Abstract
Purpose
To evaluate the variations of the sternum and provide the prevalence of sternal foramen and its anatomical relationships.
Methods
In this retrospective study, 544 subjects ranging in age from 18 to 95 years were evaluated. Sternal variations, prevalence of sternal foramen and its anatomical relationships to mediastinal structures were examined with the axial, sagittal and coronal reformat images of the patients who underwent thoracic computerized tomography.
Results
In 500 subjects, following sternal variations were found: sternal sclerotic band in 120 (24%), sternal cleft in 3 (0.6%), sternal foramen in 26 (5.2%), focal cortical notch and defect in 44 (8.8%) patients. The manubriosternal fusion was partial in 65 (13%) patients and complete in 112 (22.4%) patients. The sternoxiphoid fusion was partial in 201 (40.2%) and complete in 153 (30.6%) patients. There was no xiphoid process in 9 patients (1.8%; 29–51 years; mean age 38 years). Xiphoidal ending types were as follows: single-ended 361 (72.2%), double-ended 125 (25%), and triple-ended xiphoid 5 (1%) patients. The sternal foramen was adjacent to the lung in 13 (2.6%), to the pericardium of heart in 3 (0.6%), and to mediastinal fat in 10 (2%) patients.
Conclusion
The sternum is a very critical anatomic structure of the anterior chest wall with several variations that can be confused with pathologic conditions. Radiologists’ familiarity with these variations is important for better radiologic evaluation in making differential diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The sternum and sternal joints are important anatomic structures of the anterior chest wall with frequent variations that may mimic pathologies on images or in autopsy series [20]. The sternum is adjacent to vital mediastinal organs [9]. Most variations of the sternum are asymptomatic and neglecting these variations prior to interventions to anterior chest wall may lead to serious complications [15]. In this step, plain radiography remains incapable of determining existing variations. Computed tomography (CT), on the other hand, allows easy evaluation on axial images and detailed examination is possible with three-plane reformat images (coronal, sagittal and axial). Therefore, it is necessary for the radiologists to become familiar with these normal variants, especially for making a differential diagnosis with pathologies and for protecting patients from potential complications [20].
In this educational study, we evaluated sternal variations of patients examined with thorax CT. We also tried to point out the presence of some asymptomatic sternal variations that may lead to serious complications.
Materials and methods
Patient population
This retrospective study was performed at Bakirkoy Dr. Sadi Konuk Research and Training Hospital between January 1st and May 15th of 2016. The study protocol was approved by the Institutional Review Board. We evaluated MDCT (multiple detector computed tomography) scans of 544 subjects aged between 18 and 95 years who were admitted to the radiology department with various indications.
We obtained all medical documents and demographic data of 544 patients from the data-processing center of our hospital. Patients with sternal fractures (19 cases) and history of heart operation (25 cases) were excluded from the study. Therefore, we included 500 patients to the study (285 men, 215 women; mean age 62 years). Patients who underwent repeated thoracic MDCT examinations were evaluated only once in the study and the first scans of patients were used for the evaluation.
MDCT protocol
The images were obtained using a 40-row MDCT scanner (Siemens Medical Solution, Erlanger, Germany). A routine thorax CT protocol was followed with 1-mm slice thickness in supine position. Tube voltage was 120 kV, effective mAs was adjusted by Siemens “CARE dose”. Gantry rotation was 0.5 s, collimation was 0.6 mm, pitch was 1.2 mm. Multiplanar reconstruction was made with 4-mm image thickness. All patients underwent imaging from the thoracic inlet to adrenal glands, including the sternum and the xiphoid.
Image analysis
All images were transferred to our local workstation (Leonardo, Siemens Medical Solution, Erlanger, Germany) for evaluation. Row data were reconstructed using bone algorithms. MPR (multi-planer reformation) reconstructions were obtained with Synapse PACS (Picture Archiving and Communication Systems), (Fujifilm Medical systems, USA). In addition to images in the axial plane, we obtained sagittal and coronal multiplanar reformat images and evaluated maximum intensity projections (MIP). R.T., who is an experienced radiologist, evaluated images. We evaluated the presence of the sternal sclerotic band, sternal cleft (developmental nonunion of the sternum at midline), sternal foramen (a round or oval defect of sternum), mediastinal relationships of the sternal foramen, sternal cortical defect, sternal notch (local vertical defect at anterior or posterior sternal cortices), manubriosternal fusion (MSF) degree, manubrioxiphoidal fusion (SXF) degree, types of xiphoidal ending (single, double or triple endings), and xiphoidal ligament calcification, suprasternal bone (bony fragments at the superior edge of the manubrium).
Results
Sternal sclerotic band, sternal cleft and sternal foramen
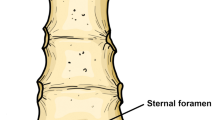
Sternal sclerotic bands (Fig. 1) were observed at the manubrium in 25 patients (5%) and sternal body in 95 patients (19%). More than half (64.4%) of manubrial sclerotic bands were located superiorly, and 82.2% of the sclerotic bands at the body were located at the inferior part. We observed a sternal cleft (Fig. 1) in only three patients which located at inferior part of the sternal body. We did not observe clefts at the manubrium. No sternal foramen was detected at the manubrium. A sternal foramen (Fig. 2) was observed in 26 (5.2%) patients at the sternal body inferiorly. The median foramen diameter was 6 mm (min 3–max 14 mm). In one patient, the foramen was continuous with a sternal cleft. The sternal foramen was adjacent to the lung in 13 (2.6%), to the pericardium-heart in 3 (0.6%), and to mediastinal fat in 10 (2%) patients.
Cortical sternal defect and sternal notch
In 44 (8.8%) patients focal, a cortical defect and notch (Fig. 3) was determined. The majority (72.7%) of sternal defects and notches were located inferiorly and at the mediastinal surface of the sternal body.
Manubriosternal and sternoxiphoidal fusions
The MSF and SXF were classified as completely and partially fused (Fig. 4). The MSF was complete in 112 (22.4%) and partial in 65 (13%) patients. The SFX was complete in 153 (30.6%) and partial in 201 (40.2%) patients. Patients with both MSF and SXF (n = 78, 15.6%) were younger than 45 years. The youngest one of the patients who had complete MSF and SXF fusion was 32 years old.
Xiphoidal ending and xiphoidal ligament calcification
The xiphoid process was absent in nine patients (1.8%). The xiphoidal ending was classified into three groups; single-ended (n = 361, 72.2%), double-ended (n = 125, 25%), and triple-ended xiphoid process (n = 5, 1%). Figure 5 shows xiphoidal endings.
Coronal reformatted images demonstrate xiphoidal endings a 51-year-old woman with absent xiphoidal ending, notice that the costal arch attaches directly to the sternal body, b 43-year-old man with single-ended xiphoid (arrowhead), c double-ended xiphoid is presented in a 54-year-old man (arrowhead), d 59-year-old woman with triple-ended xiphoid (arrowhead)
The xiphoidal ligament was calcified in 122 (24.4%) patients. In the majority of patients, it was either bilateral (74.6%) or present in patients older than 45 years (83.3%).
Suprasternal bone
The suprasternal bone (Fig. 6) was unilateral in 9 (1.8%) and bilateral in 6 (1.2%) patients.
Discussion
The sternum is an important anatomic structure of the chest wall and it has several variations that may be confused with pathologic conditions [3]. Two sternal halves ossify caudally from cartilaginous centers starting from the intrauterine 5th month. After birth, it completes its development and forms the manubrium and xiphoid process [20]. Failure of fusion of both halves results in sternal clefts and foramina. A complete sternal cleft is a very rare and serious anomaly [15]. Yekeler et al. [20] determined manubrial cleft in 0.6% and sternal cleft in 0.8% of patients. On the other hand, Macaluso et al. [11] examined a total of 122 patients and did not observe a sternal cleft. Similarly, we observed a thin sternal cleft in 3 (0.6%) patients which were located at the inferior part of the sternal body. In our study, we did not observe a manubrial cleft among our patient population.
In radiologic and anatomic studies, the frequency of sternal foramina was reported between 4.3 and 6.7% [9]. Yekeler et al. [20] reported a frequency of 4.5% in a Turkish population. Similarly, Gossner et al. [9] examined 352 chest CTs and reported a 4.5% frequency for sternal foramen presence. In our study, corresponding to previous studies, the sternal foramen frequency was 5.2%. It seems that the frequency of sternal foramen is not affected by ethnicity. Although the sternal foramen frequency has importance on an anatomical level, their relation to mediastinal structures gains clinical significance. The literature reports cases of fatal cardiac tamponade and pneumothorax after sternal biopsy or acupuncture [4, 10, 18]. Gossner et al. [9] reported that 53.3% of the foramina were adjacent to the lung, 33.3% were adjacent to mediastinal fat, and 20% were adjacent directly to pericardium/heart. Similarly, we observed that in 50% of patients the sternal foramen was adjacent to the lung, in 38.4% it was adjacent to mediastinal fat, and in 11.5% it was adjacent directly to pericardium/heart. Additionally, Papadimitriou et al. [12] found that the foramen at the inferior part of the sternum, where sternal foramen is most frequent, typically neighbored the right ventricle in 99.31% of cases. Therefore, awareness to the presence of sternal foramen and its relation to mediastinal structures is important to avoid unwanted complications.
Although sternal sclerotic band and cortical defect/sternal notch have no direct clinical importance, the knowledge of these variants is especially important for distinguishing them from posttraumatic fissures and fractures. Identifying these variations with X-ray graphy is challenging. Since CT is more sensitive for detecting osseous variations, radiologists’ familiarity with these anatomic variants in CT images is important [11, 13]. Non-existence of cortical irregularities and continuous cortex around the fissure are helpful findings for differential diagnosis [5, 14]. Yekeler et al. [20] observed vertical sclerotic bands in 37.1% of cases and cortical defects/sternal notches in 7.7%. We report similar frequencies for sclerotic band (24%) and cortical defect/notch (8.8%) among our population.
In forensic medicine, the MSF and SXF can be used for age and sex determination along with sternal morphometry [6, 8, 17]. After examining 330 patients aged from 0 to 100 years, Weaver et al. [16] concluded that sternum size increased significantly up to 30 years of age and the change in sternum size after 30 years of age was not meaningful. Yekeler et al. [20] reported the partial and complete MSF in 10 and 19.6% of patient, respectively. They also reported the partial and complete SXF in 32.4 and 30.3% of patients, respectively. Similarly, we observed the partial and complete MSF in 13 and 22.4% of cases, respectively. We also observed the partial and complete SXF in 40.2 and 30.6% of cases, respectively. We concluded that the reason behind higher rates of complete MSF and SXF fusion in our study is due to the high mean age of our study population.
Babinski et al. [2] reported a frequency of 17.5% for double-ended xiphoid. Similarly, El-Busaid et al. [7] reported a frequency of 20% for bifurcated/duplicated xiphoid among 80 cadavers. Akin et al. [1] evaluated the MDCT images of 327 patients and observed single-ended, double-ended, and triple-ended xiphoid processes in 62.6, 32.8, and 4.6% of patients, respectively. Xie et al. [19] examined 942 patients and they separated single-ended xiphoid as pointed (44.75%) and oval (41.04%). In some patients, there were no xiphoid. Yekeler et al. [20] examined 1000 patients and found the xiphoid to be single-ended in 71%, double-ended in 27.2%, and triple-ended in 0.7% of patients. Our results are concordant with the literature. The xiphoid was single-ended in 72.2%, double-ended in 25%, and triple-ended in 0.8% of patients. Rarely, the xiphoid process is reported to be absent. Yekeler et al. [20] reported the absence of the xiphoid in 1.1% among a population of one thousand. Similarly, we found that the xiphoid was absent in 1.8% of our patients. We also observed xiphoidal ligament calcification in 122 (24.4%) patients. In the majority (74.6%) of patients, the calcification was bilateral. Additionally, the majority (83.3%) of patients with ligament calcification was older than 45 years of age.
In conclusion, normal sternal variants are frequent. Asymptomatic sternal variations such as sternal foramen and sternal cleft are not infrequent variations and overlooking their presence may lead to fatal complications after sternal biopsy and acupuncture. Therefore, awareness regarding sternal variations among radiologists and residents is important for identifying and discriminating these variations from pathologies.
References
Akin K, Kosehan D, Topcu A, Koktener A (2011) Anatomic evaluation of the xiphoid process with 64-row multidetector computed tomography. Skelet Radiol 40:447–452
Babinski MA, de Lemos L, Babinski MS, Gonçalves MV, De Paula RC, Fernandes RM (2015) Frequency of sternal foramen evaluated by MDCT: a minor variation of great relevance. Surg Radiol Anat 37:287–291
Bayarogulları H, Yengil E, Davran R, Aglagul E, Karazincir S, Balcı A (2014) Evaluation of the postnatal development of the sternum and sternal variations using multidetector CT. Diagn Interv Radiol 20:82–89
Bhootra BL (2004) Fatality following a sternal bone marrow aspiration procedure: a case report. Med Sci Law 44:170–172
Cubuk S, Hamcan S (2016) Anatomic variations of sternum may mimic traumatic complications. Am J Emerg Med 34:1912.e1–1912.e2
Ekizoglu O, Hocaoglu E, Inci E, Bilgili MG, Solmaz D, Erdil I, Can IO (2014) Sex estimation from sternal measurements using multidetector computed tomography. Medicine 93:e240
El-Busaid H, Kaisha W, Hassanali J, Hassan S, Ogeng’o J, Mandela P (2012) Sternal foramina and variant xiphoid morphology in a Kenyan population. Folia Morphol 71:19–22
García-Parra P, Pérez Fernández Á, Djorojevic M, Botella M, Alemán I (2014) Sexual dimorphism of human sternum in a contemporary Spanish population. Forensic Sci Int 244:313.e1–313.e9
Gossner J (2013) Relationship of sternal foramina to vital structures of the chest: a computed tomography study. Anat Res Int 2013:780193
Halvorsen TB, Anda SS, Naess AB, Levang OW (1995) Fatal cardiac tamponade after acupuncture through congenital sternal foramen. Lancet 345:1175
Macaluso PJ, Lucena J (2014) Morphological variations of the anterior thoracic skeleton and their forensic significance: radiographic findings in a Spanish autopsy sample. Forensic Sci Int 241(220):e1–e7
Papadimitriou P, Chalkias A, Mastrokostopoulos A, Kapniari I, Xanthos T (2013) Anatomical structures underneath the sternum in healthy adults and implications for chest compressions. Am J Emerg Med 31:549–555
Rajiah P, Schoenhagen P (2013) The role of computed tomography in pre-procedural planning of cardiovascular surgery and intervention. Insights Imaging 4:671–689
Recinos G, Inaba K, Dubose J, Barmparas G, Teixeira PG, Talving P, Plurad D, Green D, Demetriades D (2009) Epidemiology of sternal fractures. Am Surg 75:401–404
Saccheri P, Sabbadini G, Toso F, Travan L (2012) A keyhole-shaped sternal defect in an ancient human skeleton. Surg Radiol Anat 34:965–968
Weaver AA, Schoell SL, Nguyen CM, Lynch SK, Stitzel JD (2014) Morphometric analysis of variation in the sternum with sex and age. J Morphol 275:1284–1299
Weaver AA, Nguyen CM, Schoell SL, Maldjian JA, Stitzel JD (2015) Image segmentation and registration algorithm to collect thoracic skeleton semilandmarks for characterization of age and sex-based thoracic morphology variation. Comput Biol Med 67:41–48
Wolochow MS (1995) Fatal cardiac tamponade through congenital sternal foramen. Lancet 346:442
Xie YZ, Wang BJ, Yun JS, Chung GH, Ma ZB, Li XJ, Kim IS, Chai OH, Han EH, Kim HT, Song CH (2014) Morphology of the human xiphoid process: dissection and radiography of cadavers and MDCT of patients. Surg Radiol Anat 36:209–217
Yekeler E, Tunacı M, Tunacı A, Dursun M, Acunas G (2006) Frequency of sternal variations and anomalies evaluated by MDCT. AJR Am J Roentgenol 186:956–960
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Local Ethics Committee.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Turkay, R., Inci, E., Ors, S. et al. Frequency of sternal variations in living individuals. Surg Radiol Anat 39, 1273–1278 (2017). https://doi.org/10.1007/s00276-017-1854-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-017-1854-7