Abstract
Purpose
This retrospective study evaluated the efficacy, safety, and factors affecting the prognosis of transarterial chemoembolisation with irinotecan-eluting beads with CalliSpheres (DEB-TACE) for intrahepatic cholangiocarcinoma (ICC).
Materials and Methods
We retrospectively collected data on 39 patients with unresectable ICC who received DEB-TACE therapy. We assessed the indicators of tumour response, progression-free survival (PFS), overall survival (OS), and the incidence of adverse events. PFS and OS were analysed using Kaplan–Meier curves, while Cox analysis was used to identify factors affecting the prognosis.
Results
The 3-month objective response rate (ORR) and disease control rate (DCR) of the 39 patients with unresectable ICC were 35.9% and 56.4%, respectively, while the 6-month ORR and DCR were 23.0% and 40.9%, respectively. The median OS and PFS were 11.0 months and 8.0 months, respectively. Cox analysis demonstrated that combined therapy (adjuvant sorafenib after DEB-TACE) and a low cancer antigen (CA) 125 level (≤ 35 U/ml) were independent favourable prognostic factors. Transient elevation of the aminotransferase level, nausea, vomiting, abdominal pain, fever, and hyper-bilirubinaemia were common adverse events in patients with unresectable ICC treated with DEB-TACE with CalliSphere beads (CBs). Hepatic abscess was the most serious complication, observed in one patient.
Conclusions
DEB-TACE with CBs is a safe and well-tolerated therapy in patients with unresectable ICC with a low incidence of adverse events and relatively prolonged survival. Combined therapy and low CA125 are prognostic factors associated with longer survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of intrahepatic cholangiocarcinoma (ICC), a malignant tumour arising from the small bile ducts, is increasing worldwide [1]. ICC accounts for approximately 15% of primary liver cancers and 3% of gastrointestinal malignancies [2, 3]. The rapid progression and high malignancy of ICC result in most patients being diagnosed at the late stage, with consequent low surgical resection rate, poor prognosis, and high mortality [4]. Factors such as tumour size, differentiation degree, presence of multiple tumours, lymph node metastasis, and portal-vein invasion have been associated with survival [5, 6]. The median overall survival (OS) of ICC ranges from 4.3 to 12 months, and long-term survival is rare [7, 8].
Liver resection is the radical therapy for ICC [9], but most patients are diagnosed with unresectable or metastatic disease. Even after resection, distant metastasis and recurrence are common, and the prognosis is poor [10, 11]. Therefore, additional locoregional and nonsurgical therapies are necessary to prolong the survival of patients with unresectable ICC. Transcatheter arterial chemoembolisation (TACE) is a widely received palliative therapy among patients with unresectable ICC and well-preserved liver function [12, 13]. Conventionally, lipiodol is used as the drug carrier in conventional TACE (C-TACE) therapy, but it has a high fluidity and poor sustained-release effect. Other embolisation materials, such as transarterial chemoembolisation with drug-eluting beads (DEB-TACE), could help overcome these issues [14].
CalliSphere beads (CBs, Jiangsu Hengrui Medicine Co., Ltd, Jiangsu, China), a novel type of drug-eluting beads, is the first drug-eluting beads product developed by China [15, 16]. Western countries, such as the USA and Italy, have confirmed the safety and efficacy of DEB-TACE [17, 18]. In a recent study, Zhou et al. used CalliSpheres loaded with epirubicin to treat unresectable ICC [19]. In another study Massimo et al. used irinotecan(100 mg)-eluting beads to treat advanced cholangiocarcinoma, but only five patients received DEB-TACE with irinotecan [17]. Irinotecan was predominately used in TACE to treat liver metastases of colorectal cancer [20]. Although it is expected that irinotecan could be a promising therapy for ICC [18], the clinical application of DEB-TACE with irinotecan in patients with ICC remains relatively limited in China.
The present study collected and analysed the data of 39 patients with unresectable ICC who underwent DEB-TACE with irinotecan therapy in Fifth Medical Centre of Chinese PLA General Hospital from April 2016 to October 2020, in an attempt to further elucidate its efficacy, safety, and factors affecting the prognosis.
Methods
Patients
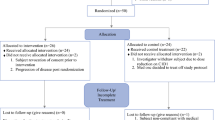
We collected the data of 39 patients with unresectable ICC who underwent DEB-TACE at the Fifth Medical Centre of Chinese PLA General Hospital between April 2016 and October 2020. The inclusion criteria were diagnosis of pathology-confirmed ICC, having received DEB-TACE therapy using CB, and availability of complete and accurate clinical data. Patients with other malignancies or those with incomplete clinical data were excluded. The study was approved by the appropriate ethics committee, and each patient and guardian provided informed consent.
Clinical Data Collection
We collected the baseline clinical data of patients from medical records, including age, sex, Eastern Cooperative Oncology Group (ECOG) performance status, tumour-node-metastasis staging, laboratory and pathologic examination results, magnetic resonance (MR) and computed tomography (CT) images, and therapy procedure.
DEB-TACE Procedure and Therapy
TACE was performed by an experienced interventional radiologist (> 5 years of experience). CBs (Jiangsu Hengrui Medicine Co., Ltd) with a diameter of 100–300 μm and 300–500 μm were used in this study. The CBs and irinotecan were mixed in a 20-mL syringe, and detailed information regarding the drug-eluting procedure is provided in the Supplemental Material (Supplemental Material).
A 5-F angiographic catheter (RF catheter; Terumo, Tokyo, Japan) was inserted into the celiac trunk and superior mesenteric artery to detect the arteries feeding the tumours with digital subtraction angiography (including cone-beam CT). The hepatic artery was then intubated using the Seldinger technique. A 2.6–2.8-Fr microcatheter (SP microcatheter; Terumo, Tokyo, Japan) was used to super select the tumour-feeding artery. The mixture of CB, irinotecan, and contrast agents was extracted using a syringe and injected into the superselected site through a microcatheter. Embolisation was discontinued when the flow rate of the contrast agent became slow or stagnant. Angiography of the superior mesenteric artery and celiac trunk was repeated, and the operation ended when the stain lesion disappeared.
TACE was repeated after 3 months if residual tumours or new lesions were confirmed on contrast-enhanced CT or MR imaging (MRI) or until it was no longer viable according to the following criteria: ECOG performance status > 2, international normalised ratio > 2.5, liver and kidney function damage, and life expectancy < 3 months.
Targeted Therapy
Adjuvant sorafenib (Bayer Pharma, Leverkusen, Germany) was administered after DEB-TACE according to the patient’s wishes when liver function returned to normal. All patients received standard doses of sorafenib (400 mg once a day, orally). Treatment interruptions and dose reductions (200 mg once a day, orally) were allowed if drug-related AEs occurred; treatment interruption was indicated if any grade-3 AEs occurred. Moreover, symptomatic treatment was provided to patients who experienced drug-related AEs.
Follow-up Assessments
At baseline, all patients underwent physical examination, medical history evaluation, assessment of the ECOG performance status, and routine laboratory tests. Contrast-enhanced CT (Siemens Sensation Cardiac; Siemens Medical Solutions, Erlangen, Germany) and MRI (Magneton Aera; Siemens Medical Solutions, Erlangen, Germany) were used to assess the tumours. The extent of disease was assessed using the aforementioned imaging modalities. The mRECIST was used to assess the tumour response, including complete response (CR), partial response (PR), stable disease (SD), and progressive disease [21]. Localized tumour response was defined as the progression/response at the embolized region. The CIRSE classification system was used to assess all AEs [22]. The objective response rate (ORR) was defined based on the assessment of CR and PR, and the disease control rate (DCR) was defined based on the assessment of CR, PR, and SD. Telephone interviews were used to follow up with all patients. The final follow-up data were obtained on April 14, 2021. OS was defined as the time from the start of DEB-TACE therapy to the date of death from any cause. PFS was defined as the time from the start of therapy to either liver-tumour progression or progression of lymph-node metastases or distant metastasis. Lymph-node metastasis was considered for tumours with a minimum diameter greater than 15 mm as measured on contrast-enhanced CT or MRI.
Statistical Analyses
SPSS version 26.0 (International Business Machines Corp., Armonk, NY, USA) and GraphPad Prism version 8.0 (GraphPad, San Diego, CA, USA) were used for the statistical analyses. Data are presented as counts (%). Differences in liver function indexes at each visit were compared with the McNemar test. Survival curves were generated using the Kaplan–Meier method, and data were compared using the log-rank test with two-sided P-values. Prognostic factors of OS were determined with univariate and multivariate Cox analyses. P < 0.05 was considered statistically significant.
Results
Patient Baseline Data
A total of 39 patients with unresectable ICC were included in the study; 26 patients had ECOG performance status 1 (66.7%). Twenty-five patients had hepatitis B infection (64.1%), while 17 (43.6%) and 21 (53.8%) patients received subsequent and combined therapy, respectively. The baseline characteristics of the patients are presented in Table 1.
Tumour Response
A total of 39 patients underwent DEB-TACE, with 22 patients (56.4%) undergoing only one session; the remaining patients received two or three sessions of DEB-TACE. Twenty-one patients (53.8%) received DEB-TACE combined with other therapies, such as molecular targeted therapy and immunotherapy. After DEB-TACE therapy, the 3-month and 6-month ORR and DCR in the 39 study patients were assessed by experienced radiologists using the mRECIST (Table 2). The localised ORR and DCR at 3 months were 35.9% and 56.4% and at 6 months were 25.6% and 43.5%, respectively. The 3-month ORR and DCR were 35.9% and 56.4%, respectively. CR, PR, and SD were observed in 3 (7.7%), 11 (28.2%), and 8 (20.5%) of the 39 patients, respectively. At 6 months, the ORR was 23.0% and the DCR was 40.9%; CR, PR, and SD were observed in 1 (2.5%), 8 (20.5%), and 7 (17.9%) patients, respectively. (Fig. 1a–d).
a, b Preoperative MRI in the arterial period and delay period shows a mass lesions in the right lobe of the liver and lymph node metastasis (white arrow); c, d Abdominal MRI reexamination 3 months after treatment revealed complete necrosis of the lesion and shrunken lymph node (white arrow) in the arterial period and delay period
Survival and Disease Progression
The OS and PFS of the patients with unresectable ICC who underwent DEB-TACE therapy were estimated with Kaplan–Meier curves, which showed that the median OS and PFS were 11 months (95% confidence interval [CI]: 8.2–13.7) and 8.0 months (95% CI: 4.8–11.1), respectively (Fig. 2a and b).
Factors Influencing OS in Patients with Unresectable ICC
Cox analysis was used to assess the data of the 39 patients with unresectable ICC treated with DEB-TACE (Table 3). Univariate analysis showed that combined therapy (hazard ratio [HR] = 5.124, P = 0.001) was correlated with longer OS, whereas the cancer antigen (CA) 125 level (HR = 0.302, P = 0.009) was associated with shorter OS in patients with unresectable ICC. Multivariate analysis showed that combined therapy (HR = 9.212, P = 0.001) independently indicated longer OS, whereas the CA125 level (HR = 0.273, P = 0.010) independently indicated shorter OS in patients with unresectable ICC. The difference in OS across patients with different characteristics was evaluated with further subgroup analysis (Fig. 3). The results showed that a CA125 level ≤ 35 U/mL (P = 0.027) (Fig. 3a) and combined therapy (P = 0.004) (Fig. 3b) were correlated with better OS. The median OS of the CA125 level ≤ 35 U/mL subgroup was 13.0 months and that of the CA125 level > 35 U/mL subgroup was 8.0 months; and 20.0 months in the subgroup that received combined therapy and 8.0 months in subgroup that did not receive combined therapy. However, sex (P = 0.098) (Fig. 3c) and tumour number (P = 0.061) (Fig. 3d) was not associated with OS.
Comparison of overall survival (OS) in the subgroup analysis. Independent predictive factors of OS were selected in the subgroup analysis to further evaluate their influence on survival. a Hazard ratio = 0.193 (95% confidence interval (CI): 0.065–0.569) in the CA125 level subgroup; b Hazard ratio = 3.779 (95% CI: 1.495–9.556) in the combined treatment subgroup; c Hazard ratio = 0.487 (95% CI: 0.211–1.124) in the sex subgroup; d Hazard ratio = 0.446 (95% CI: 0.192–1.037) in the tumour number subgroup. The Kaplan–Meier curves show the OS
Liver Function Changes After Therapy
Compared with the preoperative levels, the total bilirubin, alanine aminotransferase, and aspartate aminotransferase levels were higher 1 week after the DEB-TACE therapy (all P < 0.05). The values had returned to normal 1 month after DEB-TACE (all P < 0.05) in most patients (Table 4).
Safety Analysis
All 39 patients were evaluated for treatment safety. The most frequently reported TACE-related AEs were aminotransferase elevation (33 patients, 84.6%), hyper-bilirubinaemia (18 patients, 46.2%), abdominal pain (14 patients, 35.9%), and fever (12 patients, 30.8%). One patient developed a hepatic abscess after DEB-TACE therapy, which resolved shortly after percutaneous drainage (Table 5).
Discussion
ICC is a hepatobiliary neoplasm with poor prognosis, and only few patients with ICC undergo surgical resection [6]. Consequently, exploring reasonable and effective therapy solutions for patients with unresectable ICC has long been a worldwide challenge. TACE, as a palliative approach, is a promising locoregional therapy. Consequently, TACE has been considered a safe, effective, and feasible therapy for patients with unresectable ICC [23]. Compared with conventional TACE, DEB-TACE can be combined with drug-eluting beads and drugs with releasing properties and involves increased selective tumour targeting [24, 25]. In this preliminary study, we selected CBs with diameters of 100–300 μm and 300–500 μm because the bead size may alter the embolisation effect. Increasing evidence has shown that intratumoral vessels are usually smaller than 300 μm [26,27,28]. In addition, CBs have been developed as a new drug-eluting bead type in China. CBs, with some negatively charged groups, can be combined with chemotherapeutic drugs, such as irinotecan with a positive charge, by ion exchange [29]. Studies have demonstrated that approximately 80% of chemotherapeutic drugs can be mixed with 100–300 μm and 300–500 μm CBs within 30 min [14]. DEB-TACE with CBs is considered a reasonable and effective therapy for unresectable hepatobiliary neoplasm according to recent clinical studies [16, 19].
The ORR of patients with unresectable ICC treated with DEB-TACE in this preliminary study was lower than that in previously reported studies [19, 30]. This could be attributed to several reasons. First, the patients with unresectable ICC in this preliminary study had a poor prognosis, as the disease was diagnosed at an advanced stage. Second, this was a retrospective study, and the sample size was limited. Another phase II trial comprising patients with unresectable ICC reported an ORR of 39.3% [31]. The median OS and PFS in this study were longer than those in previous studies, but there was no significant difference [19, 32]. Similarly, a meta-analysis by Mosconi et al. showed that the ORR and median OS were 19.3% and 13.5 months, respectively, in patients with unresectable ICC who received radio-embolisation. The efficacy was not significantly different between radio-embolisation and DEB-TACE [33]. Multivariate regression analysis showed that combined therapy and the CA125 level were associated with OS in patients with unresectable ICC. Further subgroup analysis showed that a CA125 level ≤ 35 U/mL and combined therapy were related to a longer OS. Previous studies have also demonstrated that combined therapy and the CA125 level were factors influencing the prognosis [19, 32]; however, prognostic factors, such as tumour burden and lymph-node metastasis, were not statistically significant in this study, which may be related to the study sample size [34, 35]. The median survival of up to 20 months highlighted the advantage of combination therapy in patients with unresectable ICC, including combined immunotherapy or molecular targeted therapy. Therefore, a multidisciplinary approach to therapy is necessary. The CA125 level as a prognostic factor for patients with unresectable ICC requires confirmation by further prospective studies.
Regarding the safety of DEB-TACE, we observed no therapy-related deaths, and only one patient with unresectable ICC developed a hepatic abscess after DEB-TACE therapy. Hepatic abscesses are a serious and rare AE after DEB-TACE therapy [24], and the main causes involve the Child–Pugh class, damaged biliary mucosa, tumour burden, and particulate embolisation among others [36]. The baseline data of all patients and treatments were similar, but only this one patient initially underwent liver resection to remove a liver tumour, but the tumour relapsed, and the patient received DEB-TACE to treat unresectable ICC. Consequently, we assume that liver resection could lead to damage to the bile duct, and DEB-TACE treatment was performed after tumour recurrence, which could have eventually led to the occurrence of the hepatic abscess. In a previous study, the most commonly observed AEs after DEB-TACE were fever, abdominal pain, hyper-bilirubinaemia, and increased transaminase levels, and the types of AEs were similar to those of radio-embolisation [24, 33, 37,38,39]. The incidence of AEs is relatively low, and no serious AEs tend to occur [40]. Similarly, in the present study, most therapy-related AEs were of grades 1 and 2. Common AEs included nausea, vomiting, abdominal pain, fever, and fatigue. Although 84.6% and 46.2% of patients respectively had elevated transaminase and TBIL levels, the values had returned to normal 1 month after DEB-TACE in most cases. Consistent with this evidence, DEB-TACE in patients with unresectable ICC was relatively safe, and the side effects were manageable.
Our study also has many limitations. First, the sample size was relatively limited because the incidence of ICC is low. Second, there was no significant improvement in ORR, DCR, or OS in this study compared to previous studies, possibly because most patients had unresectable ICC. Although there is increasing progress in therapies for ICC, safe and effective therapies for unresectable ICC are lacking [41,42,43,44]. Third, although experienced radiologists assessed the imaging data, it was difficult to utilise the mRECIST to evaluate the safety and efficacy of DEB-TACE in ICC because of irregular necrosis. Finally, our study did not include an experimental control group. We are intending to recruit patients in a prospective study, and more compelling data will be further exhibited.
In summary, for patients with unresectable ICC, this study showed that DEB-TACE could be a reasonable and effective therapy, with a low complication rate and relatively prolonged survival. Combined therapy, including molecular targeted therapy and immunotherapy, is an independent prognostic factor for longer survival, while a high CA125 level is a poor prognostic factor for survival. Although DEB-TACE is a useful locoregional therapy, this preliminary study showed that combining targeted therapy, immunotherapy, and locoregional therapy is favourable for patients with unresectable ICC. More rigorous prospective studies are required in the future to confirm the value of comprehensive therapy in patients with unresectable ICC.
Abbreviations
- AEs:
-
Adverse events
- CB:
-
CalliSphere bead
- CI:
-
Confidence interval
- CR:
-
Complete response
- CT:
-
Computed tomography
- C-TACE:
-
Conventional TACE
- DCR:
-
Disease control rate
- DEB-TACE:
-
Drug-eluting bead TACE
- ECOG:
-
Eastern cooperative oncology group
- HR:
-
Hazard ratio
- ICC:
-
Intrahepatic cholangiocarcinoma
- MRI:
-
Magnetic resonance imaging
- mRECIST:
-
Modified response evaluation criteria in solid tumors
- ORR:
-
Objective response rate
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- PR:
-
Partial response
- SD:
-
Stable disease
References
Razumilava N, Gores GJ. Cholangiocarcinoma. Lancet. 2014;383(9935):2168–79.
Gupta A, Dixon E. Epidemiology and risk factors: intrahepatic cholangiocarcinoma. Hepatobiliary Surg Nutr. 2017;6(2):101–4.
Banales JM, Marin JJG, Lamarca A, et al. Cholangiocarcinoma 2020: the next horizon in mechanisms and management. Nat Rev Gastroenterol Hepatol. 2020;17(9):557–88.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Choi S-B, Kim K-S, Choi J-Y, et al. The prognosis and survival outcome of intrahepatic cholangiocarcinoma following surgical resection: association of lymph node metastasis and lymph node dissection with survival. Ann Surg Oncol. 2009;16(11):3048–56.
Aljiffry M, Walsh MJ, Molinari M. Advances in diagnosis, treatment and palliation of cholangiocarcinoma: 1990–2009. World J Gastroenterol. 2009;15(34):4240–62.
Kim RD, McDonough S, El-Khoueiry AB, et al. Randomised phase II trial (SWOG S1310) of single agent MEK inhibitor trametinib Versus 5-fluorouracil or capecitabine in refractory advanced biliary cancer. Eur J Cancer. 2020;130:219–27.
Markussen A, Jensen LH, Diness LV, Larsen FO. Treatment of patients with advanced biliary tract cancer with either oxaliplatin, gemcitabine, and capecitabine or cisplatin and gemcitabine-a randomized phase II trial. Cancers. 2020; 12(7)
Mazzaferro V, Gorgen A, Roayaie S, Droz Dit Busset M, Sapisochin G. Liver resection and transplantation for intrahepatic cholangiocarcinoma. J Hepatol. 2020;72(2):364–77.
Hu L-S, Zhang X-F, Weiss M, et al. Recurrence patterns and timing courses following curative-intent resection for intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2019;26(8):2549–57.
Wang M-L, Ke Z-Y, Yin S, Liu C-H, Huang Q. The effect of adjuvant chemotherapy in resectable cholangiocarcinoma: a meta-analysis and systematic review. Hepatobiliary Pancreat Dis Int. 2019;18(2):110–6.
Tan E, Cao B, Kim J, et al. Phase 2 study of copanlisib in combination with gemcitabine and cisplatin in advanced biliary tract cancers. Cancer. 2021;127(8):1293–300.
Chiang N, Chen M, Yang S, et al. Multicentre, phase II study of gemcitabine and S-1 in patients with advanced biliary tract cancer: TG1308 study. Liver Int. 2020;40(10):2535–43.
Chen Q, Sun Y, Dai H, Guo P, Hou S, Sha X. Assessment of irinotecan loading and releasing profiles of a novel drug-eluting microsphere (CalliSpheres). Cancer Biother Radiopharm. 2020;
Liu S, Yu G, Wang Q, et al. CalliSpheres microspheres drug-eluting bead transhepatic artery chemoembolization with or without sorafenib for the treatment of large liver cancer: a multi-center retrospective study. Am J Transl Res. 2021;13(12):13931–40.
Zhang X, Zhou J, Zhu DD, et al. CalliSpheres® drug-eluting beads (DEB) transarterial chemoembolization (TACE) is equally efficient and safe in liver cancer patients with different times of previous conventional TACE treatments: a result from CTILC study. Clin Transl Oncol. 2019;21(2):167–77.
Venturini M, Sallemi C, Agostini G, et al. Chemoembolization with drug eluting beads preloaded with irinotecan (DEBIRI) vs doxorubicin (DEBDOX) as a second line treatment for liver metastases from cholangiocarcinoma: a preliminary study. Br J Radiol. 2016;89(1067):20160247.
Martin RCG, Howard J, Tomalty D, et al. Toxicity of irinotecan-eluting beads in the treatment of hepatic malignancies: results of a multi-institutional registry. Cardiovasc Intervent Radiol. 2010;33(5):960–6.
Zhou T-Y, Zhou G-H, Zhang Y-L, et al. Drug-eluting beads transarterial chemoembolization with CalliSpheres microspheres for treatment of unresectable intrahepatic cholangiocarcinoma. J Cancer. 2020;11(15):4534–41.
Pereira PL, Iezzi R, Manfredi R, et al. The CIREL cohort: a prospective controlled registry studying the real-life use of irinotecan-loaded chemoembolisation in colorectal cancer liver metastases: interim analysis. Cardiovasc Intervent Radiol. 2021;44(1):50–62.
Lencioni R. New data supporting modified RECIST (mRECIST) for hepatocellular Carcinoma. Clin Cancer Res. 2013;19(6):1312–4.
Filippiadis DK, Binkert C, Pellerin O, Hoffmann RT, Krajina A, Pereira PL. Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Intervent Radiol. 2017;40(8):1141–6.
Savic LJ, Chapiro J, Geschwind J-FH. Intra-arterial embolotherapy for intrahepatic cholangiocarcinoma: update and future prospects. Hepatobiliary Surg Nutr. 2017; 6(1)
Kuhlmann JB, Euringer W, Spangenberg HC, et al. Treatment of unresectable cholangiocarcinoma: conventional transarterial chemoembolization compared with drug eluting bead-transarterial chemoembolization and systemic chemotherapy. Eur J Gastroenterol Hepatol. 2012;24(4):437–43.
Peng Z, Cao G, Hou Q, et al. The comprehensive analysis of efficacy and safety of callispheres drug-eluting beads transarterial chemoembolization in 367 liver cancer patients: a multiple-center. Cohort Study Oncol Res. 2020;28(3):249–71.
Laurent A, Wassef M, Chapot R, et al. Partition of calibrated tris-acryl gelatin microspheres in the arterial vasculature of embolized nasopharyngeal angiofibromas and paragangliomas. J Vasc Interv Radiol. 2005;16(4):507–13.
Lee K-H, Liapi E, Ventura VP, et al. Evaluation of different calibrated spherical polyvinyl alcohol microspheres in transcatheter arterial chemoembolization: VX2 tumor model in rabbit liver. J Vasc Interv Radiol. 2008;19(7):1065–9.
Lee K-H, Liapi E, Vossen JA, et al. Distribution of iron oxide-containing embosphere particles after transcatheter arterial embolization in an animal model of liver cancer: evaluation with MR imaging and implication for therapy. J Vasc Interv Radiol. 2008;19(10):1490–6.
Zhang S, Huang C, Li Z, et al. Comparison of pharmacokinetics and drug release in tissues after transarterial chemoembolization with doxorubicin using diverse lipiodol emulsions and CalliSpheres Beads in rabbit livers. Drug Deliv. 2017;24(1):1011–7.
Marquardt S, Kirstein MM, Brüning R, et al. Percutaneous hepatic perfusion (chemosaturation) with melphalan in patients with intrahepatic cholangiocarcinoma: european multicentre study on safety, short-term effects and survival. Eur Radiol. 2019;29(4):1882–92.
Sohal D, Mykulowycz K, Uehara T, et al. A phase II trial of gemcitabine, irinotecan and panitumumab in advanced cholangiocarcinoma. Ann Oncol. 2013;24(12):3061–5.
Higashi M, Yamada N, Yokoyama S, et al. Pathobiological implications of MUC16/CA125 expression in intrahepatic cholangiocarcinoma-mass forming type. Pathobiology. 2012;79(2):101–6.
Mosconi C, Solaini L, Vara G, et al. Transarterial chemoembolization and radioembolization for unresectable intrahepatic cholangiocarcinoma-a systemic review and meta-analysis. Cardiovasc Intervent Radiol. 2021;44(5):728–38.
Bagante F, Spolverato G, Merath K, et al. Intrahepatic cholangiocarcinoma tumor burden: a classification and regression tree model to define prognostic groups after resection. Surgery. 2019;166(6):983–90.
Asaoka T, Kobayashi S, Hanaki T, et al. Clinical significance of preoperative CA19-9 and lymph node metastasis in intrahepatic cholangiocarcinoma. Surg Today. 2020;50(10):1176–86.
Woo S, Chung JW, Hur S, et al. Liver abscess after transarterial chemoembolization in patients with bilioenteric anastomosis: frequency and risk factors. AJR Am J Roentgenol. 2013;200(6):1370–7.
Schicho A, Pereira PL, Pützler M, et al. Degradable starch microspheres transcatheter arterial chemoembolization (DSM-TACE) in intrahepatic cholangiocellular carcinoma (ICC): results from a national multi-center study on safety and efficacy. Med Sci Monit. 2017;23:796–800.
Carter S, Martin Ii RCG. Drug-eluting bead therapy in primary and metastatic disease of the liver. HPB. 2009;11(7):541–50.
Aliberti C, Benea G, Tilli M, Fiorentini G. Chemoembolization (TACE) of unresectable intrahepatic cholangiocarcinoma with slow-release doxorubicin-eluting beads: preliminary results. Cardiovasc Intervent Radiol. 2008;31(5):883–8.
Poggi G, Quaretti P, Minoia C, et al. Transhepatic arterial chemoembolization with oxaliplatin-eluting microspheres (OEM-TACE) for unresectable hepatic tumors. Anticancer Res. 2008;28:3835–42.
Tsilimigras DI, Sahara K, Wu L, et al. Very early recurrence after liver resection for intrahepatic cholangiocarcinoma: considering alternative treatment approaches. JAMA Surg. 2020;155(9):823–31.
Goyal L, Sirard C, Schrag M, et al. Phase I and biomarker study of the Wnt pathway modulator DKN-01 in combination with gemcitabine/cisplatin in advanced biliary tract cancer. Clin Cancer Res. 2020;26(23):6158–67.
Colyn L, Bárcena-Varela M, Álvarez-Sola G, et al. Dual targeting of G9a and DNMT1 for the treatment of experimental cholangiocarcinoma. Hepatology. 2020;
Meadows V, Francis H. Doublecortin-like kinase protein 1 in cholangiocarcinoma: is this the biomarker and target we have been looking for? Hepatology. 2021;73(1):4–6.
Funding
This work was supported by grants from the Research Fund for Interventional Oncology of Beijing Medical Award Foundation (No. XM2018_011_0006_01) and Capital's Funds for Health Improvement and Research (NO. Z181100001718075).
Author information
Authors and Affiliations
Contributions
XH: Conceptualization, substantial contributions to conception, formulation or evolution of overarching research goals and aims. LD, WJ: Methodology and Writing- original draft preparation, substantial contributions to Development of methodology and original draft preparation. MZ, ZN, ZY: Resources and Methodology, substantial contributions to samples collection, acquisition of data and analysis. YX, WZ: Investigation, substantial contributions to investigation process, specifically performing the experiments and data collection.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare.
Ethical Approval
The study was approved by the ethics committee, and each patient and guardian provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, D., Wang, J., Ma, Z. et al. Treatment of unresectable intrahepatic cholangiocarcinoma using transarterial chemoembolisation with irinotecan-eluting beads: analysis of efficacy and safety. Cardiovasc Intervent Radiol 45, 1092–1101 (2022). https://doi.org/10.1007/s00270-022-03108-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-022-03108-z