Abstract
Objective
To assess the relationship between the maximum volume of lumbar vertebral bodies and patient morphological features. Knowledge of the volume of the vertebral body is useful when performing vertebroplasty and kyphoplasty.
Methods
129 patients (18–85 years) were included consecutively over an 8-month period. All had been subject to abdominopelvic CT scans. The weight, height and body mass index (BMI) were known. The volume of each vertebral body was calculated using the formula V = π R 2. H (V = volume, R = radius, H = height). A statistical analysis of the data divided into three groups, men/women, men only and women only, was conducted by calculating the Pearson correlation coefficient.
Results
The volume of the vertebral body increased from L1 to L4, but the volume of the L5 vertebral body was lower than that of L3 and L4 in all three groups. The volumes of the vertebral bodies were greater in men than in women. Calculating the correlation coefficient showed that the variable most correlated with volume was patient’s height in both the men/women and women-only groups, while the most correlated variable in the male-only group was weight. Vertebral height was the variable most correlated with overall height in all three groups.
Conclusion
There is a wide variability in the volume of lumbar vertebrae. The volume of the vertebral body appears to vary not only with a person’s height but also their weight. The vertebral body seems to expand with weight in men.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vertebral compression fractures (VCFs) are defined by the EPOS (European Prospective Osteoporosis Study) group by two criteria [1]. The first is morphometric and results in a decrease of 20 % or more in the anterior, medial or posterior vertebral body height, leading to an absolute reduction of the same height by at least 4 mm [3]. The second, McCloskey method, is qualitative, where the vertebral body must meet deformation criteria characterized by its anterior (Ha), medial (Hm), posterior (Hp) and predicted posterior (Hpp) heights (the latter obtained using data from four adjacent vertebrae). There is deformation when at least two of the following five ratios (Ha/Hp; Hm/Hp; Ha/Hpp; Hm/Hpp; Hp/Hpp) are inferior to a defined threshold [12]. Three types of deformation are described by calculating the different ratios: anterior (Ha/Hp and Ha/Hpp), posterior (Hm/Hp and Hm/Hpp) and crush deformity (Ha/Hpp and Hp/Hpp). In addition, there are other fracture definitions and classifications, such as Genant’s, which is a semi-quantitative classification of vertebral compression fractures based on radiological criteria [8]. This latter technique uses the location (anterior, medial or posterior) and the severity of the fracture (four stages; 0: no fracture; 1: mild; 2: moderate; 3: severe).
VCFs are usually low-energy fractures in osteoporotic patients. There are 50–70,000 vertebral fracture cases per year in France alone, 700,000 in the United States and 450,000 throughout Europe [6, 7, 14]. These are far more common than femoral head fractures (300,000 in USA) or distal radius fractures (200,000 in USA). Therefore, this type of fracture has become a real public health issue. Other causes of vertebral fractures are high-energy injuries and (primary or secondary) neoplasms [14].
The conventional treatment for uncomplicated osteoporotic VCFs is usually medical, sometimes in association with the wearing of a corset. When this fails, percutaneous vertebroplasty or kyphoplasty techniques, used to expand the vertebral body by injecting biological cement into it, may be proposed, although there is no current consensus [4, 14]. The difference between these two techniques is that in kyphoplasty, a balloon is inserted and inflated prior to the injection of the biological cement. Both techniques provide a significant reduction in early post-operative pain [1, 4]. This treatment can also be offered to young patients with traumatic fractures [10, 14]. There are also open osteosynthesis procedures available.
The lumbar spine consists of five individual vertebrae, numbered L1 to L5. Lumbar vertebral bodies are much larger than those of other vertebrae. They are wider in the front and are kidney shaped. They form the boundary at the front with the small triangular vertebral foramen and extend posteriorly and laterally into thick pedicles. There have been few studies looking at the volumes of vertebral bodies [9, 13].
The purpose of this study was to investigate the relationship between the maximum volume of the vertebral bodies from L1 to L5 and patient morphological data, including weight, overall height and body mass index (BMI), using a simple extrapolation. Knowing the volume of the vertebral body can be very useful in vertebroplasty or kyphoplasty procedures.
Materials and methods
This was an epidemiological, radio-anatomical, retrospective, observational and descriptive study.
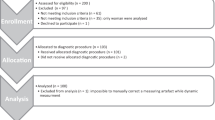
One hundred and twenty-nine patients, aged from 18 to 85 years, from the visceral surgery unit at Compiegne Hospital, including 77 men with a mean age of 62.1 years (21–85) and 52 women with a mean age of 54.1 years (19–82) were included consecutively over a period of 8 months (from 1st July, 2012 to 1st March, 2013). All had undergone an abdominopelvic CT scan, with or without contrast agent injection, using a standardized protocol with 120 kV, 50 mA, pitch of 0.885, a 400 mm field of view and 3 mm section thickness, either during hospitalization or in the year preceding hospitalization. Cross-sectional and frontal scans were taken. Weight and height were noted and body mass index (BMI = weight/height2) was calculated for each patient from the computerized medical records (DxCare®, Medasys®).
The exclusion criteria were: presence of secondary osteolytic or osteoblastic vertebral lesions, vertebral compression fractures, arthrodesis and signs of discospondylitis, kyphoplasty, or scoliosis.
This study of the vertebral bodies of all lumbar vertebrae thus covered a total of 645 vertebral bodies.
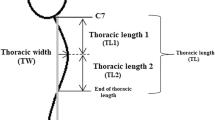
The abdominopelvic CT scans were analyzed using T2 Viewer® medical imaging software (T2 Technology®). The scanned sections were 3 mm thick. The pixel size was 1.56 mm. Calculating the volume of the vertebral body was based on a mathematical model comparing it to a cylinder. The volume was calculated by the formula V = π.R 2.H, where V was the volume of the vertebral body in cm3, R the radius of the vertebra in mm and H its height in mm. The radius was measured on transverse sections of the CT scan at mid-height of the vertebral pedicle and included the cortical bone (Fig. 1). Vertebral body height (in millimeters) was determined at the mid-vertebral level in the frontal plane and also included the cortical bone. For each of these distances, two measurements on two successive sections were made and when there was a discrepancy of more than 10 % (i.e., more than 2 mm), a third measurement enabled us to take the median of the three values. This model was only an approximation of the maximum volume of the vertebral body.
Then intra-observer variability was calculated thanks to the intraclass correlation coefficient between measurements made on the same CT scan twice. Calculation was made using R Software v 3.0.2 (The R Foundation for Statistical Computing).
All data were collected in the form of a table and a statistical analysis of the data was carried out by calculating the Pearson correlation coefficient. This correlation coefficient gives the proportions of the variance of the volume that are attributable to the variance of the size, weight and/or BMI, such that the closer this coefficient is to 1 or −1, the greater is the correlation. The statistical significance threshold of the correlation was set at 5 % (p = 0.05). Using the Student t test, the statistical calculation was expressed as a linear regression.
Four analyses were carried out on the data collected. The first was on the total population and the second separated men and women. A third excluded patients with BMI values <16 kg/m2 or >30 kg/m2. Finally, the fourth looked for a correlation between weight and overall height and the radius and height of the vertebrae.
Results
Out of the 139 patients enrolled, 10 patients were excluded for VCFs, four for secondary lesions, one for arthrodesis, one for prior kyphoplasty and two others for scoliosis.
The average weight of the 129 patients included was 76.6 ± 18.6 kg (ranging from 36 to 132). The average height was 170.3 ± 9.1 cm (150–196). The mean BMI was 26.3 ± 5.9 kg/m2 (ranging from 13.5 to 52.6).
The intraclass correlation coefficient was 0.79.
The volume of the vertebral body increased from L1 to L4 in the male/female, male-only and female-only groups. The volume of the L5 vertebral body was less than that of L3 and L4 in all three groups (Table 1).
Vertebral body volume was greater in men than in women. The radius was greater in men than in women for a given vertebra and this difference was evident at all lumbar levels. In terms of vertebral height, no differences were detected between the sexes (Table 2).
For all lumbar vertebrae, calculating the correlation coefficient showed that the variable most highly correlated with vertebral body volume was overall height in the male/female and female-only groups, with the most correlated variable being weight in the male-only group (Table 3).
These results were enhanced by the exclusion of patients with BMI values <16 kg/m2 (2 women) or >30 kg/m2 (12 women and 18 men) (Table 3).
In the latter analysis, calculating the correlation coefficient showed that the variable most correlated with vertebral body volume was weight in the male group and overall height in the female group, whereas in the male/female group, both weight and overall height variables correlated with vertebral body volume. In addition, the correlation coefficient between BMI and vertebral body volume in the women-only group was close to zero.
For all lumbar vertebrae, calculating the correlation coefficient between the variables overall height and weight and vertebral height and radius showed that in the male/female group, the radius was more closely correlated with height than weight. In contrast, in the male group the variable most correlated to the radius was weight, while in women this was overall height. Vertebral height was the variable most correlated with overall height in all three groups. Finally, in the male-only group, the correlation coefficient between weight and vertebral radius was greater than that between weight and vertebral height (Table 4).
Discussion
One of the main biases of this study is how the volume is calculated, as it is based on a cylinder model of the vertebral bodies and thus an approximation of body volume. A wedge-shaped model [11] could have been used but the main objective of the study was not to obtain an accurate calculation of the volume of the vertebral body, but to see whether there was a correlation between the morphological data and these vertebral body volumes. However, this calculation method was simple and reproducible. In addition, the study was not performed blind because the measurements were collected and analyzed by the investigators.
There was a wide inter-individual variability regarding the volume of the L1–L5 vertebral bodies, which could be explained by the wide inclusion criteria. The volume of lumbar vertebral bodies was greater in men than in women (p < 0.0001). Their volume increased from L1 to L4, but that of L5 appeared to be less than L3, which is probably due to how the volumes were calculated. The height of the vertebral body was calculated using only the frontal and not the sagittal plane; the radius was measured using a transverse plane. However, L5 tends to slope downward and backwards relative to the standard anatomical position. Therefore, the applicability of the results is weak in relation to L5. A study using multi-planar medical image reconstruction (MPR) software is necessary to choose the best angle to obtain a more accurate measurement of the vertebral body.
This study is a preliminary investigation into whether there is a correlation between vertebral body volume and a person’s height, weight or BMI.
Despite these drawbacks, our results relating to the volume of L5 appear to be in agreement with those found by Limthongkul et al. (men: 42.52 ± 10.14 cm3 and women: 28.80 ± 2.63 cm3) compared to L4 (men: 44.61 ± 9.96 cm3 and women: 30.19 ± 3.07 cm3) and L3 (men: 44.21 ± 10.14 cm3 and women: 29.54 ± 4.4 cm3) [9]. In this study, which analyzed the thoracic and lumbar vertebral body volumes of 40 patients, the volumes were accurately measured using image guidance software (BrainLAB®).
Vertebral volume increases gradually down to the sacrum. These morphological differences are directly related to the progressive increase in load on the body. Therefore, it makes sense that the volume of the vertebral body varies not only with the patient’s height but also with his or her weight.
These concepts are reflected in our results since the weight and overall height variables are both correlated with the volume of the lumbar vertebral bodies, although overall height seems to be a better indicator than weight in the combined male/female group. However, this difference disappears in the analysis of the BMI 16–30 group. In addition, it should be noted that in the male-only group, weight seems to be more correlated with lumbar vertebral body volume, while in the women-only group, overall height is the variable most correlated with vertebral body volume. The reason for analyzing the BMI 16–30 subgroup was to exclude patients whose body mass index was too extreme. This helped to potentiate the results and at the same time hardly reduced the power of the study, as only 32 patients were excluded out of the initial 129 patients. In addition, in the women-only group, volume was highly correlated with height, especially for L1. BMI, on the other hand appeared to have no correlation with vertebral body volume (0.001 for L1). This can be explained by the way the BMI was calculated, as weight was only moderately correlated (0.14 for L1) with vertebral body volume in this group. Finally, spine’s ability to adapt to excess fat seemed to have its limits since excluding obese patients potentiated the results obtained.
In addition, the height of the vertebrae was similar in both male and female groups, the difference in vertebral body volume being explained by a difference in vertebral body radius between the two sexes. The radius is indeed greater in men than in women. In addition it was found that the correlation between weight and vertebral radius was greater than that between weight and vertebral height in the male-only group. The vertebral body in men, therefore, seems to expand with weight. Finally, the height of the vertebrae is more closely correlated with the person’s height than with their weight in all 3 groups. It is, therefore, the height of the vertebrae that determines the overall height of the individual.
In vitro studies on the treatment of vertebral compression fractures using vertebroplasty or kyphoplasty showed that a cement volume of just 2 cm3 was capable of restoring the height of the vertebral body [2] and with 8 cm3 it was possible to restore vertebral body rigidity [2]. The results of this surgical technique are still controversial. The FREE study published in February 2011 brought together 300 patients [4] and resulted in a significant reduction in back pain after 7 days (VAS = −2.2 for the kyphoplasty versus the non-surgical group, p < 0.0001) and at all subsequent visits. A randomized controlled trial in 2009 compared the injection of small amounts of cement (3 cm3) with a placebo control procedure limited to inserting a needle into the vertebral laminae. No significant difference was found in immediate post-operative pain or after 6 months [5].
Other techniques include a cement injection of up to 12 cm3. In fact, the injection volume is not consensual and is left to the discretion of the physician. However, the injection pressure should be evaluated since this increases the risk of cement leakage, and this applies to both percutaneous techniques.
Finally, the application of this study would enable the maximum volume of the lumbar vertebral body to be defined (as a linear function), in men (based on their weight) and women (based on their height).
Conclusion
Vertebral body volume increases from L1 to L4. The volume of L5 is less than that of L3 and L4. These results are also reflected in the analysis of male-only and female-only groups. Overall height is the variable most correlated with vertebral body volume in the men/women and women-only groups, but it appears that in men-only group, it is weight that is most correlated with vertebral body volume.
In addition, vertebral height is more correlated with overall height than weight in all groups, while vertebral radius is more correlated with weight in men, while in women it is more correlated with their height. There is a greater correlation between vertebral radius and weight in men than vertebral height and weight.
As it is now possible to calculate the maximum volume of a vertebral body based on overall height and weight, this should be taken into account when considering vertebroplasty and kyphoplasty studies.
The authors declare that they have no conflict of interest. The experiments comply with the current laws.
References
Barr JD, Barr MS, Lemly TJ, McCann RM (2000) Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine 25(8):923–928
Belkoff SM, Mathis JM, Jasper LE, Deramond H (2001) The biomechanics of vertebroplasty: the effect of cement volume on mechanical behavior. Spine 26:1537–1541
Black D, Palermo L, Nevitt MC, Genant HK, Christensen L, Cummings SR (1999) For the study of Osteoporotic Fractures Research Group Defining incident vertebral deformity: a prospective comparison of several approaches. J Bone Miner Res 14:90–101
Boonen S, Van Meirhaeghe J, Bastian L, Cummings SR, Ranstam J, Tillman JB et al (2011) Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res 26(7):1627–1637
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C et al (2009) A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 361:557–568
Curran D, Maravic M, Kiefer P, Tochon V, Fardellone P (2010) Epidemiology of osteoporosis-related fractures in France: a literature review. Joint Bone Spine 77(6):546–551
Felsenberg D, Silman AJ, Lunt M, Armbrecht G, Ismail AA et al (2002) Incidence of vertebral fracture in Europe: results from the European Prospective Osteoporosis Study (EPOS European Prospective Osteoporosis Study (EPOS) Group. J Bone Miner Res 17(4):716–724
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8(9):1137–1148
Limthongkul W, Karaikovic EE, Savage JW, Markovic A (2010) Volumetric analysis of thoracic and lumbar vertebral bodies. Spine J. 10(2):153–158
Maestretti G, Cremer C, Otten P, Jakob RP (2007) Prospective study of stand-alone balloon kyphoplasty with calcium phosphate cement augmentation in traumatic fractures. Eur Spine J 16–5:601–610
Matsumoto M, Okada E, Kaneko Y et al (2011) Wedging of vertebral bodies at the thoracolumbar junction in asymptomatic healthy subjects on magnetic resonance imaging. Surg Radiol Anat 33(3):223–228
McCloskey EV, Spector TD, Eyres KS, Fern ED, O’Rourke N, Vasikaran S et al (1993) The assessment of vertebral deformity: a method for use in population studies and clinical trials. Osteoporos Int 3:138–147
Odaci E, Sahin B, Sonmez OF, Kaplan S, Bas O, Bilgic S et al (2003) Rapid estimation of the vertebral body volume: a combination of the Cavalieri principle and computed tomography images. Eur J Radiol 48:316–326
Saget M, Teyssédou S, Pries P, Grau-Ortiz M, Vendeuvre T, Gayet LE (2011) La cyphoplastie vertébrale par ballonnets: bilan de 3 années d’expérience. http://www.maitrise-orthopedique.com/articles/la-cyphoplastie-vertebrale-par-ballonets-bilan-de-3-annees-dexperience-33. Accessed May 2015
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Caula, A., Metmer, G. & Havet, E. Anthropometric approach to lumbar vertebral body volumes. Surg Radiol Anat 38, 303–308 (2016). https://doi.org/10.1007/s00276-015-1552-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-015-1552-2