Abstract
Purpose
To demonstrate feasibility and safety of ultrasound-guided popliteal sciatic nerve block for providing analgesia during urgent endovascular treatment of critical limb ischemia with resting pain.
Materials and Methods
Ultrasound-guided popliteal sciatic blocks were performed by an interventional radiologist in angiography suite immediately prior to commencement of urgent endovascular treatment of 30 critical limb ischemia patients. Subjective pain levels prior to and following sciatic block were assessed using the visual analog scale (VAS). Need for any supplemental anxiolytics or analgesics during treatment was recorded. Post-procedural evaluation of patient and operator satisfaction levels regarding the intervention was also documented.
Results
Ultrasound-guided sciatic block provided adequate analgesia in all patients; VAS scores were 0 (no pain) in 87% and 1–3 (mild to annoying pain) in 13%. Two patients required anxiolytic premedication. Additional analgesia was not required during course of endovascular treatment of any patients. Time necessary to perform sciatic block ranged 3–9 (mean 5.9 ± 1.3) min. Median number of needle attempts was 1 (range 1–3). Onset of satisfactory block ranged from 5 to 20 min (mean 9.4 ± 2.6 min). Mean treatment time was 102.2 ± 36.7 min, and balloon time was 22.4 ± 6.1 min. Patient and operator satisfaction with pain control were very good in all cases. There were no procedure-related complications.
Conclusions
Ultrasound-guided popliteal sciatic block is a feasible and safe alternative for providing adequate analgesia during urgent endovascular treatment of critical limb ischemia with resting pain.
Level of Evidence
Level 4, case series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endovascular treatment of critical limb ischemia involves long and painful procedures which often require anesthesia. Particularly patients presenting with ischemic resting pain require higher levels of analgesia in order to endure such long interventions. On the other hand, critical limb ischemia patients tend to have significant comorbidities which make them poor candidates for deep sedoanalgesia or general anesthesia [1]. Regional anesthesia with sciatic nerve block is a less invasive and more cost-effective pain management alternative to general anesthesia during ambulatory orthopedic and vascular surgical procedures and has lower post-procedure morbidity, such as nausea and pain, or post-anesthesia care needs [2]. In this setting, real-time ultrasound guidance is known to provide faster and more efficient regional anesthesia compared to landmark-based techniques [3, 4]. Though ultrasound-guided sciatic nerve block offers potential advantages during endovascular treatment of critical limb ischemia with severe resting pain, there is no study regarding its feasibility and effectiveness in this context yet. This study aims to address these issues.
Materials and Methods
Study was carried out by the interventional radiology center of a tertiary referral hospital on patients receiving endovascular treatment for critical limb ischemia. A specific subgroup of patients, comprising those with severe resting pain who required urgent endovascular recanalization, had received sciatic block in order to relieve ischemic foot pain, thus improving patient comfort and prevent unnecessary limb movements during procedure. Institutional review board approval was obtained for retrospective evaluation of prospectively collected data from January 2016 to May 2017. An interventional radiologist and an anesthesiologist assessed patients during inclusion process; risk of complications associated with, and contraindications to, regional sciatic block, and alternative anesthesia options were evaluated on per-case basis. Potential risks and benefits of sciatic block and endovascular treatment of critical limb ischemia, were carefully explained to each patient. Apart from a patient’s preference to go with the general anesthesia or deep sedoanalgesia options, previous experience of major allergic reactions to local anesthetics or contrast agents, history of sensory or motor neurologic deficit in lower limb, and pregnancy were established as exclusion criteria. A total of 30 patients (2 female, mean age 52.2 ± 18.7, range 28–79 years) referred for urgent revascularization of critical limb ischemia with resting pain were included after obtaining further consent, either verbally by phone calls or in written form during regular control visits, to use their relevant medical data.
Prior to initiation of sciatic block, all patients were informed about signs of local anesthetic toxicity such as circumoral numbness, metallic taste, lightheadedness, dizziness, visual and auditory disturbances such as difficulty focusing and tinnitus, disorientation and drowsiness [5, 6]. An anesthesiologist observed all patients throughout the procedure; vital signs were monitored with non-invasive blood pressure measurement, continuous ECG tracing, and pulse oximetry. Premedication with anxiolytics was not routinely administered because cooperation with an alert patient was required.
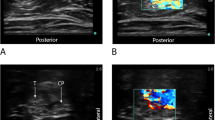
Ultrasound-guided sciatic nerve block was performed by the same operator who had prior training in, and more than 5 years of experience with, imaging-guided regional anesthesia procedures. Under aseptic conditions and patient lying prone on angiography table, linear 9–13 MHz transducer (Logiq S8, GE Healthcare, Massachusetts) was placed transversely across popliteal fossa over popliteal crease. Popliteal artery, vein and tibial nerve complex was visualized, and then transducer was moved proximally to locate bifurcation point of sciatic nerve which is the optimal site for sciatic block. At this level, tibial and common peroneal nerves branch out distally from sciatic trunk, but are still contiguous and display a bilobular pattern (Fig. 1). Needle insertion was made at the point providing shortest distance from skin near the probe to the upper margin of sciatic trunk.
A small skin wheal was raised with 1 mL of prilocaine 1% (Citanest 10 mg/ml, AstraZeneca, UK). A 21G 90 mm Quincke-type needle was advanced under real-time visualization using an in-plane technique, i.e., needle in parallel with linear probe, until its tip reached epimysium of adjacent muscle around sciatic nerve (Fig. 2). Needle was further advanced into subepimyseal perineural zone, which is between epimysium and paraneural sheath, and 1 mL prilocaine 1% was injected gently in order to widen this potential space and to improve visualization of paraneural sheath. Needle tip position is confirmed by tactile feedback, aptly named fascial pop or click, as the needle is advanced through paraneural sheath; and also by observing separation of tibial and common peroneal nerve trunks upon injection of local anesthetic solution. At this point, 18 ml of prilocaine 1% was slowly injected; then, without removing the needle tip, 20 ml of bupivacaine 0.25% (10 mL of Marcaine 5 mg/ml, AstraZeneca, UK diluted with 10 mL normal saline) was injected forming an anechoic cuff around the nerves (Fig. 3). Needle tip was repositioned under ultrasound guidance if neural swelling is observed or local anesthetic spread was deemed suboptimal during injection, or if patient complained of paresthesia.
Resting pain levels were evaluated just prior to and at every 5 min for 20 min after sciatic block by an independent observer using visual analog scale (VAS) who was not present during block administration. In patients with inadequate response to regional block, i.e., VAS ≥ 4 after 20 min, the operator administered additional 20 mL of prilocaine 1% into the local anesthetic cuff under ultrasound guidance, and VAS scores were reassessed prior to commencing with endovascular intervention. Clinical recommendations for good practice when performing peripheral nerve blocks were followed, and the standard dosage of prilocaine (200 mg) and bupivacaine (50 mg) administered in this study was in concordance with guidelines limiting each agent’s dose to prevent systemic toxicity [6,7,8]. Standard endovascular recanalization procedures were performed in accordance with guidelines for treatment of critical limb ischemia. Patients with significant procedure-related anxiety were premedicated with 1 mg midazolam intravenously. In cases of breakthrough pain, such as during balloon dilatation, regional anesthesia was planned to be supplemented with intravenous fentanyl in 25–50 μg increments.
Results
Ultrasound-guided sciatic nerve block was technically successful, i.e., ultrasound confirmed an anechoic cuff of local anesthetics around sciatic nerve bifurcation, in all patients. Despite local anesthetic infiltration in needle entry sites, 4 patients (13%) complained of minor pain during initial needle insertion. Two patients (7%) reported suboptimal pain reduction after first 20 min, with VAS = 5 in both cases, were administered additional 20 mL prilocaine 1% as described previously. Two patients (7%) required premedication with intravenous midazolam 1 mg in order to relieve procedure-related anxiety. Regional anesthesia with sciatic block provided satisfactory procedural analgesia in all patients; thus, additional analgesia with intravenous fentanyl was not required in any patients during the course of endovascular treatment.
Time necessary to perform the block ranged between 3 and 9 min (mean 5.9 ± 1.3 min). Median number of needle attempts was 1 (range 1–3). Onset of complete block among patients with successful sciatic block at first attempt ranged from 5 to 20 min (mean 9.4 ± 2.6 min). Mean treatment time was 102.2 ± 36.7 min, and balloon time was 22.4 ± 6.1 min. After regional block, VAS pain scores were 0 (no pain) in 26 patients and 1–3 (mild to annoying pain) in 4 patients (Fig. 4). Patient and operator satisfaction regarding pain control during treatment were assessed by employing 5-point Likert scale and were recorded as very good in all cases. One patient showed minor urticarial reaction limited to the nuchal region which was subsequently treated with intravenous antihistamines. No serious procedure-related side effects or complications were observed.
Discussion
Ultrasound-guided popliteal sciatic block enabled pain-free urgent endovascular revascularization in critical limb ischemia patients presenting with severe resting pain. Patient and operator satisfaction from regional block procedures were very good with no significant procedure-related complications. Utility of regional anesthesia in this setting had not previously been assessed for feasibility and safety.
Critical limb ischemia patients presenting with resting pain are frequently very stressful before undergoing endovascular interventions. In our practice, despite optimal explanation and reassurance prior to intervention, patients tend to request deep sedoanalgesia or even general anesthesia. This is probably due to fear of experiencing more pain in addition to their baseline suffering, which is not completely unfounded because significant breakthrough pain may be observed during balloon dilatation of recanalized crural arteries even under optimal sedoanalgesia. On the other hand, any analgesia or anesthesia option that requires monitored anesthesia care has inherent risks to consider such as confusion, restlessness, loss of cooperation or worse, respiratory depression and hypotension [6, 9]. This patient group, due to underlying systemic pathologies they have, is especially more susceptible to such effects. With no significant complications observed, ultrasound-guided sciatic block has proven useful in urgent treatment of our fragile patients.
Prior to implementation of ultrasound-guided sciatic block in urgent procedures, we had to recruit an anesthesiologist to the angio suite, often on very short notice, from the already understaffed emergency operating rooms. Patient-related factors such as patient having recently eaten or history of severe allergic reaction to anesthetic agents, also precluded general anesthesia. This technique has helped establish a faster and more efficient work flow in both angio suite and anesthesiology department. Reduced delay in treatment of urgent patients has also diminished any potential, and perhaps otherwise inevitable, risk of inter-departmental friction.
Randomized trials reported lower incidence of paresthesia and nerve injury with ultrasound-guided popliteal sciatic blocks compared to other nerve localization techniques [10,11,12,13,14]. Meta-analyses conclude that ultrasound guidance had not only improved onset and quality of block, but also lowered risk of unintended vascular puncture, hence incidence of local anesthetic systemic toxicity [5, 7]. In this series, operators did not expect full immobilization of limbs during endovascular treatment; thus, motor blockade of tibial and common peroneal nerves was not tested [15]. Nevertheless, improved cooperation from unsedated patients provided optimal leg immobility for operator comfort during interventions. On the other hand, as much as we prefer having full cooperation from our patients, there were frequent instances when even unsedated ones spontaneously fell asleep during mid-intervention: Patients with severe resting limb pain usually suffer from chronic insomnia; once the pain subsides following sciatic block, these already fatigued patients tend to sleep from exhaustion. In such occasions, we opted for not waking the patient throughout remainder of procedure; this did not have negative effects on clinical outcomes.
Since all sciatic blocks were performed by a single operator experienced in ultrasound-guided local injection procedures, reproducibility of the technique along with interoperator differences and learning curve of the technique remain to be addressed. In this study, we did not aim to establish a minimum effective volume required for an adequate block; thus, a standard dose of local anesthetics, i.e. safe but rather arbitrary, was administered to all cases [6]. On the other hand, there are studies reporting effectiveness of comparably lower doses of local anesthetics in such procedures [15,16,17]. Though our results are encouraging, the rather small number of cases and absolute scarcity of complications related to sciatic block procedure in this single-center preliminary series may also be considered as a limitation. As experience in this technique builds up, larger-scale research establishing the reliability of ultrasound-guided popliteal sciatic nerve block will encourage more common use of this potential prospect in urgent treatment critical limb ischemia.
Another limitation of this study is indeed inherent to its methodology and thus unavoidable: Pain levels were measured using a 10-point grading system, the visual analog scale, or VAS; and patient and operator satisfaction, likewise, were gauged using questionnaires in 5-point Likert scale response formats. These grading techniques assume that intensity of experience is linear and that attitudes or actual behavior, rather than intentions and subjective inclinations, can be accurately measured. Though there are no proven better alternatives to these, in a statistical point of view, such assumptions may diminish validity of data [18].
In conclusion, ultrasound-guided popliteal sciatic nerve block is a feasible and effective regional anesthesia technique to relieve procedural and resting pain. This practice has potential to improve efficient use of radiologic and anesthetic resources and with appropriate training is likely to be a reliable alternative to general anesthesia or deep sedoanalgesia in patients requiring urgent endovascular treatment of critical limb ischemia with resting pain.
References
Marcus AJ, Lotzof K, Kamath BS, et al. A new approach: regional nerve blockade for angioplasty of the lower limb. Cardiovasc Intervent Radiol. 2006;29:235–40.
Liu SS, Strodtbeck WM, Richman JM, Wu CL. A comparison of regional versus general anesthesia for ambulatory anesthesia: a meta-analysis of randomized controlled trials. Anesth Analg. 2005;101:1634–42.
Kent ML, Hackworth RJ, Riffenburgh RH, et al. A comparison of ultrasound-guided and landmark-based approaches to saphenous nerve blockade: a prospective, controlled, blinded, crossover trial. Anesth Analg. 2013;117:265–70.
McCartney CJ, Lin L, Shastri U. Evidence basis for the use of ultrasound for upper-extremity blocks. Reg Anesth Pain Med. 2010;35:S10–5.
Neal JM, Mulroy MF, Weinberg GL. American society of regional anesthesia and pain medicine checklist for managing local anesthetic systemic toxicity: 2012 version. Reg Anesth Pain Med. 2012;37:16–8.
Moran TC, Kaye AD, Mai AH, Bok LR. Sedation, analgesia, and local anesthesia: a review for general and interventional radiologists. Radiographics. 2013;33:E47–60.
Neal JM. Ultrasound-guided regional anesthesia and patient safety: update of an evidence-based analysis. Reg Anesth Pain Med. 2016;41:195–204.
Sermeus L, Pirson A, Breebaart B, et al. Clinical guidelines for the practice of peripheral nerve blocks in the adult. Acta Anaesthesiol Belg. 2013;64:105–8.
Lehman MA, Lind LJ. Sedation, analgesia, and anesthesia. In: Kandarpa K, Machan L, Durham J, editors. Handbook of interventional radiologic procedures. Philadelphia: Wolters Kluwer; 2016. p. 590–600.
Perlas A, Brull R, Chan VW, McCartney CJ, Nuica A, Abbas S. Ultrasound guidance improves the success of sciatic nerve block at the popliteal fossa. Reg Anesth Pain Med. 2008;33:259–65.
Mariano ER, Loland VJ, Sandhu NS, et al. Comparative efficacy of ultrasound-guided and stimulating popliteal-sciatic perineural catheters for postoperative analgesia. Can J Anaesth. 2010;57:919–26.
Dufour E, Quennesson P, Van Robais AL, et al. Combined ultrasound and neurostimulation guidance for popliteal sciatic nerve block: a prospective, randomized comparison with neurostimulation alone. Anesth Analg. 2008;106:1553–8.
Danelli G, Fanelli A, Ghisi D, et al. Ultrasound vs nerve stimulation multiple injection technique for posterior popliteal sciatic nerve block. Anaesthesia. 2009;64:638–42.
Bendtsen TF, Nielsen TD, Rohde CV, Kibak K, Linde F. Ultrasound guidance improves a continuous popliteal sciatic nerve block when compared with nerve stimulation. Reg Anesth Pain Med. 2011;36:181–4.
Bang SU, Kim DJ, Bae JH, Chung K, Kim Y. Minimum effective local anesthetic volume for surgical anesthesia by subparaneural, ultrasound-guided popliteal sciatic nerve block: a prospective dose-finding study. Medicine. 2016;95:e4652.
Latzke D, Marhofer P, Zeitlinger M, et al. Minimal local anaesthetic volumes for sciatic nerve block: evaluation of ED 99 in volunteers. Br J Anaesth. 2010;104:239–44.
Keplinger M, Marhofer P, Marhofer D, et al. Effective local anaesthetic volumes for sciatic nerve blockade: a clinical evaluation of the ED99. Anaesthesia. 2015;70:585–90.
Jamieson S. Likert scales: how to (ab)use them. Med Educ. 2004;38:1217–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Animal and Human Rights Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Tureli, D., Deniz, S., Unlukaplan, A. et al. Ultrasound-Guided Popliteal Sciatic Block Provides Adequate Analgesia During Urgent Endovascular Treatment of Critical Limb Ischemia with Resting Pain. Cardiovasc Intervent Radiol 41, 43–48 (2018). https://doi.org/10.1007/s00270-017-1802-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-017-1802-2