.1%, women 75.8%) [28]. The level most commonly affected by ASD is L3–4 (56%), followed by L4–5 (37%), L2–3 (6%), and T12–L1 or L1–2 (1%) [19]. The risk of disc prolapse is increased if the disc is not already degenerated due to the increased inherent hydrostatic pressure. The most insidious time for a disc prolapse is in the morning, when nucleus pulposus hydration state and pressure are highest, and the level most probable for this to occur is L4–5 [1, 31].
Disc height and its relationship with spinal level have been studied before. Pfirrmann et al. also showed that disc height shows a positive correlation with spinal level, similar to our results [21]. Our measurements were performed on a larger and younger patient sample, without radiological evidence of disc degeneration. They concluded that in the presence of degeneration, a decrease of disc height and volume, as well as a less convex disc shape, are to be expected. They also observed that when disc degeneration was not present, age tends to result in an inverse relationship on disc height, volume and shape. In another study, the reduction of lumbar disc height as a result of the aging process appears to be independent of whether the level has been operated on or not. Reductions in disc height at the fused levels L4–5 and L5–S1 were reported to be similar to reductions in disc height at non-fused levels, and to the identical levels in non-operated patients, after 9 years of follow-up [9]. As far as gender effect on disc space, Frobin et al. concluded that there is gender-related age dependence of disc space height, but it is explained by changes in vertebral shape and not disc height, with age [8].
As far as spinal biomechanics are concerned, a finite element model of an L3–4 motion segment has shown that disc height plays the most crucial part in motion segment stiffness compared to all other geometrical parameters of a spinal unit. Instability appears to increase as disc height increases and patient-specific ratio between disc height and vertebra height is even more important [20]. In addition, unstable spinal segments (due to disc height) transfer higher loads to the posterior spinal column, which leads to larger forces and strain exerted to the facet capsule and ligaments in flexion [5]. Therefore, the surgeon should consider properly restoring a narrowed disc space rather than overdistraction, to avoid instability of the index segment. In a prospective trial following TDR, patients with narrower disc preoperatively reported higher subjective patient satisfaction rates at the last follow-up in comparison to the group of patients with higher discs preoperatively [24].
Definition problems of ASD make its incidence difficult to calculate. Reports for revision surgery for ASD appear to be consistent though, ranging from 2 to 15% [17]. Numerous factors, either preexisting and/or surgical, have been blamed for ASD and their number is constantly increasing. There are inconsistent results and determination of the most important risk factors has not been established yet. The factors most reliably associated with ASD are laminectomy adjacent to a fusion and sagittal imbalance. Special attention is advised to avoid overdistraction and restore appropriate angular and translational alignment during arthrodesis [23]. Distraction during spinal fusion and maintenance of an abnormal intervertebral height (under- or overcorrection of a degenerated unit) seems to lead to more problems rather than relieve the patient from his symptoms. Due to the high influence of capsular ligaments on segmental stiffness, injury of the capsular ligaments of adjacent segments can highly increase instability in all motion directions. Iatrogenic overdistraction is a recognized risk factor of ASD, since it is the causative factor behind sagittal imbalance and altered facet tropism [20].
In another recent study, the effect of preoperative disc height and iatrogenic distraction during TDR on L5–S1 was investigated [27]. Greater than needed distraction does not increase the overall stability of the segment neither in flexion–extension, nor in axial rotation and lateral bending. Overdistraction can also result in high facet capsule and ligament forces during surgery leading to damaging of these structures, not only intraoperatively, but postoperatively as well. It also increases the extensile facet joint forces. These predicted high loads offer an explanation for clinical failure after TDR associated with iatrogenic overdistraction. Furthermore, Leivseth et al. showed that the amount of distraction is typically larger in L5–S1 than in L4–5, which might partially explain the unsatisfactory clinical results of a TDR in the lumbosacral segment L5–S1 [5, 18, 25, 26]. Another study tried to establish the relationship between overdistraction during posterior lumbar interbody fusion on L4–5 and the appearance of ASD at short-term follow-up (average 3.2 years) in 85 patients. It was shown that the distracted distance between the ASD groups (clinical and radiological) and the control group was statistically significant according to univariate and multivariate analyses [13].
Loss of lumbar lordosis is common in degenerative lumbar pathology secondary to disc space collapse and contributes to the development of flatback syndrome. Flatback syndrome is described as postural inclination of the trunk with loss of normal lumbar lordosis and most commonly reported cause is distraction instrumentation placement into the lower lumbar spine. Distraction-type posterior spinal instrumentation systems insufficiently restore anatomic sagittal alignment over the fused segments, due to inadequate surgical technique or preoperative planning as to the extent of iatrogenic distraction. Hypolordotic fused lumbar segments create pelvic inclination and lumbar lordosis mismatch and require distal unfused segment compensation to maintain sagittal balance. In the sagittally balanced flatback, patients can compensate with lumbosacral flexibility and reduction of thoracic kyphosis. As paraspinal musculature fatigues and discs degenerate, maintaining sagittal balance requires increasing pelvic retroversion and hip extension. Ultimately, disc degeneration at adjacent levels continues and overcomes compensatory mechanisms, resulting in sagittal imbalance and worsening symptoms. The importance of sagittal alignment after fusion dictates the need for spinal surgeons to optimize preoperative planning. Disc height restoration can increase lumbar lordosis through differential distraction of the anterior column and can also indirectly decompress the neural foramen. Intervertebral height and lumbar lordosis reconstruction are important for achieving good surgical results [3, 15].
Interpretation of ICC values was performed as proposed by Fleiss, with ICC values < 0.4 considered poor agreement; 0.40–0.74 fair to good agreement, and > 0.75 excellent agreement beyond chance [7]. Therefore, we consider interobserver and intraobserver agreement as excellent. Intraobserver agreement of measurements was slightly better than interobserver agreement. There was also no presence of bias judging by the mean difference of measurements, and range of measurements was acceptable for all intra- and interobserver measurements. This is an easy-to-apply-and-reproduce method for any radiologist or spinal surgeon with Dicom viewer software.
The major strength of this study is the introduction of a new spinal coefficient (α factor) with epidemiological and surgical applications, based on measurements on a sizeable sample. Our metrics can be used as baseline values. We have proven that α factor can be reproduced widely with a high reproducibility, as no specific equipment is required. The major limitations of this study are its retrospective nature, lack of biometric documentation such as weight and height of our subjects, which might have allowed for further deductions.
Conclusion
Our study is the first effort towards creating a database for a more systemic approach to epidemiological data concerning intervertebral disc height. We measured disc height in an asymptomatic low back pain population with normal age distribution and created baseline values. A new approach for calculating disc space as an expression of its adjacent segment has been introduced. When restoring a collapsed degenerated spinal segment, instead of randomly under- or overcorrecting disc space, these baseline values could help calculate the correct amount of distraction required, based on individualized normal relationships between neighboring intervertebral discs. Understanding normal lumbar disc morphometry is important when interpreting the pathological changes associated with disc degeneration.
References
Adams MA, Dolan P (2012) Intervertebral disc degeneration: evidence for two distinct phenotypes. J Anat 221:497–506
Billy GG, Lemieux SK, Chow MX (2014) Changes in lumbar disk morphology associated with prolonged sitting assessed by magnetic resonance imaging. PM R 6:790–795. https://doi.org/10.1016/j.pmrj.2014.02.014
Boody BS, Rosenthal BD, Jenkins TJ, Patel AA, Savage JW, Hsu WK (2017) Iatrogenic flatback and flatback syndrome: evaluation, management, and prevention. Clin Spine Surg 30(4):142–149. https://doi.org/10.1097/BSD.0000000000000522
Dabbs VM, Dabbs LG (1990) Correlation between disc height narrowing and low-back pain. Spine (Phila Pa 1976) 15:1366–1369
Dreischarf M, Schmidt H, Putzier M, Zander T (2015) Biomechanics of the L5–S1 motion segment after total disc replacement—influence of iatrogenic distraction, implant positioning and preoperative disc height on the range of motion and loading of facet joints. J Biomech 48:3283–3291. https://doi.org/10.1016/j.jbiomech.2015.06.023
Farfan HF, Cossette JW, Robertson GH, Wells RV, Kraus H (1970) The effects of torsion on the lumbar intervertebral joints: the role of torsion in the production of disc degeneration. J Bone Joint Surg Am 52:468–497
Fleiss J (1986) The design and analysis of clinical experiments. Wiley, New York
Frobin W, Brinckmann P, Biggemann M, Tillotson M, Burton K (1997) Precision measurement of disc height, vertebral height and sagittal plane displacement from lateral radiographic views of the lumbar spine. Clin Biomech (Bristol Avon) 12(Suppl 1):S1–S63
Froholdt A, Brox JI, Reikerås O, Leivseth G (2013) Disc height and sagittal alignment in operated and non-operated levels in the lumbar spine at long-term follow-up: a case-control study. Open Orthop J 7:258–263
Haefeli M, Kalberer F, Saegesser D, Nerlich AG, Boos N, Paesold G (2006) The course of macroscopic degeneration in the human lumbar intervertebral disc. Spine (Phila Pa 1976) 31:1522–1531
Hassett G, Hart DJ, Manek NJ, Doyle DV, Spector TD (2003) Risk factors for progression of lumbar spine disc degeneration: the Chingford Study. Arthritis Rheum 48:3112–3117
Jarman JP, Arpinar VE, Baruah D, Klein AP, Maiman DJ, Tugan Muftuler L (2015) Intervertebral disc height loss demonstrates the threshold of major pathological changes during degeneration. Eur Spine J 24:1944–1950
Kaito T, Hosono N, Mukai Y, Makino T, Fuji T, Yonenobu K (2010) Induction of early degeneration of the adjacent segment after posterior lumbar interbody fusion by excessive distraction of lumbar disc space. J Neurosurg Spine 12:671–679
Kanayama M, Togawa D, Takahashi C, Terai T, Hashimoto T (2009) Cross-sectional magnetic resonance imaging study of lumbar disc degeneration in 200 healthy individuals. J Neurosurg Spine 11:501–507. https://doi.org/10.3171/2009.5.SPINE08675
Kepler CK, Rihn JA, Radcliff KE, Patel AA, Anderson DG, Vaccaro AR, Hilibrand AS, Albert TJ (2012) Restoration of lordosis and disk height after single-level transforaminal lumbar interbody fusion. Orthop Surg 4(1):15–20. https://doi.org/10.1111/j.1757-7861.2011.00165.x
Kerttula LI, Serlo WS, Tervonen OA, Pääkkö EL, Vanharanta HV (2000) Post-traumatic findings of the spine after earlier vertebral fracture in young patients: clinical and MRI study. Spine (Phila Pa 1976) 25:1104–1108
Lee JC, Choi SW (2015) Adjacent segment pathology after lumbar spinal fusion. Asian Spine J 9:807–817
Leivseth G, Braaten S, Frobin W, Brinckmann P (2006) Mobility of lumbar segments instrumented with a ProDisc II prosthesis: a two-year follow-up study. Spine (Phila Pa 1976) 31:1726–1733
Mannion AF, Leivseth G, Brox JI, Fritzell P, Hägg O, Fairbank JC (2014) ISSLS Prize winner: Long-term follow-up suggests spinal fusion is associated with increased adjacent segment disc degeneration but without influence on clinical outcome: results of a combined follow-up from 4 randomized controlled trials. Spine (Phila Pa 1976) 39:1373–1383
Meijer GJ, Homminga J, Veldhuizen AG, Verkerke GJ (2011) Influence of interpersonal geometrical variation on spinal motion segment stiffness: implications for patient-specific modeling. Spine (Phila Pa 1976) 36:E929–E935. https://doi.org/10.1097/BRS.0b013e3181fd7f7f
Pfirrmann CW, Metzdorf A, Elfering A, Hodler J, Boos N (2006) Effect of aging and degeneration on disc volume and shape: a quantitative study in asymptomatic volunteers. J Orthop Res 24:1086–1094
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26:1873–1878
Radcliff KE, Kepler CK, Jakoi A, Sidhu GS, Rihn J, Vaccaro AR, Albert TJ, Hilibrand AS (2013) Adjacent segment disease in the lumbar spine following different treatment interventions. Spine J 13:1339–1349
Siepe CJ, Hitzl W, Meschede P, Sharma AK, Khattab MF, Mayer MH (2009) Interdependence between disc space height, range of motion and clinical outcome in total lumbar disc replacement. Spine (Phila Pa 1976) 34:904–916
Siepe CJ, Korge A, Grochulla F, Mehren C, Mayer HM (2008) Analysis of post-operative pain patterns following total lumbar disc replacement: results from fluoroscopically guided spine infiltrations. Eur Spine J 17:44–56
Siepe CJ, Mayer HM, Heinz-Leisenheimer M, Korge A (2007) Total lumbar disc replacement: different results for different levels. Spine (Phila Pa 1976) 32:782–790
Strube P, Hoff EK, Schürings M, Schmidt H, Dreischarf M, Rohlmann A, Putzier M (2013) Parameters influencing the outcome after total disc replacement at the lumbosacral junction. Part 2: distraction and posterior translation lead to clinical failure after a mean follow-up of 5 years. Eur Spine J 22:2279–2287
Teraguchi M, Yoshimura N, Hashizume H, Muraki S, Yamada H, Minamide A, Oka H, Ishimoto Y, Nagata K, Kagotani R, Takiguchi N, Akune T, Kawaguchi H, Nakamura K, Yoshida M (2014) Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: the Wakayama Spine Study. Osteoarthr Cartil 22:104–110. https://doi.org/10.1016/j.joca.2013.10.019
Videman T, Battié MC, Parent E, Gibbons LE, Vainio P, Kaprio J (2008) Progression and determinants of quantitative magnetic resonance imaging measures of lumbar disc degeneration: a five-year follow-up of adult male monozygotic twins. Spine (Phila Pa 1976) 33:1484–1490
Wang H, Chen W, Jiang J, Lu F, Ma X, Xia X (2016) Analysis of the correlative factors in the selection of interbody fusion cage height in transforaminal lumbar interbody fusion. BMC Musculoskelet Disord 17:9
Zhong W, Driscoll SJ, Wu M, Wang S, Liu Z, Cha TD, Wood KB, Li G (2014) In vivo morphological features of human lumbar discs. Medicine (Baltimore) 93:e333. https://doi.org/10.1097/MD.0000000000000333
Author information
Authors and Affiliations
Contributions
AHF: Data analysis, manuscript writing. DLA: Project development, manuscript writing. AHK: Manuscript editing. SEV: Manuscript writing and editing. MH: Data collection and manuscript editing. AHZ: Project development, data collection, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Fyllos, A.H., Arvanitis, D.L., Karantanas, A.H. et al. Magnetic resonance morphometry of the adult normal lumbar intervertebral space. Surg Radiol Anat 40, 1055–1061 (2018). https://doi.org/10.1007/s00276-018-2048-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-018-2048-7