Abstract
Hepatic lymphorrhea is a leakage from the liver’s lymphatic ducts into the abdominal cavity and an extremely rare complication associated with injury of the hepatoduodenal ligament, which can lead to refractory ascites. Hepatic lymphorrhea is constituted by non-chylous ascites and can be visualized by transhepatic lymphangiography instead of pedal or intranodal lymphangiography. To date, only a few successfully treated cases using interventional procedures have been reported. Although n-butyl-2-cyanoacrylate (NBCA) glue is widely used in various cases of vascular embolization and other lymphatic leak treatments, there have been no reports of its use for post-surgical hepatic lymphorrhea. The NBCA glue embolization described in this case report may be one of the treatment options to control the refractory ascites derived from hepatic lymphorrhea.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatic lymphorrhea is a leakage from the hepatic lymphatic system into the abdominal cavity and an extremely rare complication that can cause refractory ascites [1,2,3,4,5]. Hepatic lymphorrhea is constituted by non-chylous ascites, which usually results from injury to the hepatoduodenal ligament in surgeries such as pancreaticoduodenectomy. This condition is different from chylous ascites resulting from an intestinal lymphatic injury. Furthermore, unlike lymphatic leakage due to injury to the aortoiliac lymphatic system after pelvic surgery, leakage points have not been visualized by pedal or intranodal lymphangiography [3,4,5,6]. Only a few reports on the successful treatment of this condition exist, using interventional procedures when conservative treatment failed [3,4,5]. However, to the best of our knowledge, there have been no reports on antegrade n-butyl-2-cyanoacrylate (NBCA) glue embolization for post-surgical hepatic lymphorrhea. We present a case of successful embolization using NBCA glue following hepatic lymphangiography with lipiodol via a puncture needle.
Case Report
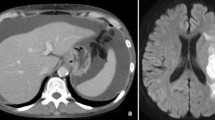
A 62-year-old male with mixed-type intraductal papillary mucinous neoplasm at the head of the pancreas was admitted to our hospital for surgery. He was an alcoholic with a history of lacunar infarction in the brain and hypertension. He was taking aspirin and antihypertensive drugs. Preoperative laboratory tests revealed moderate renal dysfunction (creatinine 1.4 mg/dL, estimated glomerular filtration rate [eGFR] 44 mL/min) and hepatic dysfunction [γ-glutamyl transpeptidase 643 U/L, alkaline phosphatase (ALP) 417 U/L]. A subtotal stomach-preserving pancreaticoduodenectomy with lymph node dissection was performed. The liver was found to have a hard and irregular surface intraoperatively, which was presumed to reflect chronic alcoholic hepatitis. The surgery was completed without any complications. All postoperative drains were removed by postoperative day (POD) 7, but abdominal distension due to ascites was observed. Although administration of diuretics and albumin preparations and ascites drainage were performed, they did not help improve the condition (Fig. 1). The ascites was not chylous, and its analysis revealed triglyceride levels < 110 mg/dL, high protein levels (4.2 g/dL), and increased lymphocytes (93.4%). Chronic hepatitis was confirmed during surgery, and it is well known that the hepatic lymphatic flow increases tenfold in a cirrhotic liver compared to a healthy one [4]. In addition, the surgical procedure did not extend around the aorta. Although no abnormal findings were observed in the hepatoduodenal ligament dissection during the operation, hepatic lymphorrhea was strongly suspected because of these factors. Administration of total parenteral nutrition and octreotide acetate was initiated. Although the amount of ascites drainage was also increased, prerenal failure worsened (the eGFR decreased to 17.9 mL/min at POD 42). These conservative therapies were unable to control the massive ascites. Unlike lumbar and paraaortic lymphatic leakage, the leakage point of hepatic lymphorrhea cannot be visualized by conventional intranodal lymphangiography [3,4,5,6]. Therefore, percutaneous transhepatic lymphangiography was chosen. On POD 49, 5800 mL of ascites was slowly drained during albumin administration. After local anesthesia and injection of hydroxyzine, the area around the anterior branch of the portal vein was punctured with a 21 G × 15 cm Chiba needle (Hanaco Medical Co., Ltd., Saitama, Japan) under ultrasound guidance (Fig. 2A), because the hepatic lymphatic system usually runs parallel to the portal venous system. A small amount of nonionic contrast was slowly injected under fluoroscopic guidance, and the lymphatic vessels were successfully visualized by the fifth puncture. After switching to lipiodol on slow administration, leakage was clearly visualized in the hepatic hilum (Fig. 2A). Approximately 4 mL of lipiodol was injected, which accumulated in the hepatic hilum to block the NBCA glue (Histoacryl; B. Braun Melsungen AG, Germany; NBCA mixed with lipiodol at a 1:7 ratio) entering the peritoneal cavity (Fig. 2C). Next, while monitoring the retraction of the needle, 2.5 mL of NBCA glue was slowly administered via a puncture needle flushed with 5% glucose solution (Fig. 2D). Embolization of the injured hepatic lymphatics around the hepatic hilum was achieved. Epigastric pain occurred during glue injection but improved after the procedure. A plain computed tomography was performed to confirm lipiodol accumulation in the hilum and lymphatic vessels of the liver (Fig. 3A). On the day after embolization, 900 mL of ascites was drained; however, the drainage decreased significantly thereafter, and the drain was removed on the 17th day. On the eighth day after embolization, the ongoing presence of lipiodol was confirmed in the hilum and lymphatic vessels of the liver on CT (Fig. 3B). The patient’s condition improved and he was discharged on POD 80 (31 days after embolization). Liver transaminase and ALP levels did not increase compared to their pre-embolization levels, and the eGFR improved to preoperative levels. No abdominal distension due to ascites was observed during the 5 months of follow-up.
(a) A 21 G × 15 cm Chiba needle is deeply advanced parallel to the anterior branch of the portal vein under ultrasound guidance (arrowhead: puncture needle; asterisk: anterior branch of the portal vein). B Transhepatic lymphangiography with a small amount of lipiodol shows the extravasation of contrast in the hepatic hilum (arrowheads: leakage of lipiodol). The flow of contrast into the abdominal cavity is also seen (small arrowheads). The intrahepatic bile ducts in the left hepatic lobe are visualized due to the incorrect administration of lipiodol during the second puncture (arrows). C A total of 4 mL of lipiodol is slowly administered to accumulate sufficient lipiodol at the hepatic hilum to block the leakage of the NBCA glue into the abdominal cavity as much as possible (asterisk). Lipiodol in the abdominal cavity, including the perihepatic cavity, also rose to the surface (two asterisks). D Subsequently, 12.5% NBCA glue is administered, and the distribution of cast formation in the hepatic lymphatic vessels is confirmed
A CT immediately after embolization shows the accumulation of lipiodol and NBCA glue from the hepatic hilum to the hepatic lymphatic vessels (circle). Lipiodol accumulation in the para-aortic lymph node is visualized (arrows). B CT 8 days after embolization shows the ongoing accumulation of glue around the hepatic hilum, and reveals a decrease of ascites (dagger). A median of 260 mL/day (range, 170–680 mL/day) of ascites was drained from days 2 to 10 after embolization. Afterward, 35 mL/day (range, 20–70 mL/day) of ascites was drained until tube removal. CT, computed tomography
Discussion
In most cases, conservative therapy, comprising total parenteral nutrition, octreotide acetate, diuretic, albumin, and plasma protein administration as well as ascites drainage, helps improve hepatic lymphorrhea. However, if this is not successful, treatment may be difficult. A diagnosis of hepatic lymphorrhea relies on the confirmation of the presence of ascites that is not chyle, low triglyceride levels (< 110 mg/mL), and visualization of leakage by percutaneous transhepatic lymphangiography [3,4,5,6]. Conventional intranodal lymphangiography was not used because of its inability to visualize hepatic lymphorrhea. Nadolski et al. [7] reported that the leakage point was not detected in 14 of 31 refractory chylous ascites by pedal or intranodal lymphangiography. There were 5 cases of pancreatic resection including pancreaticoduodenectomy, in which no leaks were visualized. In other words, it was presumed that these cases were hepatic lymphorrhea, and the leaks were not anatomically visualized by conventional lymphangiography. The therapeutic effect of lipiodol lymphangiography on various lymphatic leaks has also been reported [8, 9]. However, in this case, the therapeutic effect of lipiodol alone was considered low because of the visible leakage. Therefore, antegrade embolization was attempted using NBCA glue to adequately cover the injured site. The glue could be injected stably without retracting the needle. When puncturing around the portal vein, which is considered the Disse space [10], it may be better to aim at the relatively central side, as in our case. The hepatic lymphatic vessel system includes a superficial system of the hepatic capsule and a deep system that runs parallel to the portal vein or hepatic vein [10]. It is presumed that no critical adverse event occurs after the embolization of the lymphatic vessels around the portal vein. Guez et al. [3] reported embolization with 0.5 mL of Onyx, and Nguyen et al. [5] reported sclerotherapy using 6 mL of lauromacrogol 400 (polidocanol) foam; however, apparently some interventional radiologists are not accustomed to such embolic or sclerosing material. Kojima et al. [4] reported retrograde sclerotherapy using Picibanil (OK-432) at the leakage cavity. In the present case, embolization using NBCA glue injected via the transhepatic lymphangiography route was simple and effective.
In conclusion, embolization using NBCA glue via the percutaneous transhepatic lymphangiography route may be an effective treatment option for post-surgical hepatic lymphorrhea.
References
Tanaka K, Ohmori Y, Mohri Y, Tonouchi H, Suematsu M, Taguchi Y, et al. Successful treatment of refractory hepatic lymphorrhea after gastrectomy for early gastric cancer, using surgical ligation and subsequent OK-432 (Picibanil) sclerotherapy. Gastric Cancer. 2004;7:117–21.
Inoue Y, Hayashi M, Hirokawa F, Takeshita A, Tanigawa N. Peritoneovenous shunt for intractable ascites due to hepatic lymphorrhea after hepatectomy. World J Gastrointest Surg. 2011;3:16–20.
Guez D, Nadolski GJ, Pukenas BA, Itkin M. Transhepatic lymphatic embolization of intractable hepatic lymphorrhea. J Vasc Interv Radiol. 2014;25:149–50.
Kojima M, Inoue M, Yamamoto S, Kanai T, Nakatsuka S, Nakagawa M. Successful treatment of hepatic lymphorrhea by percutaneous transhepatic lymphangiography followed by sclerotherapy using OK-432. Surg Case Rep. 2019;5:203.
Nguyen NC, Inoue M, Le TL, Pham HC, Trinh HS, Pham DH, Delphine N, et al. Intrahepatic lymphatic channel sclerotic embolization for treatment of postoperative lymphatic ascites: a report of 3 cases. Radiol Case Rep. 2020;15:2353–7.
Inoue M, Nakatsuka S, Yashiro H, Tamura M, Suyama Y, Tsukada J, et al. Lymphatic intervention for various types of lymphorrhea: access and treatment. RadioGraphics. 2016;36:2199–211.
Nadolski GJ, Chauhan NR, Itkin M. Lymphangiography and lymphatic embolization for the treatment of refractory chylous ascites. Cardiovasc Intervent Radiol. 2018;41:415–23.
Matsumoto T, Yamagami T, Kato T, Hirota T, Yoshimatsu, Masunami T, et al. The effectiveness of lymphangiography as a treatment method for various chyle leakages. Br J Radiol. 2009;82:286–90.
Kariya S, Nakatani M, Yoshida R, Ueno Y, Komemushi A, Tanigawa N. Repeated intranodal lymphangiography for the treatment of lymphatic leakage. Lymphology. 2015;48:59–63.
Itkin M, Nadolski GJ. Modern techniques of lymphangiography and interventions: current status and future development. Cardiovasc Intervent Radiol. 2018;41:366–76.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed Consent
Informed consent for the percutaneous transhepatic lymphangiography and embolization procedures was obtained from the patient.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hasegawa, T., Tsuboi, M., Fukushima, K. et al. Refractory Hepatic Lymphorrhea: Percutaneous Transhepatic Lymphangiography and Embolization with n-Butyl-2-Cyanoacrylate Glue. Cardiovasc Intervent Radiol 44, 1127–1130 (2021). https://doi.org/10.1007/s00270-021-02802-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-021-02802-8