Abstract
Objective
The present study was undertaken to know the anatomical basis of medial sural artery (MSA) and its perforators in Nepalese.
Methods
The popliteal arteries of 16 preserved cadaveric lower limbs were injected with a mixture of red ink and glycerine. The number, location, diameter of perforators; length and intramuscular course of pedicle; the branching pattern of MSA were observed and measured.
Results
The mean of 2.2 ± 1.2 perforators (range 0–4) was observed. The perforators were clustered between 8.6 and 25.7 cm from the popliteal crease and 0.3–7.5 cm from posterior midline of leg. The dominant perforators were observed in middle 1/3rd of the leg. The average pedicle length was 12.04 ± 3.27 cm. The intramuscular courses of pedicles were observed in deep and superficial strata in 65.7 and 34.3%, respectively. The MSA originated from popliteal artery in 62.5% and common sural artery in 37.5%. An accessory MSA was found in 12.5%. Type I and Type III branching patterns of MSA were observed in 31.2% each whereas Type II was found in 37.5%. The mean external diameter of perforators and MSA were 0.85 ± 0.27 mm and 2.2 ± 0.43 mm, respectively.
Conclusions
The metrical presentation of this study provides an easy access to know about the distribution of perforators and branching pattern of MSA which will help the surgeons to make a convenient plan to harvest the MSA perforator flap in Nepalese population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perforator-based skin flaps, nourished by musculocutaneous perforating vessels are becoming popular in recent decades [5]. The vascular anatomy of posterior calf region is based on superficial sural artery and musculocutaneous perforators from medial and lateral sural arteries [2]. The medial and lateral sural arteries are large branches of the popliteal artery and arise at variable levels, usually at the level of the tibiofemoral joint line [16]. The sural arteries may arise from a common trunk from popliteal artery as common sural artery (CSA) [11]. Each sural artery supplying the corresponding head of gastrocnemius muscle gives number of musculocutaneous perforators to supply the skin of the posterior calf. Due to the presence of musculocutaneous perforators, the skin with certain muscles can be transferred reliably as a perforator flap [13].
The conceptual idea of perforator flaps were first postulated in the 1960s [4] and subsequently in the late 1980s, Kroll and Rosenfield L. made the beginning of perforator flaps [10]. Then in 2001, Cavadas et al. [2] described the anatomical basis of the perforators from the medial and lateral sural arteries and also introduced the medial sural artery perforator flap. Subsequently, further anatomical studies on medial sural artery (MSA) perforators have been performed by others [6, 8, 17].
The MSA perforator flap is a thin flap with a long and reliable vascular pedicle. It is a good alternative for the reconstruction of soft tissue defects in distal extremities [2, 6, 8] and the head and neck region [7]. This flap can be elevated without the need of gastrocnemius muscle sacrifice, thus causing minimum donor-site morbidity [6, 18]. Dusseldrop JR et al. with their radiological study have identified three different types of branching patterns of the intramuscular course of MSA [3]. Type I consists a single branch, Type II exhibits two branches and Type III reveals three or more branches of MSA. The knowledge about these branching patterns is important for the surgeons to plan for the pedicle reconstruction of the lower limb [3].
Various anatomical studies conducted by several authors exposed different anatomical distribution of MSA perforators [2, 6, 8, 17]. However, the studies regarding its branching pattern are limited. Hence, to gain better understanding of vascular anatomy of medial posterior calf region, an anatomical study of MSA and its perforators on the Nepalese population was performed. It is primarily aimed for the surgeons, to aid in their preoperative plan of the MSA perforator flaps in a composite population of Nepal.
Materials and methods
The study was conducted at Department of Anatomy, Nepal Medical College from January 2016 to March 2017. It involved 16 lower extremities of 8 adults’ preserved cadavers (6 males and 2 females), approximately 30–55 years of age. For cadaver preservation, the arterial embalming technique was used, which involves injecting the preservative fluid through cannula in common carotid artery via gravity method. Prior to dissection, length of the individual leg was measured from medial epicondyle of the femur to medial malleolus. Then, the popliteal artery was exposed at the popliteal fossa and injected with a red dye, a special mixture of red ink 40 ml and glycerine 10 ml, using a 50-ml syringe with 16 gauge needle, fitted with a catheter. After 48 h, the leg dissection was performed to explore the perforators. The skin was retracted medially from posterior midline of leg. The total number of MSA perforators including both dominant and non-dominant was recorded. The perforators with external diameter > 0.5 mm were taken as dominant perforators in accordance with other authors [3, 6, 9]. Those perforators arising from arteries other than MSA were excluded.
The following parameters were recorded:
-
1.
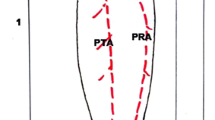
Number of perforators The numbers of perforators piercing the medial head of gastrocnemius muscle were identified (Fig. 1) and their exit points in the fascia were marked on the skin surface with pushpins.
-
2.
Distance of perforators from popliteal crease (PC) and posterior midline (PML) were measured with the help of measuring tape. The distance of each perforator from PC was correlated with the length of leg to find out exact location of perforators in leg.
-
3.
Length and intramuscular course of pedicle The intramuscular dissection of the identified perforators was performed through the medial head of gastrocnemius muscle and was continued proximally till MSA. The intramuscular course of pedicle was observed and its length was measured from the main trunk of MSA to the origin of perforators [7, 17].
-
4.
Origin of MSA The level of origin of each MSA was observed with respect to PC [17].
-
5.
Branching pattern of MSA The number of branches arising from MSA were recorded and classified into different types.
-
6.
External diameter of perforators and MSA Their external diameters at their origin were measured with a help of digital vernier caliper.
Results
Number of perforators
The MSA perforators were traced in all 16 legs. A total of 35 musculocutaneous perforators were identified in 15 (94%) legs while a right leg of a male cadaver (6.2%) revealed an absence of MSA perforator. Amongst those 15 legs with MSA perforators, one musculocutaneous perforator was observed in 4 legs, two perforators in 5, three perforators in 3 and four perforators in remaining 3 legs (Table 1). Out of 35 perforators, 18 (51.4%) perforators were identified in right legs and 17 (48.6%) perforators in left. In overall, the average number of perforators including both dominant and non-dominant was 2.2 ± 1.2 (range 0–4). However, considering only the dominant perforators, the total of 31 dominant perforators (diameter > 0.5 mm) was observed with an average of 1.94 ± 1.1.
Distance of perforators from PC and PML of leg
All 35 perforators were distributed in a distance between 8.6 and 25.7 cm (mean 15.1 ± 3.6 cm) from PC. Among them, 29 perforators (83%) were observed within a distance of 10.5–18.5 cm from PC (Fig. 2). In context to PML of leg, all the perforators were distributed within the distance of 0.3–7.5 cm with a mean of 3.15 ± 1.8 cm (Fig. 2).
The length of the leg was ranged from 36.5 to 41.5 cm (mean 39.6 ± 1.43 cm). The location of MSA perforators was observed in relation to the length of the legs. Amongst 31 dominant perforators, 22 perforators (70.97%) were distributed in the middle 1/3rd and the rest 9 perforators (29.03%) in the upper 1/3rd of the leg (Table 2). The locations of dominant perforators were observed in the middle 1/3rd of the leg irrespective of their length of the leg (Table 2).
Length and intramuscular course of pedicle
The average pedicle length was found as 12.04 ± 3.27 cm (range 5.7–20.3 cm). During the intramuscular dissection, two different patterns of intramuscular course of pedicles were observed. The pedicles of 23 perforators (65.7%) had a deep intramuscular course within the medial head of gastrocnemius, thus rendering dissection more difficult. The remaining pedicles of 12 perforators (34.3%) ran superficially within the muscle (superficial intramuscular course) leading to minimum muscular damage and easier dissection.
Origin of MSA
In 62.5% (10 legs), MSA was observed to originate directly from popliteal artery (Fig. 3), while in the rest of the 37.5% (6 legs) MSA originated from CSA (Fig. 4). The MSA emerged distal to PC in 50% of legs, at the level of PC in 25% and proximal to the PC in the rest 25% of the cases. An accessory MSA was found in each of the right lower limbs of two male cadavers. In both cases, the accessory MSA originated from popliteal artery distal to PC (Fig. 5) whereas main MSA originated from CSA (Fig. 5).
Left leg showing Type III intramuscular branching pattern of MSA with its musculocutaneous perforators (asterisk) arising from its medial and intermediate branch. LHG lateral head of gastrocnemius muscle, MHG medial head of gastrocnemius muscle, MSA medial sural artery, PA popliteal artery, SSA superficial sural artery
Left leg showing Type II intramuscular branching pattern of MSA with a single musculocutaneous perforator (asterisk) arising from its medial branch. CSA common sural artery, LHG lateral head of gastrocnemius muscle, LSA lateral sural artery, MHG medial head of gastrocnemius muscle, MSA medial sural artery, PA popliteal artery, SSA superficial sural artery
Right leg showing the presence of an accessory MSA arising from popliteal artery and its musculocutaneous perforator (diamond). Note the Type I intramuscular branching pattern of an accessory MSA and perforators (asterisk) from main MSA. CSA common sural artery, LHG lateral head of gastrocnemius muscle, LSA lateral sural artery, MHG medial head of gastrocnemius muscle, MSA medial sural artery, PA popliteal artery, SSA superficial sural artery
Branching pattern of MSA
Three different types of branching patterns of intramuscular course of MSA were observed. Type I and Type III (Fig. 3) were observed in 5 (31.2%) legs each whereas Type II (Fig. 4) was found in 6 (37.5%) legs. Type I branching pattern of accessory MSA was observed in two right legs (Fig. 5).
External diameter of perforators and MSA
The average external diameter of perforators was 0.85 ± 0.27 mm (range 0.30–1.34 mm). The external diameters of 14 perforators were found to be greater than 1 mm whereas 4 perforators’ diameters were less than 0.5 mm. The diameters of remaining 17 perforators were ranged between 0.5 and 1 mm. The mean external diameter of perforator ≥ 1 mm was 1.12 ± 0.10 mm (range 1–1.34 mm). The external diameter of MSA near its origin was found to be ranged from 1.5 to 3.2 mm (mean 2. 2 ± 0.43 mm). The mean external diameter of the accessory MSA was 2.1 ± 0.2 mm.
Discussion
There are several advantages of using musculocutaneous perforator flaps over classic gastrocnemius myocutaneous flaps, such as reduced donor-site morbidity, less functional loss and increased flap mobility and shaping [2, 5, 6, 9].
Number of perforators
In the present study, the average number of MSA perforator was 2.2 (range 0–4). This finding is in concurrence with the average mentioned by various authors [1, 2, 7, 8, 12, 17] (Table 3). Wong et al. [19], however, have reported an average of 4.4 perforators (range 3–8) out of 10 cadaveric lower limbs, which conflicts with our observation and is higher. In the study conducted by Dusseldrop et al. [3], the average number of dominant perforators (> 0.5 mm) was 2 (range 0–6), which is consistent with our finding (mean 1.9; range 0–4), but there exists conflicts in case of the number of perforators observed per leg, in that they observed more numbers than we did.
Our study revealed an absence of MSA perforator in a single right leg. This discrepancy may have resulted due to the differing diameter selection criteria for choosing the perforators as dominant one. In some of the studies, perforators with small diameter (< 0.5 mm or < 1 mm) were ignored [3, 15]. In the study conducted by Dusseldrop et al. [3], they found an absence of dominant MSA perforators (diameter > 0.5 mm) in 1 (7%) out of 14 lower limbs. In contrast, Shimizu et al. [15], however, studied only those perforators wider than 1 mm as dominant one and reported the absence in 1 (8.3%) out of 12 lower limbs.
Distance of perforators from the PC and PML of leg
In our study, MSA perforators were observed at a distance of 8.6 to 25.7 cm (mean 15.1 ± 3.6 cm) from PC. This is concurrent with the observations made by other authors [2, 7, 8, 19] (Table 3). We also observed a cluster of MSA perforators within 10.5–18.5 cm from PC, which is similar to Cavadas et al. [2] where the clusters were reported within 9–18 cm. The location of perforators is variable and depends on the underlying branching pattern [3], length of leg and gastrocnemius muscle belly [12].
The perforators in our study were observed at 0.3–7.5 cm (mean 3.15 ± 1.8 cm) from PML, which concurs with the finding of Kao et al. [7] (0.5–7 cm, mean 3.6 ± 1.3 cm). However, the studies conducted by Cavadas et al. [2] and Okamoto et al. [12] have found a narrow range of 1–6 cm (mean 2.5 cm) and 0.5–4.5 cm, respectively (Table 3).
Length and intramuscular course of pedicle
The average pedicle length of our study was 12.04 cm, which is consistent with the observation of other studies [7, 17] (Table 3). Our study established the shortest pedicle length of 5.7 cm and the longest pedicle length of 20.3 cm. The shortest pedicle length is in agreement with Kim et al. [8], while on the contrary, the longest pedicle length is in agreement with Okamoto et al. [12] and Altaf [1]. Kao et al. [7] in their clinical study had stated that the pedicle length of even 16 cm is adequate to reach the recipient vessels in the neck region during MSA perforator flap transfer. The pedicle length are reported to depend on the locations of the selected and dominant perforators [1]. This may be the reason behind reporting different pedicle length by various authors. Generally, the skin flaps with long pedicles have a greater arc of rotation for free flaps [1, 6, 19] and have a great advantage to cover wide soft tissues defect.
As for the intramuscular course of pedicle, in our study we observed deep and superficial course of pedicle in 65.7 and 34.3% cases, respectively, which is in close resemblance with Thione et al. [17] who observed in 70 and 30% cases, respectively. However, in stark contrast to our finding, Hallock only observed superficial intramuscular course of pedicles in all the legs [6].
Origin of MSA
According to present study, MSA originated from the popliteal artery in 62.5% and CSA in 37.5% of the legs. Similar study was conducted by Altaf [1] where he observed origin of MSA from popliteal artery in 70% and CSA in 30%. In contrast to the study conducted by Altaf [1] our study revealed more number of MSA originated from CSA, i.e. 37.5% vs 30%. Our study revealed an accessory MSA in 12.5% of the legs. This is similar to the observation reported by Potparic et al. [14] in 15% but slightly lower than the finding observed by Hallock [6] in 20%.
The MSA emerged distal to PC in most of the legs (50%) of our study: at the level of PC in 25% and proximal to PC in the remaining 25% of the legs. However, Thione et al. observed level of origin of MSA at PC in 70% and proximal to PC in the remaining 30% [17].
Branching pattern of MSA
This study revealed the most common branching pattern as Type II, which is concurrent with other authors [3, 19]. However, the percentage frequency of Type II (37.5%) is significantly lower than the findings of Wong et al. [19] and Dusseldrop et al. [3] who observed it in 80 and 59%, respectively. Our study observed Type I branching pattern of MSA in 31.2% which is similar to Dusseldrop et al.’s study [3] but higher than Wong et al.’s [19] who observed in 10%. Similar to Type I, Type III branching pattern of MSA was also found in 31.2% which is higher than the findings observed by other authors [3, 19] who observed it in 10%. Previous studies [3, 19] described Type III as least common branching pattern, which is inconsistent with our observation. These significant variations may possibly be the result of sample size or ethnicity differences between Nepalese, Singaporean [19] and Australian [3] population. Further studies with more sample size are needed to account for population bias. Also the large variation might be because of ethnicity factor which also requires further detailed study.
Diameter of perforators and MSA
The average external diameter of perforators was 0.85 ± 0.27 mm. Other studies have observed the average external diameter as 0.5 mm [17], 0.7 mm [1] and 0.8 mm [12]. It shows that the mean diameter of 0.85 mm of this study is almost equal to the findings of Altaf et al. [1] and Okamoto et al. [12] (Table 3). The mean external diameter of perforator ≥ 1 mm was 1.12 mm (range 1–1.34 mm). In contrast to this, Wong et al. [19] observed a slightly larger mean diameter of 1.5 mm with wider range of 1–2 mm (Table 3).
The mean external diameter of MSA was observed as 2.2 ± 0.43 mm (range 1.5–3.2 mm) which is in agreement with Thione et al. [17]. However, in disagreement with our observation, some of the other studies have reported the mean diameter as 3 mm [1, 18] and 2.5 mm [3, 12]. The MSA diameter of 2 mm is widely accepted to be suitable for easy microanastomosis with recipient vessels by many studies [1, 12, 17]. Since the study was conducted on embalmed cadavers, the diameter presented in our study may be narrower than that of living condition. Hence, anatomical study in fresh cadaver before embalming may yield a better insight.
Conclusion
The presence of at least one single dominant MSA perforator in the lower extremities corroborates the reliability of MSA flap. The metrical presentation of MSA perforators in the present study provides a reliable knowledge about the differing distribution of perforators and branching pattern of MSA. Based on this information, the surgeons can choose the leg with most suitable intramuscular branching pattern of MSA and can modify the surgical approach to efficiently harvest the MSA perforator flap.
References
Altaf FM (2011) The anatomical basis of the medial sural artery perforator flaps. West Indian Med J 60:622–627
Cavadas PC, Sanz-Gimenez-Rico JR, Camara AG, Navarro-Monzonis A, Soler-Nomdedeu S, Martinez-Soriano F (2001) The medial sural artery perforator free flap. Plast Reconstr Surg 108:1609–1615
Dusseldrop JR, Pham QJ, Ngo Q, Gianoutsos M, Moradi P (2014) Vascular anatomy of the medial sural artery perforator flap: a new classification system of intra-muscular branching patterns. J Plast Reconstr Aesthet Surg 67:1267–1275
Fujino T (1967) Contribution of axial and perforator vasculature to circulation in flaps. Plast Reconstr Surg 39:125–137
Geddes CR, Morris SF, Neligan PC (2003) Perforator flaps: evolution, classification, and applications. Ann Plast Surg 50:90–99
Hallock GG (2001) Anatomic basis of the gastrocnemius perforator-based flap. Ann of Plast Surg 47:517–522
Kao HK, Chang KP, Chen YA, Wei FC, Cheng MH (2010) Anatomical basis and versatile application of the free medial sural artery perforator flap for head and neck reconstruction. Plast Reconstr Surg 125:1135–1145
Kim HH, Joeng JH, Seul JH, Cho BC (2006) New design and identification of the medial sural perforator flap: an anatomical study and its clinical applications. Plast Reconstr Surg 117:1609–1618
Kosutic D, Pejkovic B, Anderhuber F, Vadnjal-Donlagic S, Zic R, Gulic R (2012) Complete mapping of lateral and medial sural artery perforators: anatomical study with Duplex-Doppler ultrasound correlation. J Plast Reconstr Aesthet Surg 65:1530–1536
Kroll SS, Rosenfield L (1988) Perforator-based flaps for low posterior midline defects. Plast Reconstr Surg 81:561
McMinn RMH (1994) Lower limb. Lastʼs anatomy: regional and applied. Churchill Livingstone, New York, pp 173–175
Okamoto H, Sekiya I, Mizutani J, Otsuka T (2007) Anatomical basis of the medial sural artery perforator flap in Asians. Scand J Plast Reconstr Surg Hand Surg 41:125–129
Otani M, Okamoto H, Kagami H, Narita Y, Ebisawa K, Oda T (2012) Anatomical study on perforators of the medial and lateral sural artery in Asains. Nagoya Med J 52:89–98
Potparic Z, Colen LB, Sucur D, Carwell GR, Carraway JH (1995) The gastrocnemius muscle as a free-flap donor site. Plast Reconstr Surg 95:1245–1252
Shimizu F, Kato A, Sato H, Taneda H (2009) Sural perforator flap: assessment of the posterior calf region as donor site for a free fasciocutaneous flap. Microsurgery 29:253–258
Spinner R, Howe B (2016) Leg. In: Tubbs RS (ed) Gray’s anatomy: the anatomical basis of clinical practice. Elsevier, Philadelphia, pp 1400–1417
Thione A, Valdatta L, Buoro M, Tuinder S, Mortarino C, Putz R (2004) The medial sural artery perforators: anatomic basis for a surgical plan. Ann Plast Surg 53:250–255
Torres LR, Teixeria WGJ, Setani EO, Wei TH, Zumiotti AV (2007) Skin flap of medial gastrocnemius muscle’s perforating arteries:an anatomical study. Acta Ortop Bras 15:40–42
Wong MZ, Wong CH, Tan BK, Chew KY, Tay SC (2012) Surgical anatomy of the medial sural artery perforator flap. J Reconstr Microsurg 28:555–560
Acknowledgements
The authors would like to thank Mr. Prem Panta, Lecturer (Statistician), Department of Community Medicine, for his assistance in data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors received no specific funding for this study.
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
This study underwent approval through Research and Institutional Review Committee (IRC) of Nepal Medical College and Teaching Hospital.
Rights and permissions
About this article
Cite this article
Basnet, L.M., Ghosh, S.K., Shrestha, S. et al. Anatomical study of medial sural artery and its perforators in Nepalese: an aid to reconstructive surgery. Surg Radiol Anat 40, 935–941 (2018). https://doi.org/10.1007/s00276-017-1956-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-017-1956-2