Abstract
Background
As a minimally invasive treatment for common bile duct (CBD) stones, ultrasound-guided percutaneous transhepatic cholangioscopic lithotripsy (PTCSL) is gaining attention and recognition from the medical community.
Methods
A retrospective analysis was conducted on patients with CBD stones treated in our hospital from January 2016 to April 2022. Patients were divided into three groups: 77 treated with PTCSL, 93 with endoscopic retrograde cholangiopancreatography (ERCP), and 103 with laparoscopic common bile duct exploration (LCBDE). Their clinical data, perioperative indicators, and complications were analyzed comparatively. Then, risk factors for the post-PTCSL recurrence of CBD stones were analyzed by logistic regressions. Finally, the receiver operating characteristic curve was drawn.
Results
All perioperative indicators of the PTCSL group were better than the LCBDE group (P < 0.001). The incidences of cholangitis, hemobilia, and incisional infection after surgery were lower in the PTCSL group than in the LCBDE group (P < 0.05). Pancreatitis, reflux esophagitis, and papillary stenosis occurred less frequently in the PTCSL group than in the ERCP group (P < 0.05). Logistic regression analysis indicated that gallstones and family history were independent risk factors. The AUC for recurrent CBD stones predicted by multi-indicators was 0.895 (95% CI 0.792–0.999, P < 0.001) with a sensitivity of 96.7% and specificity of 68.8%.
Conclusions
Ultrasound-guided PTCSL is a safe and effective treatment for CBD stones. Patients recovered quickly with fewer postoperative complications. It can be a first-line treatment for CBD stones. Gallstones and family history are independent risk factors for recurrent CBD stones, which provide a reference for clinicians in identifying the high-risk population needing close follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Common bile duct (CBD) stones are a common biliary disease and a major cause of benign biliary obstruction [1]. CBD stones can also lead to complications such as cholangitis, pancreatitis, and jaundice. It is clinically necessary to manage CBD stones as soon as possible, even if the patients are asymptomatic [2]. Currently, CBD stones are mainly treated with endoscopic retrograde cholangiopancreatography (ERCP) [3]. However, ERCP is unsuitable for patients who experienced gastrointestinal or biliary surgery, as the partial abnormalities of biliary anatomy after surgery will render the ERCP ineffective [4]. Laparoscopic common bile duct exploration (LCBDE) is the primary treatment alternative for whom ERCP is not successful or possible [5]. Previous surgeries involving the upper abdomen pose an increasing challenge for LCBDE due to potential complications in identifying the anatomical structures of Calot’s triangle and the CBD [6, 7]. As a new treatment option, the ultrasound-guided percutaneous transhepatic cholangioscopic lithotripsy (PTCSL) can clear the stones by inserting a choledochoscope through a tract created between the skin and intrahepatic duct with ultrasound guidance. Stones at the end of the bile duct can be taken and biliary stricture can be fixed with minimal invasion and fast recovery, avoiding repeated open surgery. These advantages make PTCSL an essential treatment for CBD stones. However, this minimally invasive technique has not been fully popularized. PTCSL remains to be a second-line treatment for CBD stones and there are few related studies. Therefore, a retrospective analysis was conducted on patients undergoing PTCSL, ERCP, and LCBDE in our hospital. The clinical data, perioperative indicators, and postoperative complications were compared to evaluate the clinical efficacy and safety of PTCSL in treating CBD stones. It is expected that this research could provide evidence for clinical practice. We also hope that the comparative analysis of risk factors for the post-PTCSL recurrence of CBD stones would serve as a reference for clinicians in identifying the high-risk population to follow up closely.
Materials and methods
Research subjects
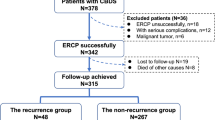
Patients underwent ultrasound-guided PTCSL/ERCP/LCBDE for CBD stones in our hospital from January 2016 to April 2022. A total of 85 participants were treated with PTCSL, 170 with ERCP, and 206 with LCBDE. Inclusion criteria: (1) aged 18 years and older; (2) diagnosed with CBD stones via color Doppler ultrasound, CT, or MRCP; (3) preoperative liver function graded as Child–Pugh class A, class B; (4) no residual stones shown in postoperative cholangiography or CT; (5) followed up by 6 months and longer. Exclusion criteria: patients with biliary malformations or malignant tumors; (2) pregnant and breastfeeding women; (3) absent or incomplete clinical data; (4) failure of the operation or a change in the course of surgery patients. Finally, 77 participants treated with PTCSL, 93 with ERCP, and 103 with LCBDE were included.
Examination procedures
PTCSL group
When general anesthesia was delivered, ultrasound-guided percutaneous transhepatic biliary drainage (PTBD) was performed following the standard surgical procedure. Detailed steps are as follows: first, the desired bile duct was punctured using an 18-gauge coaxial needle (Hakko, Japan) under ultrasound guidance (Fig. 1a). Upon the successful puncture of the bile duct, the core needle was removed, and a 0.018-inch guidewire (Cook, America) was advanced into the bile duct along the outer needle which was then withdrawn. A dilator catheter from 8F to 16F (Cook, America) was placed along the guidewire to dilate the passage. After the passage was dilated, a 16-gauge sheath (SPECATH, Foshan, China) was inserted along the guidewire (Fig. 1b). Last, a rigid choledochoscope (CHF type P10, Olympus, Tokyo, Japan) was placed into the bile duct through the sheath for performing PTCSL (Fig. 1c). Assisted with choledochoscope, the stone was extracted (Figs. 1d, 2a) via basket (Cook, America) or clamp (Richard Wolf, Germany). The CBD stones were fragmented with a pneumatic urological lithotripter (Swiss LithoClast, Switzerland) and probe (Swiss LithoClast, Switzerland) when necessary, and then flushed out of the body with water. All procedures were performed in the CBD via sheath without contact with the tract wall. Once the procedures were completed, choledochoscope and ultrasound were used to check the presence of residual stones. The stones left could be removed precisely with ultrasound guidance. If the stones were all cleared, cholangiography was conducted forthwith (Fig. 3a) to evaluate the patency of the duodenal papilla (Fig. 3b). In the end, a 16F external biliary drainage catheter was placed with ultrasound guidance (Fig. 2b) to drain the bile for 2–3 days, and a follow-up cholangiography via DSA or CT was carried out (Fig. 2c, d). Outpatient follow-up visits lasted more than six weeks after the surgery, and the drainage tube was clamped for a period of 1–2 days. If there were no indications of fever or jaundice during this period, the catheter was then safely removed.
LCBDE group and ERCP group
LCBDE was performed under general anesthesia following the standard surgical procedure. Once the procedure was completed, choledochoscope was used to check if there were intrahepatic duct (IHD) stones retained. After the surgery, a 14Fr drainage catheter (SDTE, Shandong, China) was inserted into the CBD in the surgical site for postoperative drainage and cholangioscopy. If residual stones were detected by postoperative cholangioscopy, they would be removed through the drainage tract.
Midazolam and Propofol were administered intravenously for sedation prior to ERCP. All procedures were performed using a duodenoscope (JF-260 V, TJF-260 V, Olympus, Tokyo, Japan). The catheter was inserted into the CBD through the duodenal papilla. If necessary, endoscopic papillary balloon dilation (EPBD) or endoscopic sphincterotomy (EST) would be performed. Standard techniques such as basket, balloon, or mechanical lithotripsy were adopted to clear stones. After the surgery, a nasobiliary catheter was placed into the CBD for temporary drainage. If the postoperative cholangiography was normal, the nasobiliary catheter would be withdrawn 3–5 days after the surgery.
Data collection
Data collected from three groups included: (1) participants’ characteristics before the surgery; (2) perioperative indicators, such as the duration of surgery, the amount of intraoperative bleeding, postoperative hospital stays, the time to pass gas after surgery, postoperative pain VAS score (0–10, the higher the score, the worse the pain) [8], and cost. (3) complications, including hemobilia, cholangitis, pancreatitis, intra-abdominal infection, incisional infection, recurrent stones, reflux esophagitis, papillary stenosis, and biliary stricture; (4) univariate and multivariate logistic regression analyses of risk factors for the post-PTCSL recurrence of CBD stones.
Follow-up
Participants returned to our hospital for CT scans and color Doppler ultrasound examinations 6 months after discharge to identify whether stones or complications occurred. Additionally, participants present with related symptoms would undergo a follow-up check at once. All participants were followed up for no less than 6 months until October 2022.
Statistical analysis
Statistical analyses were performed using SPSS, version 24.0. Enumeration data were presented with frequency (percentages). χ2 test was used to compare groups. Measurement data were expressed as mean ± standard deviation (mean ± sD). A univariate analysis of variance (ANOVA) was employed in comparison between groups. Nonnormally distributed measurement data was shown in the median (interquartile range) [M (P25, P75)], and groups were compared using a nonparametric test (Kruskal–Wallis). A logistic regression model was adopted for univariate and multivariate analyses. P < 0.05 was considered to be statistically significant. A receiver operating characteristic (ROC) curve was drawn with the area under the curve (AUC) applied to assess the effectiveness of prediction.
Results
Characteristics of participants
There was no statistically significant difference in participants’ characteristics, including age, sex, the state of CBD stones, clinical symptoms, and medical history among the three groups (P > 0.05), see Table 1.
Perioperative indicators
The LCBDE group exhibited a higher level than the PTCSL group and ERCP group in the duration of surgery, the amount of intraoperative bleeding, postoperative hospital stays, the time to pass gas, postoperative pain VAS score, and cost (P < 0.001). There was no statistically significant difference between the PTCSL group and the ERCP group (P > 0.05), see Table 2.
Complications
Among 93 participants in the ERCP group, pancreatitis occurred in 5 (5.4%), reflux esophagitis in 7 (7.5%), and papillary stenosis in 4 (4.3%). As for 103 participants in the LCBDE group, cholangitis occurred in 11 participants (10.7%), hemobilia in 9 (8.7%), and incisional infection in 8 (7.8%). In the PTCSL group of 77 participants, cholangitis occurred in 2 (2.6%), hemobilia in 1 (1.3%), and incisional infection in 1 (1.3%). The LCBDE group had a higher incidence of cholangitis than the PTCSL group (P < 0.05). Compared with the PTCSL group and the ERCP group, the LCBDE group experienced hemobilia and incisional infection more frequently (P < 0.05). The incidence of pancreatitis in the ERCP group was higher than in the PTCSL group (P < 0.05). The ERCP group manifested a higher incidence of reflux esophagitis and papillary stenosis than the PTCSL group (P < 0.05). In comparison with the PTCSL group and the ERCP group, recurrent CBD stones were less frequent in the LCBDE group (P < 0.05). No statistically significant difference was found in the incidences of intra-abdominal infection, and biliary stricture among the three groups (P > 0.05). See Table 3
Analysis of risk factors for the post-PTCSL recurrence of CBD stones
Univariate logistic regression analyses identified age (≥ 60), the internal diameter of CBD (≥15 mm), jaundice, gallstones, hyperlipidemia, cholangitis, and family history as risk factors associated with the post-PTCSL recurrence of CBD stones (P < 0.05). In addition, multivariate logistic regression analyses indicated that gallstones and family history were independent risk factors for recurrent CBD stones (P < 0.05), see Table 4.
The accuracy of risk factors in predicting the recurrence of CBD stones
The AUC for the ROC curves of the post-PTCSL recurrence of CBD stones predicted by gallstones and family history was 0.795 and 0.734, respectively. The AUC for the curve of the recurrence of CBD stones predicted by multi-indicators was 0.895 (95% confidence intervals was 0.792–0.999, P < 0.001) with a sensitivity of 96.7% and a specificity of 68.8%. See Fig. 4
Discussion
PTCSL is minimally invasive. This unconventional surgical treatment for CBD stones has drawn the medical community’s attention [9, 10]. Previously, the percutaneous transhepatic puncture was performed under X-ray guidance, which is somewhat blind. In contrast, ultrasound-guided percutaneous transhepatic puncture has gained more popularity among scholars for its advantages, such as observing how the bile ducts and blood vessels travel and adjusting the puncture approach in real-time to enhance the success rate of the puncture.
While ERCP is considered a first-line treatment for CBD stones, its success rate may be compromised in patients with anatomical abnormalities within the digestive system that impede endoscopic access to the biliary tree. In addition to previous gastric or bile duct surgeries, modern obesity surgeries can also create challenges in accessing the papilla. In these circumstances, PTCSL is preferred. ERCP has an incidence of complications that cannot be ignored in previous research [2, 11]. In this research, pancreatitis, reflux esophagitis, and papillary stenosis were not found in the PTCSL group. Such a difference is attributable to the EST used in the ERCP. EST can destroy the Oddi sphincter, which may lead to long-term postoperative complications such as papillary stenosis, pancreatitis, reflux esophagitis caused by bile reflux, bacterial infection, and inflammation of the bile duct system [12, 13]. In the PTCSL procedure, the anatomy and function of the Oddi sphincter are intact, which can minimize the damage to the duodenal papilla by the medical apparatus when clearing stones, avoid the reflux of food and digestive juice into the bile duct, and lower the incidence of postoperative pancreatitis and reflux esophagitis [4, 14].
LCBDE is the primary alternative for treating CBD stones, but there still remain 5–10% of CBD stones difficult to be removed [15]. In the LCBDE group of this research, cholangitis occurred more frequently than in the PTCSL group. The postoperative incidence of cholangitis is a critical parameter for evaluating the long-term outcomes of the surgery for CBD stone removal [16]. Additionally, it should be noted that LCBDE incurs higher costs compared to the other two groups. In the PTCSL procedure, the best approach to puncturing the desired bile duct is determined with ultrasound guidance, keeping away from the intestines, blood vessels, and chest cavity. A rigid or soft choledochoscope and protective sheath are employed. All procedures are completed within the protective sheath placed in the dilated bile duct to prevent the livers and bile ducts from damage and minimize the possibility of cholangitis. PTCSL outperforms LCBDE for its advantages, such as short surgery duration, less blood loss, short postoperative hospital stays, fewer days before passing gas, and milder pain after the surgery. Meanwhile, intraoperative cholangiography was implemented. A diluted contrast agent was injected with the guidance of a choledochoscope to observe the patency of the lower part of CBD and duodenal papilla and the opening and closing of the Oddi sphincter. Cholangiography was able to ensure the biliary obstruction was relieved, avoid damage to the duodenal papilla by apparatus, and improve the success rate of surgery.
However, the results of the follow-up indicated a recurrence rate of up to 20.8% after the PTCSL. Gallstones and family history are independent risk factors for the post-PTCSL recurrence of CBD stones. Ando et al. [17] also found that gallstones were an independent risk factor for recurrent CBD stones. This is because gallstones have a propensity to migrate into the CBD and block the flow of bile. This disrupted flow hinders the effective clearance of all stones, resulting in the presence of residual small stones within the duct and subsequently leading to CBD stone formation [18, 19]. In this study, the LCBDE group had the lowest recurrence rate of CBDS, which could be attributed to the concurrent performance of cholecystectomy. Positive family history of gallstones is a universally acknowledged risk factor for gallstones. It is reported that people with a family history of bile duct stone may have a doubled risk of developing it, and first-degree relatives of patients with bile duct stone may experience a higher incidence of it [20]. Previous research stated that the diameter of CBD ≥ 15 mm and cholangitis were independent risk factors for recurrent CBD stones [21]. Although clinical symptoms after removing stones can be mitigated quickly, cholangitis still exists, and cholangitis will stimulate the Oddi sphincter repetitively and disrupt the flow and drainage of bile, resulting in recurrent CBD stones. In this research, the diameter of CBD ≥ 15 mm and cholangitis are related risk factors for recurrent CBD stones instead of independent ones, which is possibly ascribed to the less frequent recurrence of CBD stones among participants in this research. Therefore, the relationship between the diameter of CBD and cholangitis should be studied further.
In addition to treating CBD stones, PTCSL is also applicable to IHD stones [22]. PTCSL can easily access the desired bile duct and deal with the stones directly. PTCSL can remove all stones from patients with IHD and CBD stones in one surgery. In contrast, it is hard to clear IHD stones using ERCP, which is mainly for removing extrahepatic bile duct stones [23]. Moreover, the recurrent and retained stones and biliary stricture will lead to high incidences of residual and recurrent stones and complications. PTCSL can cope with difficult extrahepatic and intrahepatic bile duct stones simultaneously, making it the best choice for treatment.
The limitations of this study include its retrospective design and small sample size. Therefore, it is imperative to continue long-term follow-up in order to comprehensively evaluate the safety and efficacy of PTCSL as a treatment modality for CBD stones. Furthermore, conducting multi-center research with a larger sample size is essential to identify additional independent risk factors associated with the recurrence of CBD stones after PTCSL.
In summary, PTCSL is an effective and safe surgery. PTCSL is superior to ERCP and LCBDE for quick recovery and fewer postoperative complications. It can be chosen as the first-line treatment for CBD stones and the primary treatment for patients with CBD and IHD stones, indicating a tremendous clinical application and promotion value. Gallstones and family history are independent risk factors for the post-PTCSL recurrence of CBD stones, which provide a reference for clinicians in identifying the high-risk population to follow up closely.
Availability of data and material
The data underlying this article will be shared on reasonable request to the corresponding author.
Abbreviations
- PTCSL:
-
Percutaneous transhepatic cholangioscopic lithotripsy
- CBD:
-
Common bile duct
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- LCBDE:
-
Laparoscopic common bile duct exploration
- ROC:
-
Receiver operating characteristic
- AUC:
-
The area under the receiver operating characteristic curve
- IHD:
-
Intrahepatic duct
- EST:
-
Endoscopic sphincterotomy
References
Wu Y, Xu CJ, Xu SF (2021) Advances in risk factors for recurrence of common bile duct stones. Int J Med Sci 18(4):1067–1074. https://doi.org/10.7150/ijms.52974
Cianci P, Restini E (2021) Management of cholelithiasis with choledocholithiasis: endoscopic and surgical approaches. World J Gastroenterol 27(28):4536–4554. https://doi.org/10.3748/wjg.v27.i28.4536
Manes G, Paspatis G, Aabakken L et al (2019) Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 51(5):472–491. https://doi.org/10.1055/a-0862-0346
Zhang J, Ling X (2021) Risk factors and management of primary choledocholithiasis: a systematic review. ANZ J Surg 91(4):530–536. https://doi.org/10.1111/ans.16211
Bekheit M, Smith R, Ramsay G et al (2019) Meta-analysis of laparoscopic transcystic versus transcholedochal common bile duct exploration for choledocholithiasis. BJS Open 3(3):242–251. https://doi.org/10.1002/bjs5.50132
Lyu Y, Cheng Y, Li T et al (2019) Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: a meta-analysis. Surg Endosc 33(10):3275–3286. https://doi.org/10.1007/s00464-018-06613-w
Araki K, Shirabe K, Watanabe A et al (2017) Risk factors for an additional port in single-incision laparoscopic cholecystectomy in patients with cholecystitis. J Med Invest 64(3.4):245–249. https://doi.org/10.2152/jmi.64.245
Moisset X, Attal N, Ciampi de Andrade D (2022) An emoji-based visual analog scale compared with a numeric rating scale for pain assessment. JAMA 328(19):1980. https://doi.org/10.1001/jama.2022.16940
Lin W, Chen M, Li B, Wang W, Li S, Lyu G (2022) Intraoperative ultrasound-guided percutaneous hepatocholangiostomy applied in the cholangioscopic lithotripsy for hepatolithiasis and choledocholithiasis. Surg Endosc. https://doi.org/10.1007/s00464-022-09540-z
Zhuo H, Chen Z, Lin R, Yang S, Zhuang H, He C, Liu X (2020) Percutaneous transhepatic choledochoscopic lithotomy (ptcsl) is effective for the treatment of intrahepatic and extrahepatic choledocholithiasis. Surg Laparosc Endosc Percutan Tech 31(3):326–330. https://doi.org/10.1097/SLE.0000000000000874
Yang JH, Li W, Si XK et al (2018) Efficacy and safety of therapeutic ERCP in the elderly: a single center experience. Surg Laparosc Endosc Percutan Tech 28(2):e44–e48. https://doi.org/10.1097/SLE.0000000000000499
Paspatis GA, Paraskeva K, Vardas E et al (2017) Long-term recurrence of bile duct stones after endoscopic papillary large balloon dilation with sphincterotomy: 4-year extended follow-up of a randomized trial. Surg Endosc 31(2):650–655. https://doi.org/10.1007/s00464-016-5012-9
Cheon YK, Lee TY, Kim SN et al (2017) Impact of endoscopic papillary large-balloon dilation on sphincter of Oddi function: a prospective randomized study. Gastrointest Endosc 85(4):782-790.e1. https://doi.org/10.1016/j.gie.2016.08.031
Seo YR, Moon JH, Choi HJ et al (2013) Papillary balloon dilation is not itself a cause of post-endoscopic retrograde cholangiopancreatography pancreatitis; results of anterograde and retrograde papillary balloon dilation. J Gastroenterol Hepatol 28(8):1416–1421. https://doi.org/10.1111/jgh.12277
Aburajab M, Dua K (2018) Endoscopic management of difficult bile duct stones. Curr Gastroenterol Rep 20(2):8. https://doi.org/10.1007/s11894-018-0613-1
Tazuma S, Unno M, Igarashi Y et al (2017) Evidence-based clinical practice guidelines for cholelithiasis 2016. J Gastroenterol 52(3):276–300. https://doi.org/10.1007/s00535-016-1289-7
Ando T, Tsuyuguchi T, Okugawa T et al (2003) Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut 52(1):116–121. https://doi.org/10.1136/gut.52.1.116
Choi HH, Min SK, Lee HK et al (2021) Risk factors of recurrence following common bile duct exploration for choledocholithiasis. J Minim Invasive Surg 24(1):43–50. https://doi.org/10.7602/jmis.2021.24.1.43
Cai JS, Qiang S, Bao-Bing Y (2017) Advances of recurrent risk factors and management of choledocholithiasis. Scand J Gastroenterol 52(1):34–43. https://doi.org/10.1080/00365521.2016.1224382
Maurer KR, Everhart JE, Knowler WC et al (1990) Risk factors for gallstone disease in the Hispanic populations of the United States. Am J Epidemiol 131(5):836–844. https://doi.org/10.1093/oxfordjournals.aje.a115574
Li S, Su B, Chen P et al (2018) Risk factors for recurrence of common bile duct stones after endoscopic biliary sphincterotomy. J Int Med Res 46(7):2595–2605. https://doi.org/10.1177/0300060518765605
Wang P, Sun B, Huang B et al (2016) Comparison Between percutaneous transhepatic rigid cholangioscopic lithotripsy and conventional percutaneous transhepatic cholangioscopic surgery for hepatolithiasis treatment. Surg Laparosc Endosc Percutan Tech 26(1):54–59. https://doi.org/10.1097/SLE.0000000000000222
Troncone E, Mossa M, De Vico P et al (2022) Difficult biliary stones: a comprehensive review of new and old lithotripsy techniques. Medicina (Kaunas) 58(1):120. https://doi.org/10.3390/medicina58010120
Acknowledgements
First and foremost, I would like to show my deepest gratitude to my supervisor, Dr. Lu Wuzhu, a respectable, responsible, and resourceful scholar, who has provided me with valuable guidance in every stage of the writing of this thesis. I would like to express my sincere gratitude to all my co-authors for their invaluable guidance, remarkable kindness, and unwavering patience throughout the completion of my thesis. Without their constant encouragement and support, it would have been impossible for me to accomplish this thesis.
Funding
This study has received funding by the Science and Technology Plan Medical and Health Projects of Zhuhai (ZH22036201210048PWC).
Author information
Authors and Affiliations
Contributions
“All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by WLu, XC, SZ, KH and YL. The first draft of the manuscript was written by ZG, DY, and XH, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript”.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Our institutional review board (IRB) approved this retrospective study that evaluated de-identified data and involved no potential risk to patients. This study was conducted in accordance with the current version of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Fifth Affiliated Hospital of Sun Yat-sen University (Date: June 2nd, 2022 /No. K84-1).
Informed consent
Written informed consent was obtained from all patients. No link between the patients and the researchers was made available to avert any potential breach of confidentiality.
Consent for publication
Written informed consent was obtained from all subjects (patients) in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gao, Z., Ye, D., Hong, X. et al. Ultrasound-Guided Percutaneous Transhepatic Cholangioscopic Lithotripsy for the Treatment of Common Bile Duct Stones and Analysis of Risk Factors for Recurrence. World J Surg 47, 3338–3347 (2023). https://doi.org/10.1007/s00268-023-07217-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-07217-9