Abstract
Purpose
The foramen cecum (FC) is a fine bony canal with the aperture located immediately anterior to the crista galli (CG). The venous structures in the regions of the FC and CG have been inconsistently described and are not well understood. Here we explore these veins using magnetic resonance imaging.
Materials and methods
We enrolled 101 patients who underwent contrast examinations and exhibited intact skin, skull, dura mater, and intracranial dural sinuses. Imaging data were obtained as thin-sliced, seamless sagittal sections and were transferred to a workstation for analysis.
Results
In 84 % of the patients, tubular-shaped venous extensions arose from the rostral end of the falx cerebri and were confirmed to lie in the FC. These extensions were supplied by the superior sagittal sinus or the frontal cortical vein, and were classified into four types: rudimental slight projections, short and straight extensions, long and straight channels, and long and tortuous channels. Furthermore, 27.7 % of the patients exhibited a distinct venous channel between the venous extension in the FC and the median vestibular submucosa of the nasal cavity. Among these channels, 81.5 % were connected to the vein lying in the FC via a short channel that vertically pierced the CG.
Conclusions
The FC contains tubular-shaped venous extensions that are supplied by the rostral end of the superior sagittal sinus or the frontal cortical vein. The cranial cavity, FC, and nasal cavity may be connected by a venous channel.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
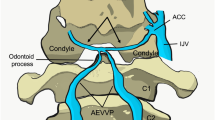
The crista galli (CG) is a vertical bony projection that is centrally located between the anterior parts of both cribriform plates. The anterior-posterior dimension of the CG is 12.7 ± 2.4 mm and the cranial-caudal dimension is 12.9 ± 2.5 mm [7]. The aperture of the foramen cecum (FC) is located immediately anterior to the CG, at the bottom of the anterior limit of the anterior cranial fossa. The posterior margin of the FC aperture forms a shallow groove that runs posterior toward the anterior margin of the CG (Fig. 1). The rostral end of the falx cerebri (FaCe) attaches to the dorsal ridge of the CG. Ossification of the CG is thought to begin at 1–2 months of age, and completed by approximately 24 months, with an anterior cartilaginous gap in the region of the FC [1]. The CG exhibits varying degrees of morphology and pneumatization [3, 6], which are thought to be exclusively derived from the frontal sinus, not from the ethmoid complex cells [16].
The endocranial appearance of a half-cut dry skull from an adult. Viewed from above (a), obliquely above (b, c), and laterally (d), showing the cribriform plate region. CP cribriform plate, EF ethmoidal foramen, CEF cribroethmoidal foramen, asterisk foramen cecum, OR orbital roof. The posterior margin of the foramen cecum forms a shallow groove that runs posterior to the anterior margin of the CG. The skull is owned by the Department of Neurological Surgery, Juntendo University Urayasu Hospital
Few studies have examined the development of the FC, thus it remains poorly understood. In the fourth to seventh gestational weeks, a transient dural diverticulum is thought to extend through the FC, travel through the prenasal space, and terminate at the skin of the nasal bridge. The subsequent normal regression of the dural diverticulum leaves a blind-end in the FC [10]. In the clinical setting, the FC can present as an unclear finding on neuroimages (Fig. 2). A previous study with computed tomography demonstrated that the length of the FC in an adult population was 4–15 mm [8]. In 1911, Rouvière reported two distinct foramina in the cribriform plate [13]. In later years, these foramina were found to locate at the areas of least resistance in the anterior part of the cribriform plate, predisposing to cerebrospinal fluid leaks, encephaloceles, or tumor spread [11].
There has been a general acceptance that the veins of the upper nasal region join a vein or veins that pass through the FC and connect to the most rostral part of the superior sagittal sinus (SSS). This anastomosis between the extracranial and intracranial venous systems has been presumed to provide an avenue of escape for intracranial venous blood after occlusion of the SSS or when the SSS is anomalous [14, 15]. Furthermore, this venous pathway has been assumed to be a portal of entry for inflammatory or tumoral processes that originate from the nose and extend into the intracranial cavity, as well as arteriovenous fistulas of the cribriform plate region. However, few of these speculations have not been verified, while there have been reports documenting contradictory results [6, 8, 17].
The present study aimed to explore the venous channels in the regions of the FC and CG using MR imaging.
Materials and methods
This prospective study evaluated 138 outpatients who presented to our institution between November 2010 and August 2015 for headache, dizziness, seizure, loss of consciousness, or sensorimotor disturbances. All the patients underwent cerebral MR imaging including contrast examinations, and eventually 101 patients who exhibited intact skin, skull, dura mater, and intracranial dural sinus were included in the study. Patients with brain tumors were excluded. The study population included 48 men and 53 women who were 18–77 years old (mean 50 years old). The present study was performed in accordance with our institution’s guidelines for human research, and the study’s design was approved by our ethics review board. Written informed consent was obtained from all 138 patients.
All examinations were performed using a 3.0-T MR scanner that was equipped with a 32-channel head coil (Achieva R2.6; Philips Medical Systems, Best, The Netherlands). Contrast examinations were performed via an intravenous infusion of gadolinium (0.1 mmol/kg) on a T1-weighted sequence, and were obtained in seamless sagittal sections of the entire cranial vault. The imaging parameters were: pulse repetition time, 4.1 ms; echo delay time, 1.92 ms; slice thickness, 1.00 mm; interslice gap, 0 mm; matrix, 320 × 320; field of view, 250 mm; flip angle, 13°; and scan duration, 4 min 25 s. All imaging data from the contrast examinations were transferred to a workstation (Virtual Place Lexus 64; AZE, Tokyo, Japan) and were analyzed independently by two authors (YY and HO).
Results
On obtained MR images, variable tubular-shaped venous extensions, arising from the anteroinferior edge of the FaCe and lying in the FC, were identified in 85 of the 101 patients (84 %). All of these extensions appeared as intensely enhanced single channels that travelled in the anteroinferior direction, with the lower edge ending adjacent to the posterior or inferior wall of the frontal sinus. In any of the cases these extensions did not pierce the marrow of the nasal bone or reach the superficial layer of the skin. In addition, there were no cases of tubular-shaped venous extensions that were comprised of two or more channels. In 82 patients (81.2 %), the rostral end of the SSS supplied the venous structure that was lying in the FC, and a frontal cortical vein supplied the venous structure in 19 cases (18.8 %). These tubular extensions were morphologically classified into four types: rudimental slight projections (RP), short and straight extensions (SE), long and straight channels (LS), and long and tortuous channels (LT) (Fig. 3). The most frequent type was RP (61.2 % of the 85 cases), followed by SE (22.4 %), LS (8.2 %), and LT (8.2 %) (Table 1).
Post-contrast midsagittal magnetic resonance images from different patients. Four types of tubular-shaped venous extension are shown (a–d arrow), arising from the rostral end of the superior sagittal sinus or the frontal cortical vein that lies in the foramen cecum. a Rudimental projection; b short extension, c long and straight channel, d long and tortuous channel; CV frontal cortical vein, FS frontal sinus
A distinct venous channel connecting the rostral end of the FaCe and the median vestibule of the nasal cavity was found in 28 cases (27.7 %). Along the near-midline, this channel passed through the marrow of the nasal bone, changed direction at the lower edge of the nasal bone, and eventually reached the vestibular submucosa of the nasal cavity (Fig. 4). In 22 cases (81.5 %), this channel was connected to the venous channel in the FC via a short pathway that pierced the CG in a vertical direction (Fig. 4). In 19 cases (67.9 %), the anastomotic channel between the cranial cavity and nasal cavity was visible in the same image with the tubular extensions in the FC, while in 9 cases (32.1 %) it was visible in the adjacent image. Peripheral anastomoses were not observed between these venous pathways.
Post-contrast midsagittal magnetic resonance images from different patients. A venous channel lying in the foramen cecum (a, b arrow) and a connecting venous pathway between the basal level of the crista galli (CG) to the nasal cavity (NC) (a, b double asterisks). The latter travels on the midline through the nasal bone (NB), changes direction at the lower edge of the nasal bone, and eventually reaches the vestibular submucosa of the nasal cavity (b double arrows). These veins are connected by a communicating pathway (a, b asterisk)
Discussion
For an accurate understanding of the congenital frontonasal lesions, comprehensive knowledge on the embryological development of the anterior neuropore and postnatal maturation of the frontonasal region is required [4, 9, 10]. In the present study, we observed tubular-shaped venous extensions that arose from the rostral end of the FaCe and were consistently delineated as single channel. They were supplied by the rostral end of the SSS in 81.2 % of the cases and the frontal cortical vein in 18.8 % of the cases. These tubular extensions ended at the posterior or inferior wall of the frontal sinus, which may partly explain the etiology of spontaneous cerebrospinal fluid rhinorrhea that emanates from an FC defect in the posterior frontal sinus table [2]. Given that the end of the FC is commonly adjacent to the frontal sinus wall, the length and shape of the FC may be, at least partially, regulated by the development of the frontal sinus.
The rostral end of the SSS exhibits variable morphology, and its classification into four types was proposed based on embryological development: the classic anatomy with a fully developed rostral SSS, duplication of the rostral SSS, a complete or bilateral hypoplastic rostral SSS, and a unilateral hypoplastic rostral SSS [14]. In the present study, we did not ascertain the relationships between different types of venous channels in the FC and morphologies of the rostral SSS. This topic may need further investigation in the future.
San Millán Ruiz et al. reported two unique cases of angiographically verified intracranial venous drainage of the nasal mucosa, which were thought to associate with asymptomatic hypoplasia of the SSS [15]. However, in those cases, the exact site of passage for the ascending nasal vein through the anterior fossa floor was not ascertained. In the present study, 28 of 101 patients (27.7 %) exhibited a distinct venous channel that connected the rostral end of the FaCe to the vestibule of the nasal cavity, which indicates that a normal venous channel may connect the nasal and cranial cavities. At this time, its functional implications are unclear. Given that most of the anastomotic channels were connected to the vein lying in the FC, it is possible that these channels may function together.
The CG is an important surgical boundary in endoscopic transcribriform surgery, and closely located to two distinct foramina: the ethmoidal foramen and the cribroethmoidal foramen [11, 13]. The former is located in the anteromedial part of the cribriform plate, immediately lateral to the CG, and contains a process of the dura mater. The latter is found at a greater lateral distance and is reported to contain the anterior ethmoidal nerve (Fig. 1). Given the presence of a dura mater process, a fraction of the ethmoidal foramina may transmit an anastomotic channel between the intracranial and extracranial venous systems.
Ranieri et al. documented an interesting case of a 49-year-old woman who presented with chronic migraine-associated headache attacks, which were followed by epistaxis and resolution or significant improvement in her pain. The patient also exhibited symptoms suggesting an increased intracranial pressure, and MR venography revealed a bilateral narrowing of the transverse sinuses. The exact underlying mechanism for these phenomena was unclear [12]. We assume that an anastomotic channel between the rostral end of the SSS/frontal cortical vein and the nasal cavity might partly explain the etiology of these phenomena.
Toriumi et al. have documented a subcutaneous venous system that exclusively existed above the muscular layer of the nasal region. Furthermore, most of those veins were found to drain into the facial vein and angular vein [18]. Based on these findings, we hypothesize that the anastomotic channel in the present study which connected the intracranial and nasal cavities may convey venous flow collecting from the nasal mucosa into the cranial cavity. The channel also may play a role in the spread of nasal and sinus infections into the cranial cavity. Although infrequent, these pathologies have been documented to occur cerebral venous/sinus thrombophlebitis, cerebral abscess, and subdural empyema [5, 19].
The present study evaluated only a relatively small number of cases, and the obtained findings and hypotheses need critical validation in a larger patient population. Nevertheless, we believe that our findings can be a help for a better understanding of the venous connection between the cranial cavity and nasal region.
Conclusions
The FC contains a tubular-shaped venous extension that is supplied by the rostral end of the SSS or frontal cortical vein. The cranial cavity, FC, and nasal cavity may be connected by a venous channel.
References
Belden CJ, Mancuso AA, Kotzur IM (1997) The developing anterior skull base: CT appearance from birth to 2 years of age. AJNR Am J Neuroradiol 18:811–818
Gaffey MM, Friedel ME, Fatterpekar GM, Liu JK, Eloy JA (2012) Spontaneous cerebrospinal fluid rhinorrhea of the foramen cecum in adulthood. Arch Otolaryngol Head Neck Surg 138:79–82
Hajiioannou J, Owens D, Whittet HB (2010) Evaluation of anatomical variation of the crista galli using computed tomography. Clin Anat 23:370–373
Hedlund G (2006) Congenital frontonasal masses: developmental anatomy, malformations, and MR imaging. Pediatr Radiol 36:647–662
Jones NS, Walker JL, Bassi S, Jones T, Punt J (2002) The intracranial complications of rhinosinusitis: can they be prevented? Laryngoscope 112:59–63
Kaplan HA, Browder A, Browder J (1973) Nasal venous drainage and foramen caecum. Laryngoscope 83:327–329
Lee JM, Ransom E, Lee JY, Palmer JN, Chiu AG (2011) Endoscopic anterior skull base surgery: intraoperative considerations of the crista galli. Skull Base 21:83–86
Lewińska-Śmiłek B, Szaro P, Ciszek B (2013) Anatomy of the adult foramen cecum. Eur J Anat 17:142–145
Mahatumarat C, Taecholarn C, Rojvachiranonda N (1999) Spontaneous closure of bony defect in a frontoethmoidal encephalomeningocele patient. J Craniofac Surg 10:149–154
Müller F, O’Rahilly R (1986) The development of the human brain and the closure of the rostral neuropore at stage 11. Anat Embryol (Berl) 175:205–222
Patron V, Berkaoui J, Jankowski R, Lechapt-Zaicman E, Moreau S, Hitter M (2015) The forgotten foramina: a study of the anterior cribriform plate. Surg Radiol Anat 37:835–840
Ranieri A, Topa A, Cavaliere M, De Simone R (2014) Recurrent epistaxis following stabbing headache responsive to acetazolamide. Neurol Sci 35(Suppl 1):181–183
Rouvière H (1911) Précis d‘anatomie et de dissection. Masson, Paris (French)
San Millán Ruíz D, Fasel JH, Gailloud P (2012) Unilateral hypoplasia of the rostral end of the superior sagittal sinus. AJNR Am J Neuroradiol 33:286–291
San Millán Ruíz D, Gailloud P, Rüfenacht DA, Yilmaz H, Fasel JH (2006) Anomalous intracranial drainage of the nasal mucosa: a vein of the foramen caecum? AJNR Am J Neuroradiol 27:129–131
Som PM, Park EE, Naidich TP, Lawson W (2009) Crista galli pneumatization is an extension of the adjacent frontal sinuses. AJNR Am J Neuroradiol 30:31–33
Thewissen JG (1989) Mammalian frontal diploic vein and the human foramen caecum. Anat Rec 223:242–244
Toriumi DM, Mueller RA, Grosch T, Bhattacharyya TK, Larrabee WF Jr (1996) Vascular anatomy of the nose and the external rhinoplasty approach. Arch Otolaryngol Head Neck Surg 122:24–34
Younis RT, Lazar RH, Anand VK (2002) Intracranial complications of sinusitis: a 15-year review of 39 cases. Ear Nose Throat J 81:636–638
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests concerning the materials or methods used in this study or the findings specified in this study.
Rights and permissions
About this article
Cite this article
Tsutsumi, S., Ono, H. & Yasumoto, Y. A possible venous connection between the cranial and nasal cavity. Surg Radiol Anat 38, 911–916 (2016). https://doi.org/10.1007/s00276-016-1650-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-016-1650-9