Abstract
In the surgical setting, horseshoe kidneys (HKs) may be a cause for confusion because of their complicated morphology, especially in the vicinity of the vascular and urinary collecting systems around the isthmus of the HK. In the patients with HK, analysis of the anatomical structure of the isthmus is both useful and necessary. The aim of this study is to observe the vascular and collecting system of the HK using anatomical and contrast imaging technique, then make use of the knowledge for clinical anatomy. A HK voluntarily donated post-mortem to our department in 2013 by an 80-year-old woman was dissected. The gross anatomy of this HK was reported. In this study, we additionally analyzed this kidney using micro-computed tomography with both colored and colorless contrast media after the kidney was made transparent. Contrast imaging clearly revealed that each of the five renal arteries, including the three surplus renal arteries, entering the HK distributed blood to different regions. Neither side of the urinary collecting system crossed the midline of the isthmus. Two surplus renal veins emerged from the HK and two ureters descended dorsal to the isthmus. These observations show that gross anatomical observation and contrast imaging of the HK can provide very important surgical information. Our results can contribute to both better understanding of fundamental knowledge and progress in the surgery of HKs such as in the setting of biopsy and transplantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The horseshoe kidney (HK) is a major congenital abnormality of the kidney first described by Berengario in 1522. The incidence of HK is 0.27 % (7 of 2595) [4]. In >90 % of HKs, the right and left kidneys are fused at their lower poles. According to Farman, 15 % of an HK consists of fibrous tissues and the other 85 % of renal parenchymal tissues [1]. Individuals with HKs are more likely to have hydronephrosis, infections, and renal stones and may experience problems during transplantation and biopsy [2, 5, 9]. HKs have been the focus of anatomical studies carried out all over the world and for several centuries. Recent studies have used radiological imaging to examine the vascular anomalies associated with HKs. In the surgical setting, HKs may be a cause for confusion because of their complicated morphology with respect to the vascular and urinary collecting systems, especially around the isthmus. Therefore, anatomical knowledge of a HK, including its position, vascular systems, and urinary collecting systems, but especially the anatomical structure of the isthmus, is extremely important. We previously reported the gross anatomical observation of a HK donated to our department [3]. Here, we report the contrast imaging findings of the vascular and collecting systems in this kidney and discuss the clinical implications of the determined anatomy.
Case report
The HK was voluntarily donated post-mortem to our department, by an 80-year-old woman for research and education purposes. Her kidney was free from disease. This study was performed in keeping with the requirements of the Declaration of Helsinki.
Observational methods
The HK was first subjected to gross anatomical dissection as described in a previous report [3]. It was then made transparent and analyzed using contrast imaging. The transparency procedure was as follows: the specimen was immersed in 10 % formalin for 1 month and then washed under running water for 30 min, followed by incubation in 3 % potassium hydroxide (containing 0.2 mL of 3 % hydrogen peroxide per 100 mL) for 3 months for maceration and depigmentation. Three colored derivatives of contrast medium (blue, yellow, red; Microfil; Flow Tech, Hartford, CT, USA) were then injected into all five renal arteries: blue contrast medium was injected into the two upper renal arteries, which entered into the upper part of the renal hilum as normal renal arteries; yellow contrast medium was injected into the two middle renal arteries, which entered the lower part of the renal hilum on both sides; and red contrast medium was injected into a renal artery entering the lower part of the isthmus. In addition, colorless contrast dye (Iopamiron Inj, Syringe; Bayer Yakuhin, Osaka, Japan) was injected into the right and left ureters. The contrast-enhanced HK was then examined using micro-computed tomography (micro-CT; R_mCT; Rigaku, Tokyo, Japan). Because the HK was too large for a single micro-CT scan, it was scanned twice and the two images were merged on the computer.
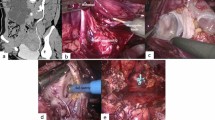
Shape, size, and position of the HK (Fig. 1a)
The right and left kidneys were fused at their lower poles by the isthmus, forming a typical U-shaped HK. The isthmus was located ventral to the abdominal aorta and inferior vena cava, and the inferior mesenteric artery descended dorsal to the isthmus. The upper poles of both sides of the kidney were located at the level of the middle region of the second lumbar vertebra. The bottom of the isthmus was located at the lower margin of the fourth lumbar vertebra. The fixed HK weighed 215.0 g. The width of the right kidney was 4.0 cm, and that of the left 4.3 cm. The isthmus was 3.6 cm long and maximally 1.8 cm thick. The distance between the inferior border of the isthmus and the bifurcation of the common iliac arteries was 1.5 cm.
a Dissected HK (reuse with permission from Kurume Igakukai Zasshi). b Histology of the isthmus. c Arterial and venous systems of the horseshoe kidney. AA abdominal aorta, BC Bowman’s capsule, CT celiac trunk, GC glomerular capillary, IMA inferior mesenteric artery, IVC inferior vena cava, LA left renal artery, LAV left adrenal vein, LC left common iliac vein, LO left ovarian vein, LP left renal pelvis, LU left ureter, LV left renal vein, RA right renal artery, RC right common iliac artery, RO right ovarian vein, RP right renal pelvis, RU right ureter, RV right renal vein, SMA superior mesenteric artery, SRA1 first surplus renal artery, SRA2 second surplus renal artery, SRA3 third surplus renal artery, SRV1 first surplus renal vein, SRV2 second surplus renal vein. Scale bar 50 µm
Renal hilum, pelvis and ureter (Fig. 1a)
The hilum of each kidney opened widely in the ventral direction. The right renal hilum was 7.5 cm long and 2.7 cm wide, and the left hilum was 7.6 cm long and 2.5 cm wide. The right and left pelvises expanded to the front. There were two ureters, both of which descended without forming shallow grooves on the ventral surface of the kidney.
Arterial system (Fig. 1c)
The abdominal aorta descended on the dorsal side of the HK. The right and left common iliac arteries branched at the level of the lower border of the fourth lumbar vertebra. The right renal artery (6 mm in diameter) arose from the right side of the abdominal aorta and was slightly lower than the left renal artery arising from the left side of the abdominal aorta (5 mm in diameter). Each renal artery entered the upper part of the renal hila on the respective sides, at the level of the middle part of the second lumbar vertebra. The inferior mesenteric artery (IMA) arose from the ventral side of the abdominal aorta at the level of the middle part of the third lumbar vertebra. There were three surplus renal arteries (SRAs). The first SRA (3 mm in diameter) emerged from the right side of the abdominal aorta slightly below the level of the IMA and entered the inferior part of the right renal hilum. The second SRA (6 mm in diameter) emerged from the left side of the abdominal aorta slightly below the first SRA and entered the inferior part of the left renal hilum. The third SRA (5 mm in diameter) emerged from the medial side of the origin of the right common iliac artery and entered the inferior isthmus on the right side. There were no abnormalities in either the lumbar arteries or the median sacral artery.
Venous system (Fig. 1c)
The inferior vena cava (IVC) ascended alongside the abdominal aorta. Three veins from the right side of the renal hilum joined the right ovarian veins; the right renal vein then entered the IVC. On the left side, the left ovarian veins entered at the lower wall of the left renal vein, formed by three distinct veins. The two left ovarian veins ascended and joined before entering the left renal vein. The left adrenal vein joined at the upper wall of the left renal vein, and the vein arising from the lower part of the hilum joined the left renal vein. The first of the two surplus renal veins (SRVs) arose from the upper part of the right hilum and entered into the dorsal side of the IVC at a position slightly higher than the right renal vein. The second SRV arose from the dorsal side of the lower part of the isthmus, then descended, accompanying the third SRA, then joined a vein arising from lateral side of the left common iliac vein, before entering the right ovarian vein.
Histological findings (Fig. 1b)
To observe the isthmus histologically, tissue from the dorsal side of the isthmus was removed, prepared as paraffin-embedded sections, and stained with hematoxylin and eosin. Histological findings showed that the isthmus comprised renal parenchyma, including Bowman’s capsule, glomerular capillaries, and renal tubules.
Contrast imaging of the arteries and collecting systems (Fig. 2)
Figure 2a shows the distribution of the five renal arteries. The right renal artery supplied the upper half of the right kidney, including the upper half of the right renal hilum (right blue area). The left renal artery supplied the upper half of the left kidney, including the upper half of the left renal hilum (left blue area). Both arteries extended inferolaterally. The first SRA supplied the lower half of the right kidney, including the lower half of the right renal hilum (right yellow area); the second SRA supplied the lower half of the left kidney, including the lower half of the left renal hilum (left yellow area). The distribution area of the right SRA was slightly narrower than that of the left SRA, based on the color-contrasted images. The third SRA arose from the right common iliac artery, supplied the isthmus, and extended along its right side (red area). The third SRA did not supply the renal hilum on either side. Figure 2c shows the image obtained by ureterography using colorless contrast medium. The many minor renal calices united to form the major calyx on each side and several major calices united to form the renal pelvis, which continued to the ureters. The collecting systems were distributed throughout the kidney except at the isthmus. The ureters on both sides seemed to be slightly enlarged. The right major renal calyx continued only into the right ureter, and the left major renal calyx only into the left ureter. There were no collecting systems crossing the midline of the isthmus. Figure 2b is a diagram of the renal arteries and collecting systems. The renal arteries on both sides and the first and second SRAs supplied a region close to the renal calyx, whereas the third SRA entered the isthmus on the right side and was very close only to the right renal calyx.
a Contrast image of the colored renal arteries. b Diagram of the renal arteries and collecting systems, and their regions of distribution. Blue renal arteries, yellow first and second surplus renal arteries, red third surplus renal artery, orange renal calyx and ureters. c Contrast three-dimensional CT imaging of the renal calyx and ureters
Discussion
Among the surgeries of the HK, transplantation of a HK is very rare but has important considerations given the difficulties related to its morphology. According to Stroosma et al. [9], between the years 1975 and 2000, 80 HKs were isolated and transplanted into 97 patients. Two procedures are used in the transplantation of a HK: en bloc transplantation and split transplantation. The decision to transplant a HK en bloc depends on several factors, including donor age, renal isthmus morphology, and vascular anatomy. If the collecting system crosses the midline, or if it does not cross the midline and the isthmus has a high-risk vascular system, en bloc transplantation is performed. If the collecting system does not cross the midline and the isthmus has a low-risk vascular system, then split transplantation is used.
Satyapal et al. reported that SRAs are seen in approximately 28 % of normal kidneys [7]. Thus, the presence of the first and second SRAs in our HK may not have been specific findings, whereas the SRA entering the isthmus was characteristic and is seen only in HKs. Natsis et al. described that a classification system with six basic patterns of arterial supply for each HK segment had been proposed by Graves. According to Graves’ classification, present case was type 1f (24 %) in which isthmus may be supplied by arterial branch from common iliac artery. These observations highlight the importance of determining the arterial distribution to the isthmus. For a patient with a HK who is undergoing surgery, the injection of methylene blue into the SRA entering the isthmus has been suggested to define the extent of the parenchymal blood supply by this vessel [8]. The analysis of our HK specimen was based on the same considerations as in HK transplantation. In addition, using contrast-enhanced micro-CT imaging together with the transparency procedure we were able to visualize the HK vasculature, including the SRAs, in detail. The imaging findings together with macroscopic observations of the SRAs with contrast dye revealed that the third SRA entered the inferior part of the isthmus and supplied only the isthmus. In addition, ureterography showed that the collecting system did not cross the midline in the present case. So this HK could have been transplanted by splitting with trimming away the reddened isthmus.
Although collecting systems may not be present in the HK isthmus, either gross-anatomically or radiologically, it may still contain many histologically proven nephrons, as seen in this specimen. Thus, the presence of an artery supplying the isthmus may indicate the presence of a nephron and functional urine production within the isthmus, because the supplying SRA can branch to form afferent arteries and then glomerular capillaries. Failure to recognize this anatomical arrangement can result in urinary leakage after splitting the isthmus.
In clinical reports of surgical procedures involving a HK, the venous system, including the IVC and renal veins, are often hardly mentioned. However, according to Sato et al. the incidence of IVC anomalies in HKs is higher than in normal kidneys [6]. In our specimen, there were no major anomalies of the venous system, although there were two SRVs, with the second one arising from the isthmus and connecting with the left common iliac vein, which could pose a risk during transplantation. In transplantation or other surgeries of HKs, the relationship among the renal arteries, veins, and ureters must be carefully noted because they may not be the same as those of a normal kidney. Despite the many detailed reports of the vessel patterns in dissected HKs, we recommend that anatomical, radiographic, and histological investigations of each HK will be of clinical benefit.
Conclusion
An anatomical and radiographic study of a dissected HK showed the typical U shape of the kidney, and the presence of three SRAs, two SRVs, and two ureters. Contrast imaging revealed that the third SRA entered the inferior part of the isthmus and supplied the entire isthmus. The urinary collecting system did not cross the midline of the isthmus. Our anatomical, radiographic, and histological approach can contribute to an improved surgical technique in the transplantation and biopsy of HKs.
References
Farman F (1968) Handbuch der Urologie: fusion anomalies of the kidney. Springer, New York, pp 66–72
Foster JT, Morrissey PE (2013) Segmental renal ischemia following transplantation of horseshoe kidney as separate allografts. Case Rep Transplant 2013:852127-1–852127-3. doi:10.1155/2013/852127
Iwanaga J, Saga T, Tabira Y, Tanaka S, Watanabe K, Yamaki K (2014) A case of horseshoe kidney with surplus renal arteries found in a student course of gross anatomy dissection. Kurume Igakukai Zasshi 77:57–62 (in Japanese)
Narita H, Tani T, Tonosaki Y (2012) Associations between kidney position and surplus renal arteries in horseshoe kidney: case report and analysis. Okajimas Folia Anat Jpn 89:7–13
Natsis K, Piagkou M, Skotsimara A, Prorogerou V, Tsitouridis I, Akandalakis P (2014) Horseshoe kidney: a review of anatomy and pathology. Surg Radiol Anat 36:517–526
Sato A (2011) Venous anomalies and horseshoe kidney. A minefield in open vascular surgery. Circ J 75:2759–2760
Satyapal KS, Haffejee AA, Singh B, Ramsaroop L, Robbs JV, Kalideen JM (2001) Additional renal arteries incidence and morphometry. Surg Radiol Anat 23:33–38
Sieńko J, Kotowski MJ, Nowacki A, Romanowski M, Sulikowski T, Ostrowski M (2013) Methylene blue usage in horseshoe kidney graft separation: case report. Transplant Proc 46:2923–2926
Stroosma OB, Schurink GWH, Smits JMA, Kootstra G (2001) Transplanting horseshoe kidneys: a worldwide survey. J Urol 166:2039–2042
Acknowledgments
The authors wish to thank the individual who donated their body for the advancement of education and research.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iwanaga, J., Saga, T., Tabira, Y. et al. Contrast imaging study of the horseshoe kidney for transplantation. Surg Radiol Anat 37, 1267–1271 (2015). https://doi.org/10.1007/s00276-015-1501-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-015-1501-0