Abstract
Purpose
To evaluate the ability of neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), aspartate aminotransferase-to-lymphocyte ratio (ALRI) and systemic-inflammation index (SII) to predict clinical outcomes in hepatocellular carcinoma (HCC) patients undergoing transarterial radioembolization (TARE).
Materials and Methods
One hundred forty-five patients who underwent treatment of 167 HCCs had their pretreatment and 1 month post treatment laboratory values evaluated. Overall survival (OS), progression-free survival (PFS) and local PFS models were performed with patients separated by median inflammatory scores.
Results
The median pretreatment NLR, PLR, ALRI and SII were 3.0 (range: 0.5–176), 104.4 (range: 25–830), 55.7 (range: 7.5–2090) and 360.2 (range: 51.1–7207.8), respectively. While the median post treatment NLR, PLR, ALRI and SII were 6.2 (range: 0.4–176), 180 (range: 35–2100), 125 (range: 15.9–5710) and 596.8 (range: 28.9–19,320), respectively. OS models showed significant differences when separating the groups by median post treatment NLR (p = 0.003) and SII (p = 0.003). Multivariate Cox regression models for OS with all pre and post treatment inflammatory markers (log-scale) as well as tumor size, AFP and Child–Pugh score showed significant pretreatment NLR [HR: 0.22 (95% CI:0.06–0.75), p = 0.016] and SII [3.52 (95% CI: 1.01–12.3), p = 0.048], as well as post treatment NLR [6.54 (95% CI: 1.57–27.2), p = 0.010] and SII [0.20 (95% CI: 0.05–0.82), p = 0.025] association. The post treatment ALRI (p = 0.010) correlated with PFS while, post treatment NLR (p < 0.001), ALRI (p = 0.024) and SII (p = 0.005) correlated with local PFS.
Conclusion
Pretreatment and post treatment NLR and SII may be associated with OS and post treatment ALRI may be associated with both PFS and local PFS in HCC patients undergoing TARE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the third most common cause of cancer death worldwide [1] and transarterial radioembolization (TARE) has been shown to provide significant benefit to a wide spectrum of HCC patients [2,3,4]. However, there have also been significant advances in the treatment options for patients with HCC over the last several years [5]. This underlies the importance of identifying prognostic factors not only for patient education but also to select the best treatment strategy for each patient. Similarly, although TARE has been shown to be effective, judging its clinical result by imaging at 1 month is difficult [6]. Therefore, markers which may help to understand post treatment prognosis during early follow-up would be of benefit.
The tumor microenvironment and immune system have become increasingly recognized as integral components in cancer outcomes [5]. At the same time, systemic inflammation has been recognized as an indicator of poorer outcomes [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]. This has led to the investigation of neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) correlation with clinical outcomes in the setting of locoregional therapies and HCC. NLR was developed to evaluate two aspects of the immune system, namely inflammation (both acute and chronic) as indicated by the neutrophil count and adaptive immunity, by evaluation of the lymphocyte count [7]. PLR uses the same marker of adaptive immunity, lymphocyte count, but utilizes platelets, which are known to be rich in pro-inflammatory agents and have complex interactions with the tumor microenvironment, instead of neutrophils as a marker of inflammation [8]. While relatively robust data is available on the utility of NLR and PLR when HCC is treated with transarterial chemoembolization (TACE) [9,10,11] and liver resection [11,12,13], little data is available in the setting of TARE [14,15,16,17,18]. Furthermore, in the available studies discrepancies in NLRs ability to predict outcomes such as overall survival (OS) have emerged. For instances, pre and post treatment NLR values have been found to be significant in predictors of OS in some studies [14, 15] but not others [16].
Additionally, to the authors’ knowledge, no data is available on the ability of other systemic inflammatory scores, such as aspartate aminotransferase to lymphocyte ratio (ALRI) and systemic-inflammation index (SII) to predict outcomes in this patient population. SII incorporates both platelets and neutrophils, which have proven roles in inflammation and tumoral interaction as described above as well as lymphocytes (adaptive immunity) in its calculation [7, 8]. ALRI, again utilizes lymphocytes, an important factor in adaptive immunity but instead of platelets or neutrophils incorporates aspartate aminotransferase (AST). AST is an established marker of liver injury, which can occur in inflammation, and given HCC is a primary liver cancer this marker is of interest [19]. SII and ALRI have been shown to be of utility in HCC patients treated by other means such as surgical resection and TACE [12, 13, 20, 21], and thus their investigation in radioembolization is of merit.
Radioembolization provides a unique setting for these inflammatory scores that all incorporate the lymphocyte count into their calculation, due to the radiosensitivity of this cell population [22,23,24,25,26]. However, to date there is limited data for NLR and PLR in the setting of HCC treated with TARE and no data, to the authors knowledge, of the correlation between SII and ALRI and oncologic outcomes in this setting. Therefore, this study aims to fill this gap in knowledge by evaluating the potential association of both pretreatment and 1 month post treatment NLR, PLR, ALRI and SII and oncologic outcomes in patients with HCC treated by TARE.
Material and Methods
Patient Population
After obtaining institutional review board (IRB) approval all patients treated with TARE between 1/1/2014 and 12/31/2019 were reviewed. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained for each procedure, however, informed consent for this research project was waived by the IRB. Inclusion criteria included treatment for HCC and laboratory data allowing for calculation of at least one inflammatory score (NLR, PLR, ALRI or SII). Exclusion criteria included those patients who did not have technically successful TARE treatments, defined as complete coverage of the target perfused volume, were lost to follow-up prior to 3 months post treatment and those who requested to be omitted from retrospective research. In the case of post treatment inflammatory score calculations patients who did not have the necessary laboratory values drawn within 14–90 days post treatment were also excluded.
Outcomes
OS was considered the primary outcome and defined as the time between the initial treatment and time of death from any cause, the last clinical follow-up or time of transplant. Secondary outcomes included progression-free survival (PFS), local PFS, and radiologic response. PFS was defined as time from initial treatment to progression by European Association for the Study of the Liver (EASL) criteria or death. Local PFS was defined as time from initial treatment to local progression by EASL criteria or death. For the OS, PFS and local PFS patient data were censored at the time of last clinical follow-up or transplantation if the appropriate end point had not been reached. Radiologic response was evaluated utilizing the EASL criteria on 3 months post treatment imaging. An objective radiologic response (ORR) was considered to be a partial or complete response by EASL criteria.
Laboratory, Treatment and Demographic Data
The patients’ electronic medical records were reviewed and laboratory values including neutrophils, lymphocytes, international normalization ratio (INR), creatinine total bilirubin, albumin and alpha fetoprotein (AFP) were collected in the pre and post treatment period. These laboratory values were utilized to calculate the model for end stage liver disease (MELD) score and Child–Pugh score. Demographic data including sex, cause of cirrhosis and age were also collected. Finally, procedural details such as type of yttrum-90 utilized (resin or glass), perfused volume, activity delivered, tumoral absorbed dose and normal tissue absorbed dose were recorded as was the size of the largest treated HCC.
TARE Treatment and Follow-Up
All patients were reviewed at a multidisciplinary conference and considered for intra-arterial therapy if not felt to be candidates for curative intent ablation or surgical resection. Ultimately the choice of intra-arterial therapy (TARE or TACE) was left at the discretion of the treating Interventional Radiologist and evolved over the study period. However, in general patients with large (> 5 cm) HCCs and those with aggressive features (infiltrative HCC or portal vein invasion) tended to be treated with TARE. The TARE procedure has been described extensively before [2,3,4]. However, in brief patients underwent a mapping procedure utilizing technetium-99 m macroaggregated albumin (Tc 99 m MAA). Following Tc 99 m MAA delivery patients underwent a single photon emission computed tomography (SPECT) CT to determine distribution within the liver, lung shunt fraction, and if extrahepatic signal was present. The dose per patient was calculated at the performing Interventional Radiologist preference utilizing a variety of dosimetry techniques, including body surface area (BSA), MIRD, partition, and a multi-compartment method, during the study period. Similarly, the target absorbed dose varied over the study period. Patients returned within two weeks of mapping and the dose was delivered from the predetermined location. Following delivery patients underwent a post TARE bremsstrahlung SPECT CT. The use of resin (Sirtex Medical) or glass (Boston Scientific) yttrium 90 was based on user preference.
Patients were followed up at 1 and 3 months with both laboratory values and imaging. Patients were then followed every 3–6 months after that. Complications were recorded during follow-up, however, symptoms of post embolization syndrome, such as fatigue, mild pain (not requiring further treatment) and nausea were considered expected side effects and not complications. Complications were graded according to CIRSE guidelines [27].
Inflammatory Score Calculations
NLR, PLR and ALRI were calculated by dividing the neutrophil count, platelet count, and aspartate aminotransferase (AST) level by the lymphocyte count, respectively. Finally, SII was calculated by multiplying the neutrophil and platelet count and dividing that number by the lymphocyte count. Pretreatment inflammatory values were calculated based on laboratory data collected on the day of, but prior to, treatment. While post treatment values were collected at 30 day follow-up visits with the collection date occurring a mean of 41.9 ± 22.1 days following TARE treatment.
Statistical Analysis
Demographic and clinical measures were summarized descriptively. They were summarized either per subject or per TARE, as appropriate. Chi-square and two sample t-tests were used to compare groups for categorical and continuous measures, respectively. Due to skewness, comparisons were made by separating groups using median pre and post treatment NLR, PLR, ALRI and SII for all survival analyses.
The OS, PFS and local PFS curves were represented with the Kaplan–Meier method. Hazard ratios (HR), 95% confidence intervals and p-values were calculated using univariate Cox proportional-hazards regression models. For OS, only the data from the first observation per subject was used. All data were used for the PFS analyses, however a “cluster” term was included in each model to correct the standard errors using the grouped jackknife method that accounts for clustering due to multiple observations per subject. Additionally, multivariate Cox regression models were performed including all pre and post treatment inflammatory values, as well as log AFP, Child–Pugh score and tumor size (as continuous variables) for OS, PFS and local PFS. p-Values < 0.05 were considered statistically significant. R (Version 3.6.0) was used for all statistical analyses.
Results
In total 145 patients who underwent 167 TARE were included. There were 134 patients (92%) and 152 unique tumors (91%) with all pretreatment data available, and 126 patients (87%) and 148 unique tumors (89%) with all post treatment data available. Overall, there were 115 patients (79%) and 131 unique tumors (78%) with complete pre and post treatment data. The mean age was 63.8 ± 10.0 years and the population included 115 (80.3%) men and 30 (20.7%) women. The majority of patients received lobar deliveries (88/167, 52.7%), however only 3 patients (3/145, 2.1%) ultimately received bilobar treatment. Three patients (3/145, 2.1%) suffered complications which included celiac dissection (n = 1, CIRSE grade 1), radiation cholecystitis (n = 1, CIRSE grade 1) and gastrointestinal bleed (n = 1, CIRSE grade 3), respectively. Demographic data can be found in Table 1.
Table 2 reports the median and mean pre and post treatment NLR, PLR, ALRI and SII values. The median pretreatment NLR, PLR, ALRI and SII were 3.0 (range: 0.5, 176), 104.4 (range: 25, 830.0), 55.7 (range: 7.5, 2090) and 360.2 (range: 51.1, 7207.8), respectively. While the median post treatment NLR, PLR, ALRI and SII were 6.2 (range: 0.4, 176), 180 (range: 35, 2100), 125 (range: 15.9, 5710) and 596.8 (range: 28.9, 19,320), respectively.
Overall Survival
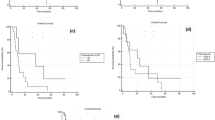
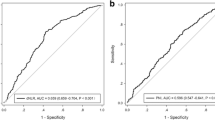
Figure 1 presents the Kaplan–Meier curves for overall survival (OS) when separating patients by the median pretreatment NLR, PLR, ALRI and SII. Neither pretreatment NLR (p = 0.800), PLR (p = 0.535), ALRI (p = 0.711) or SII (p = 0.960) were found to have significantly different survival curves. Figure 2 demonstrates the patients separated by median post treatment NLR, PLR, ALRI and SII. While below median post treatment NLR (p = 0.004) and SII (p = 0.004) patients were found to have longer OS, PLR (p = 0.844) and ALRI (p = 0.127) were not found to be significantly associated.
Table 3 shows the results of a multivariate Cox regression model which included all pre and post treatment inflammatory values as well as AFP, tumor size, and Child–Pugh score. On this analysis pretreatment NLR [0.22 (95% CI: 0.06–0.75), p = 0.016] and SII [3.52 (95% CI: 1.01–12.3), p = 0.048] were significantly associated with OS, as were post treatment NLR [6.54 (95% CI: 1.57–27.2), p = 0.010] and SII [0.20 (95% CI: 0.05–0.782, p = 0.025] for inflammatory markers.
Progression-Free Survival
Figure 3 presents the Kaplan–Meier curves for overall PFS when separating patients by the median pretreatment NLR, PLR, ALRI and SII. Neither pretreatment NLR (p = 0.876), PLR (p = 0.541), ALRI (p = 0.090) or SII (p = 0.632) were found to have significantly different PFS curves. Figure 4 demonstrates the patients separated by median post treatment NLR, PLR, ALRI and SII. While patients with below median post treatment ALRI (p = 0.010) were found to have significantly better PFS, neither NLR (p = 0.073), PLR (p = 0.373) or SII (p = 0.205) were found to be associated with PFS.
Table 4 shows the results of a multivariate Cox regression model which included all pre and post treatment inflammatory values as well as AFP, tumor size and Child–Pugh score. On this analysis no inflammatory markers remained significantly associated with PFS.
Local Progression-Free Survival
Figure 5 presents the Kaplan–Meier curves for local PFS when separating patients by the median pretreatment NLR, PLR, ALRI and SII. Neither pretreatment NLR (p = 0.551), PLR (p = 0.685), ALRI (p = 0.493) or SII (p = 0.784) were found to have significantly different local PFS curves. Figure 6 demonstrates the patients separated by median post treatment NLR, PLR, ALRI and SII. Patients with below median post treatment NLR (p < 0.001), SII (p = 0.005) and ALRI (p = 0.024) were found to have significantly longer local PFS. No statistically significant association between PLR (p = 0.183) and local PFS was found.
Table 5 shows the results of a multivariate Cox regression model which included all pre and post treatment inflammatory values as well as AFP, tumor size and Child–Pugh score. On this analysis no measure remained significantly associated with either local or overall PFS.
Objective Radiologic Response (ORR)
The correlation between NLR, PLR, ALRI, and SII and ORR can be found in Table 6. However, neither the pretreatment NLR, PLR, ALRI or SII had a significant association with the radiologic response when evaluated by all 4 EASL response categories or when divided into responders or non-responders. Of the post treatment values only those patients with above median SII after TARE had a greater likelihood of achieving an ORR (p = 0.044).
Discussion
This study evaluated the association of four inflammatory scores (NLR, PLR, ALRI and SII) both before and 1 month after treatment with meaningful clinical outcomes in HCC patients undergoing TARE. One surprising finding was that separating patients by median pretreatment NLR, PLR, ALRI and SII was not significantly associated with OS, PFS or local PFS on the univariate analysis. However, the multivariate Cox regression model which included all pre and post treatment inflammatory values as well as AFP, tumor size and Child–Pugh score showed a correlation between OS and pretreatment NLR [0.22 (95% CI: 0.06–0.75), p = 0.016] and SII [3.52 (95% CI: 1.01–12.3), p = 0.048]. These findings differ from Sukato et al. who found a relationship between pretreatment NLR and OS on Kaplan–Meier analysis but not multivariate analysis when using a cutoff of 5 [14]. The lack of relationship between pretreatment NLR and OS on Kaplan–Meier analysis is consistent with Li et al. who also failed to show a significant relationship when evaluating NLR as a continuous variable [16]. The significance of NLR in the multivariate analysis likely indicates a relationship between NLR and the other prognostic factors. Similar to NLR, pretreatment SII was not found to be associated with survival on Kaplan–Meier analysis but did demonstrate an association in the multivariate model. To the authors knowledge SII has not been studied in the setting of TARE for HCC. However, the multivariate model findings are consistent with the findings of Hu et al. and Yang et al. who found SII to be predictive of OS in the setting of HCC treated with surgical resection and TACE, respectively [13, 20].
The use of NLR as a prognostic indicator for outcomes in HCC patients treated by surgical resection and TACE has been fairly well documented [9,10,11,12,13]. Lymphocytes play a role in cytotoxic cell death and the production of anti-tumor cytokines [28], therefore, lymphopenia is associated with an impaired host immune response to the tumor and thus poor cancer-specific survival [29]. Similarly, neutrophilia also increases NLR values and has been associated with greater infiltration of tumor associated macrophages (TAMs) as well as elevated pro-inflammatory cytokines, which promote angiogenesis and tumor growth [30, 31]. The relative depletion of lymphocytes and/or neutrophilia likely explains NLRs predictive values. However, TARE itself has been shown to lead to a reduction of lymphocytes, which are a radiosensitive cell population [22,23,24,25,26]. While lymphocyte depletion has been typically thought of as a poor prognostic sign in solid cancers, one study demonstrated that relative lymphocyte depletion following TARE was associated with improved OS [22, 25]. This may imply that neutrophilia is of greater influence when evaluating the correlation between post treatment NLR and clinical outcomes.
Dividing patients by above and below median post treatment inflammatory markers resulted in significantly different Kaplan–Meier OS curves for NLR (p = 0.003) and SII (p = 0.003). In all cases those patients showing above median values demonstrated significantly worse OS. Conversely, the same was not demonstrated in regard to PLR (p = 0.844) and ALRI (p = 0.127). In the multivariate Cox regression model, post treatment NLR (p = 0.010) and SII (p = 0.025) remained significantly associated with OS. The NLR findings are similar to Estrade et al. who demonstrated that patients with a NLR of > 7.2 at 3 months post treatment had significantly worse OS [15]. These findings would suggest that NLR and SII may be best suited of the four inflammatory scores studied to predict OS in HCC patients undergoing TARE. Given both NLR and SII incorporate neutrophils in their calculation may provide further support for neutrophils playing an important role in this patient population.
Progression-free survival (and in particular local progression-free survival) are important markers in the setting of HCC treatments. While PFS is a correlate of OS, local PFS provides greater details on how the locoregional therapy worked, in its intent to treat the local disease. This is highlighted by previous studies which demonstrated that local control of HCC leads to improved OS as compared to best supportive care [32, 33]. Again, when evaluating PFS and local progression-free survival neither pretreatment NLR, PLR, ALRI or SII (p > 0.05 for all) were found to differ significantly when separated by the median. However, lower than median post treatment ALRI (p = 0.024) was associated with PFS and post treatment local progression-free survival was associated with post treatment NLR (p < 0.001), SII (p = 0.005) and ALRI (p = 0.024). When utilizing the multivariate Cox regression model, none of the inflammatory scores remained significant for either overall or local PFS. ALRI was the only marker found to be significantly associated with both local and overall PFS and is unique among the four studied inflammatory scores in that it involves a liver marker (AST). While the mechanism of ALRI relation to PFS and local PFS is not studied here one possible explanation is that the elevation in AST is a result of increased normal tissue dose which may in turn indicate less tumoral uptake.
The ability to accurately report treatment outcomes at 1 month by imaging is difficult when utilizing TARE to treat HCC [6]. Therefore, non-imaging markers are of interest. Neither NLR, PLR or ALRI were found to have predictive value in terms of radiologic responses in either the pretreatment or 1 month post treatment setting. However, having higher SII one month following treatment seemed to correlate with improved ORR. This was an unexpected finding and the explanation for this is not studied here. The reduction in lymphocytes, previously described following TARE, which has been associated with improved OS in some studies [25] does not seem to be a likely explanation given it should have influenced the other inflammatory markers as well. Therefore, it would be important for these findings to be confirmed prior to them being implemented into clinical decision making.
This study has a number of limitations including the fact that it is a retrospective single center review. Furthermore, the study was conducted at a quaternary referral center and some patients were lost to follow-up because of this. Similarly, there were a limited number of patients and this was compounded by the fact that not all variables were available for all patients. Finally, the center utilizes several different locoregional therapies for HCC and the subgroup selected for TARE may provide a selection bias.
In conclusion, both pretreatment and post treatment NLR and SII are significantly associated with OS on multivariate analysis, suggesting they may be best suited for OS predictions in HCC patients undergoing TARE. Furthermore, post treatment ALRI seems to correlate with PFS and local PFS and may be a helpful marker when counseling patients during the early post treatment stage.
References
Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends—an update. Cancer Epidemiol Prev Biomark. 2016;25(1):16–27.
Salem R, Gordon AC, Mouli S, et al. Y90 radioembolization significantly prolongs time to progression compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2016;151(6):1155–63.
Garin E, Tselikas L, Guiu B, et al. Personalised versus standard dosimetry approach of selective internal radiation therapy in patients with locally advanced hepatocellular carcinoma (DOSISPHERE-01): a randomized, muticentre, open-label phase 2 trial. Lancet Gastroenerol Hepatol. 2021;6(1):17–29.
Salem R, Johnson GE, Kim E, et al. Yttrium-90 radioembolization for the treatment of solitary, unresectable hepatocellular carcinoma: the LEGACY study. Hepatology. 2021. https://doi.org/10.1002/hep:31819. (epub ahead of print).
Finn RS, Qin S, Ikeda M, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382(20):1894–905.
Young S, Taylor A, Golzarian J, et al. Clinical utility of one month imaging following selective internal radiation therapy. Diagn Interv Imaging. 2019;100(1):39–46.
Faria SS, Fernandes PC, Silva MJB, et al. The neutrophil-tolymphocyte ratio: a narrative review. Ecancermedicalscience. 2016;10:702.
Lai Q, Vitale A, Manzia TM, et al. Platelets and hepatocellular cancer: bridging the bench to the clinics. Cancers. 2019;11(10):1568.
Li S, Feng X, Cao G, Wang Q, Wang L. Prognostic significance of inflammatory indices in hepatocellular carcinoma treated with transarterial cheomebolization: A Systematic review and meta-analysis. PLoS ONE. 2020;15(6):e0230879.
Wang C, Wang M, Zhang X, et al. The neutrophil-to-lymphocyte ratio is a predictive factor for the survival of patients with hepatocellular carcinoma undergoing transarterial chemoembolization. Ann Transl Med. 2020;8(8):541.
Sullivan K, Groeschl R, Turaga K, et al. Neutrophil-to-lymphocyte ratio as a predictor of outcomes for patients with hepatocellular carcinoma: a Western perspective. J Surg Oncol. 2014;109(2):95–7.
Jin J, Zhu P, Liao Y, Li J, Liao W, He S. Elevated preoperative aspartate aminotransferase to lymphocyte ratio index as an independent prognostic factor for patients with hepatocellular carcinoma after hepatic resection. Oncotarget. 2015;6:19217–27.
Hu B, Yang XR, Xu Y, et al. Systemic immune inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20:612–22.
Sukato DC, Tohme S, Chalhoub D, et al. The prognostic role of neutrophil-to-lymphocyte ratio in patients with unresectable hepatocellular carcinoma treated with radioembolization. J Vasc Interv Radiol. 2015;26(6):816–24.
Estrade F, Lescure C, Muzellec L, et al. Lymphocytes and neutrophil-to-lymphocyte ratio variations after selective internal radiation treatment of HCC: a retrospective cohort study. Cardiovasc Intervent Radiol. 2020;43(8):1175–81.
Li X, Montazeri SA, Paz-Fumagalli R, et al. prognostic significance of neutrophil to lymphocyte ratio dynamics in patients with hepatocellular carcinoma treated with radioembolization using glass microspheres. Eur J Nucl Med Mol Imaging. 2021. https://doi.org/10.1007/s00259-020-05186-7. (epub ahead of print)
Yoneoka G, Bozhilov K, Wong LL. Prognostic ability of inflammation-based markers in radioembolization for hepatocellular carcinoma. Hepatoma Res. 2020;6:67.
Taussig MD, Irene Koran ME, Mouli SK, et al. Neutrophil to lymphocyte ratio predicts disease progression following intra-arterial therapy of hepatocellular carcinoma. HPB (Oxford). 2017;19(5):458–64.
Yang Z, Zhang J, Lu Y, et al. Aspartate aminotransferase-lymphocyte ratio index and systeimic immune-inflammation index predict overall survival in HBV-related hepatocellular carcinoma patients after transcatheter arterial chemoembolization. Oncotarget. 2015;6(40):43090–8.
Yang Z, Zhang J, Lu Y, et al. Aspartate aminotransferase-lymphocyte ratio index and systemic immune-inflamation index predict overall survival in HBV-related hepatocellular carcinoma patients after transcatheter arterial chemoembolization. Oncotarget. 2015;6:43090–8.
Lu LH, Wei W, Li SH, Zhang YF, Guo RP. The lymphocyte-C-reactive protein ratio as the optimal inflammation-based score in patients with hepatocellular carcinoma underwent TACE. Aging. 2021;13(4):5358–68.
Venkatesulu BP, Mallick S, Lin SH, Krishnan S. A systemic review of the influence of radiation-induced lymphopenia on survival outcomes in solid tumors. Crit Rev Oncol Hematol. 2018;123:42–51.
Carr BI. Hepatic arterial 90Yttrium glass microspheres (Therasphere) for unresectable hepatocellular carcinoma: interim safety and survival data on 65 patients. Liver Transpl. 2004;10:S107-110.
Salem R, Lewandowski RJ, Atassi B, et al. Treatment of unresectable hepatocellular carcinoma with use of 90Y microspheres (TheraSphere): safety, tumor response, and survival. J Vasc Interv Radiol. 2005;16(12):1627–39.
Dunfee BL, Riaz A, Lewandowski RJ, et al. Yttrium-90 radioembolization for liver malignancies: prognostic factors associated with survival. J Vasc Interv Radiol. 2010;21(1):90–5.
Salem R, Johnosn GE, Kim E, et al. Yttrium-90 radioembolization for the treatment of solitary, unresectable hepatocellular carcinoma: the LEGACY study. Hepatology. 2021. https://doi.org/10.1002/hep.31819. epub ahead of print
Filippiadis DK, Binkert C, Pellerin O, Hoffman RT, Krajina A, Pereira PL. Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Intervent Radiol. 2017;40(8):1141–6.
Ding PR, An X, Zhang RX, et al. Elevated preoperative neutrophil to lymphocyte ratio predicts risk of recurrence following curative resection for stage IIA colon cancer. Int J Colorectal Dis. 2010;25(12):1427–33.
Ohtani H. Focus on TILS: prognostic significance of tumor infiltrating lymphocytes in human colorectal cancer. Cancer Immun. 2007;7:4.
Kuang DM, Zhao Q, Wu Y, et al. Peritumoral neutrophils link inflammatory response to disease progression by fostering angiogenesis in hepatocellular carcinoma. J Heaptol. 2011;54(5):948–55.
Mouchli M, Reddy S, Gerrard M, Boardman L, Rubio M. Usefulness of neutrophil-to-lymphocyte ratio (NLR) as a prognostic predictor after treatment of hepatocellular carcinoma. 2021. https://doi.org/10.1016/j.aohep.2020.08.067. Epub 2020 Sep 5
Llovet JM, Real MI, Montana X, et al. Arterial embolization or chemoembolization versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomized controlled trial. Lancet. 2002;359:1734–9.
Lo CM, Ngan H, Tso WK, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002;35:1164–71.
Acknowledgements
Research reported in this publication was supported by National Institute of Health grant P30 CA77598 utilizing the Biostatistics and Bioinformatics Core shared resource of the Masonic Cancer Center, University of Minnesota and by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number UL1-TR002494. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding
This study was not supported by any funding. SY is a consultant for Boston Scientific. JG and DD are consultants for Sirtex Medical.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shamar Young, Nathan Rubin, Donna D′Souza, Pranav Sharma, John Pontolillio, Siobhan Flanagan, Jafar Golzarian, Tina Sanghvi declare that they have no conflict of interest.
Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
For this type of study formal consent is not required. This study has obtained IRB approval from University of Minnesota IRB and the need for informed consent was waived. For this type of study consent for publication is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Young, S., Rubin, N., D’Souza, D. et al. Inflammatory Scores: Correlation with Clinical Outcomes in Hepatocellular Carcinoma Patients Undergoing Transarterial Radioembolization. Cardiovasc Intervent Radiol 45, 461–475 (2022). https://doi.org/10.1007/s00270-022-03080-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-022-03080-8