Abstract
Background
Gunshot wounds to the heart are regarded as one of the most lethal penetrating injuries. There has been an increase in gunshot wounds to the chest in our institution in recent years. Injuries to the heart caused by gunshot wounds can be challenging, with patients arriving in hospital in different physiological states. We report our trauma unit’s experience with civilian gunshot wounds to the heart.
Methods
A retrospective review from January 2005 till December 2018 of those 18 years of age and above who presented to our hospital with penetrating cardiac injuries over eight years was done. Those who presented with a carotid pulse and a cardiac rhythm were included in the study. Blood pressure of less than 90 mmHg was considered as haemodynamic instability. Demographics, physiological parameters, injuries sustained, preferred surgical access to the chest, and type of surgery were analysed. The complications during their hospital stay and outpatient clinic were documented. The incidences of in-hospital mortality were also noted. Descriptive statistics with STATA version 15 were conducted. A p-value of < 0.05 was considered statistically significant.
Results
A total of 37 patients were enroled in the study; four were excluded for incomplete data. All presented directly from the scene, with a median age of 30 (IQR 24–36). Haemodynamic instability was in 64% of the cases. The most common injured chamber was the right ventricle (75.7%). There were only two complications recorded; local wound sepsis and empyema. All survivors received a post-surgical echocardiogram. The overall survival rate was 18.9% (n = 7). Of the ten that required emergency room thoracotomy, only one survived to discharge.
Conclusion
Gunshot wounds to the heart have a mortality rate greater than 80% in those arriving alive. Only one in ten of those who meet the strict criteria for emergency room thoracotomy survive hospitalisation. The local complication rate was low.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Penetrating injuries to the heart are caused by stabs, gunshot wounds and rarely, accidental impalements [1, 2]. The mechanism of penetrating cardiac injuries varies worldwide [1, 3, 4] . Data from the United States reported 70% gunshot wounds and 30% stab wounds distribution [5, 6]. Intentional gunshot wounds to the heart also contribute to the predominance of gunshot wound distribution [5,6,7,8]. However, in South Africa, the opposite is reported, with 82–94% stab wounds and 6–18% gunshot wounds [3, 9, 10].
Chest injuries are on the rise in South Africa and are often associated with high mortality rates [3, 9,10,11]. The management of penetrating chest injuries has evolved to mostly being non-operative in nature [11]. A subset of penetrating chest injuries presents following gunshot wounds [11, 12]. Gunshot wounds to the chest and abdomen are common in our institution. The management of these patients can be a challenge. Gunshot wounds to the heart are regarded as one of the most lethal penetrating injuries [2]. Survivors of gunshot wounds put an economic burden on the healthcare system [13]. The morbidity affects not only the victims but also the victim’s families [13]. Gunshots that result in homicide or mass shootings get more attention than the survivors that present to the hospital [13, 14].
These gunshot injuries can be perforating or non-perforating [15,16,17]. They can also be full thickness, tangential or result from shockwaves [15, 16]. Bullets do not always follow a straight trajectory to the target [15, 16]. Injuries resulting from shockwave injuries may be challenging to diagnose [16]. Full-thickness injuries are likely to result in multi-chamber injuries [16]. Data on multi-chambered injuries are contradictory and inconsistent [3, 4, 9,10,11,12]. A study by Degiannis showed this was not associated with poor patient outcomes [10].
The literature suggests that patients who have sustained gunshots present in a worse physiological state than those who sustained stab wounds [5, 18]. More than 70% of patients who sustain gunshot wounds present with no signs of circulation or respiration [5, 18]. Furthermore, cardiac tamponade was reported to be less and exsanguination more common in gunshot injuries than in stabs [12, 15, 19]. Gunshot wounds can cause disruptive injuries to the heart, which promote exsanguination and decompression into the chest cavity [5, 18]. When cardiac tamponade is present, it has favourable outcomes [18].
It is unsurprising that gunshot heart injuries are rare and are said to have poor outcomes [3, 4, 9,10,11,12]. However, despite the high mortality rates, with improvements in prehospital care and surgical skills, we see more case reports of patients with penetrating cardiac injuries being salvaged [5, 18, 20, 21]. It was worth looking at our experience in a low-to-middle income country with a high volume of penetrating trauma. Our unit works as a level 1 trauma that caters to all types of trauma, and the procedures are done by trauma surgeons or specialist surgeons in the department. The hospital is a 1100 bedded hospital, seeing 220 priority one cases per month and a total of 1200 total trauma cases per month. There are 18 critical beds and 26 other dedicated beds for visceral trauma (excluding orthopaedics and neurosurgery. Prehospital services are variable, with some patients arriving directly to the facility on private transport and many more arriving with prehospital services that vary from basic to advanced care. This prehospital setup is better than most Sub-Saharan countries. We hope our experience will shed light on managing these highly lethal cases.
Our study aims to describe the outcomes and injuries of patients who sustained penetrating cardiac injuries at a single institution in Johannesburg, South Africa.
Materials and methods
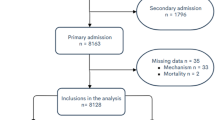
We retrospectively reviewed all patients who presented to Charlotte Maxeke Johannesburg Academic Hospital Trauma Unit with penetrating cardiac injuries from gunshots over a period of 8 years (01 January 2011–31 December 2018). The patients were identified from the hospital trauma database. All patients above the age of 18 with gunshot wounds to the heart who presented with a carotid pulse and a cardiac rhythm were included in the study. Patients who presented pulseless were not included, regardless of presence of other signs of life. Four patients who had significant missing data were excluded from the study.
Blood pressure of less than 90 mmHg was considered haemodynamic instability.
The patient’s demographics, mechanism of injury, injury severity score (ISS), physiological parameters at the scene and on presentation, investigation findings, type of operation, length of hospital stay, morbidities and in-hospital mortalities were recorded. Echocardiography was requested in all survivors post-surgical repair. All surviving candidates were followed up at least twice on an outpatient basis.
Statistical analysis
Means (± SD) are presented for continuous variables, and frequencies (%) are presented for categorical variables. All analyses were done using STATA version 15. Continuous variables were first tested for normality using the Shapiro–Wilk test. Fisher’s exact test was used to test the significance of the relationship between categorical variables. Univariate and multivariate analyses were conducted on the data. A p-value of < 0.05 was considered statistically significant.
Ethics approval was obtained from the University of the Witwatersrand Human Ethics committee and the hospital CEO. Ethics number M180463 was allocated to the study. The study was also registered on Clinical Trial.gov NCT05016986.
Results
After excluding four patients for missing data, 37 patients that sustained penetrating gunshot wounds (GSW) to the heart over eight years were enroled in the study. Thirty five (94.59%) were males and 2 (5.41%) females. The median age was 30 years (IQR 24–36). Sixty-four per cent of patients presented haemodynamically unstable (n = 24), and 13 (35%) patients were haemodynamically normal on presentation to the emergency department (see Table 1). Beck’s triad of hypotension, distended neck veins/increased CVP, and muffled heart sounds were present in about 51% of patients.
All our patients presented from the scene and were all victims of interpersonal violence. The median systolic blood pressure prehospital was 92 mmHg, with a diastolic median of 58 mmHg. The median pulse rate prehospital was 89 beats per minute. On presentation to the emergency department, the median vital signs were a systolic BP of 69 mmHg, diastolic BP of 55 mmHg and a pulse rate of 92 beats per minute. The physiological parameters in the hospital showed a median acidaemia of 7, 16 ± 0.16 and a hyperlactatemia of 7 mmol/l (IQR 4.7–10.1) with a base excess of − 11, 4 mmol/l ± 8.33. The median RTS was 5, 6 (IQR 3.6–7.6). The median ISS was 32 (IQR 26–41) (see Table 1).
The most common investigations in the emergency department (ED) were chest X-rays (73%) and chest ultrasound (55%). Echocardiograms in ED (9%) and cardiac enzymes (6%) were only done in selected cases. Intravenous lines were established in all cases, with 41% receiving central venous catheters in the ED.
Most patients sustained other associated chest injuries (59.4%) besides cardiac injuries, abdominal injuries (64.9%), head injuries (16.2%) and extremities (16.2%) (see Table 2). All patients had sustained gunshot wounds to the chest, nine cases were purely chest injuries, fourteen had thoraco-abdominal injuries, 12 had separate chest and abdominal gunshot injuries and, two had chest and extremity gunshot wounds. The most common injuries from the chest were parenchymal lung injuries (n = 13). Combined hollow and solid organs (n = 10) were the most common injuries in the abdomen (see Table 2).
Ten patients had an emergency room thoracotomy performed as they arrived in extremis. Twenty patients had an anterolateral thoracotomy in theatre. Only five had sternotomy incisions to access the thorax (see Table 3). Two other patients had clamshells for right atrial injuries. The most injured chamber was the right ventricle (n = 28), followed by the left ventricle (n = 4), right atrium (n = 2) and left atrium (n = 1) (see Table 3). There were 2 combined chamber injuries and no injuries to coronary vessels. All cardiac repairs were done with a non-absorbable polypropylene suture depending on the chamber involved. (Prolene 2/0, Prolene 3/0 and Prolene 4/0). Pledgets were utilised in atrial or auricular repairs only. All patients who survived were admitted to ICU. The complications among survivors were local wound sepsis (n = 1) and empyema (n = 1).
The mortality rate was 81.1%, with six patients (16.21%) dying in the emergency department, twelve patients (32.43%) died on the table in the theatre, eleven (29.72%) died shortly after admission to ICU, and one (2.7%) later in the ward. Nine of the ten patients who had emergency room thoracotomy due to extremis died. Six of the ten died in the emergency department and the remaining 3 in theatre. Most of the deaths occurred in theatre. Among the survivors (7/37), 6 were discharged home, and one stepped down to another hospital. Associated chest injury apart from the heart was a predictor of death (p < 0.05) (see Table 4).
Discussion
Gunshot wounds to the heart are often fatal due to the damage they inflict on the heart [1]. These can be challenging cardiac injuries to manage. There has been an increase in gunshot wounds in several countries including South Africa due to increased use of firearms, organised crime and interpersonal violence [1, 15, 22]. Most patients with gunshot wounds to the heart will die on the scene [12]. The ones that present to hospitals may be salvaged even in the absence of cardiothoracic surgery services in specialised centres [10]. Our study was focused on those who presented directly to our institution with signs of life. Our general approach to these injuries is depicted in the flow chart. Those declared dead at the scene are taken directly to the mortuary for forensic investigations.
Trauma patients are usually young males, as shown in our cohort of patients [3, 4, 9,10,11,12] [1,2,3,4,5,6]. The clinical status on presentation of these patients influences the outcomes [18]. The median systolic blood pressure was 69 mmHg; physiologically, these patients had acidaemia, hyperlactatemia and a high base deficit. These parameters reveal very sick patients when they arrive in the emergency department. The median ISS was 32, and RTS 5, 6 (see Table 4) in keeping with the energy mechanism associated with gunshot compared to stabs [23]. Up to 65% of patients with penetrating cardiac injuries present to the emergency department with no recordable blood pressure [5]. Ten patients presented agonal and had an emergency room thoracotomy in keeping with our previously reported experience [24]. Only two had a clamshell thoracotomy as we tend to reserve this approach to more complex injuries compared to other centres [25]. Other studies also showed that clinical status on presentation had a significant bearing on mortality [10, 18].
The most injured chamber of the heart was the right ventricle in 75.7% of our patients. This is in keeping with other previous studies regarding penetrating chest injuries [4,5,6, 8, 9, 12]; the explanation offered was the fact that the right ventricle is the most presenting chamber to the anterior mediastinum [1]. There were 2 patients with combined chamber injuries. This was not associated with increased mortality, as in a previous study [11]. No coronary injuries were reported in these patients who managed to present to the hospital. This may be due to selection bias, as those with complex coronary vessel injuries may have died at the scene [5, 18, 20]. Though sternotomy was utilised in only 13, 5% of the cases, it was associated with survivability (p = 0.003) (see Table 4), in keeping with our surgical practice to do sternotomy in the more stable cases.
Alive patients were admitted to ICU at the end of surgery for further monitoring and care. We conducted a postoperative echocardiogram on all survivors, and no repeat echocardiogram was ever deemed necessary at outpatient follow-up. The overall recorded morbidity rate was 5.4%, with one patient developing local wound sepsis and another developing an empyema which required a relook thoracotomy. Tang et al., in their cohort of penetrating cardiac injuries, had a complication rate of 17% in their survivors [26]. Carr et al. had up to 43% confirmed immediate complications, which settled in time [27]. Our morbidity was, therefore, lower than reported in other studies, probably in keeping with the young age noted in our cohort.
Most of our patients had combined extra-cardiac injuries, with only two having sustained isolated gunshots to the heart. Other studies showed no association between associated injuries and mortality [9, 18]. In our study, other associated chest injuries were a predictor of mortality (see Table 4). This may reflect a high injury burden to the chest cavity, which has close proximity of pivotal structures. Associated abdominal injuries were not statistically associated with mortality (p > 0.05) compared to what we had experienced when looking at outcomes in those requiring Emergency Room thoracotomy, where combined chest and abdominal injuries had poorer outcomes [24].
The overall survival of patients in our series was 18.9% (7/37), in keeping with another reported mortality rate after gunshot wounds ranging from 12 to 81% [1]. This survival rate must consider that 64.86% presented with haemodynamic instability. However, some of these studies included patients with other missiles causing penetrating cardiac injuries [1]. The 90% mortality seen in those who had emergency room thoracotomy is in keeping with our unit’s policy to perform this procedure in those presenting in extremis only [24]. A study on penetrating cardiac injuries in South Africa (stab and gunshot combined) had a mortality rate of 81% in gunshot injuries patients [10], which is similar to our findings. Our series reports on civilian gunshots only. Cardiopulmonary resuscitation before arrival, high Injury Severity Score (ISS), high Revised Trauma Score (RTS), hypotension and greater vessel injuries are known to be associated with poor outcomes in penetrating cardiac injuries [18].
Conclusion
Gunshot wounds to the heart have a high mortality rate. A survival rate of 18.9% is acceptable considering the energy transfers associated with gunshot injuries and the fact that the majority presented with haemodynamic instability. The right ventricular chamber was the most common injury site. The morbidity rate was lower than in other series. We propose a prospective multicentre study be considered in low-to-middle income countries to clarify outcomes and patterns of gunshot injuries to the heart under these circumstances.
Limitations to the study
This study was a retrospective study looking only at gunshot injuries to the heart. Bias might have been introduced by this being a single-centre study. The total study numbers were few due to only a few survivors being able to make it to an institution. This sample size could explain why we could not statistically demonstrate the direct link of BP < 90 to the mortality outcomes. The morbidity reporting was self-reported, limited to short-term follow-ups, and may have missed some minor complications. No long-term follow-up was done in our cohort.
References
Lone RA, Wani MA, Hussain Z et al (2009) Missile cardiac injuries: review of 16 years’ experience. Ulus Travma ve Acil Cerrahi Derg 15(4):353–356
Asfaw I, Arbulu A (1977) Penetrating wounds of the pericardium and heart. Surg Clin N Am 57(1):37–48
Campbell NC, Thomson SR, Muckart DJJ et al (1997) Review of 1198 cases of penetrating cardiac trauma. Br J Surg 84(12):1737–1740
Mandal AK, Sanusi M (2001) Penetrating chest wounds: 24 years’ experience. World J Surg 25(9):563–568
Buckman RF, Badellino MM, Mauro LH et al (1993) Penetrating cardiac wounds: prospective study of factors influencing initial resuscitation. J Trauma Injury Infect Crit Care 34(5):717–725
Asensio JA, Berne JD, Demetriades D et al (1998) One hundred five penetrating cardiac injuries. J Trauma 44(6):1073–1082
Luna G, Adye B, Haun-Hood M et al (2001) Intentional injury treated in community hospitals. Am J Surg 181(5):463–465
Inkinen J, Kirjasuo K, Gunn J, Kuttila K (2015) Penetrating trauma; experience from Southwest Finland between 1997 and 2011, a retrospective descriptive study. Eur J Trauma Emerg Surg 41(4):429–433
Madiba TE, Thomson SR, Mdlalose N (2001) Penetrating chest injuries in the firearm era. Injury 32(1):13–16
Degiannis E, Loogna P, Doll D et al (2006) Penetrating cardiac injuries: recent experience in South Africa. World J Surg 30(7):1258–1264
van Waes OJF, Halm JA, van Imhoff DI et al (2018) Selective nonoperative management of penetrating thoracic injury. Eur J Emerg Med 25(1):32–38
Clarke DL, Quazi MA, Reddy K, Thomson SR (2011) Emergency operation for penetrating thoracic trauma in a metropolitan surgical service in South Africa. J Thorac Cardiovasc Surg 142(3):563–568
Rhee PM, Moore EE, Joseph B et al (2016) Gunshot wounds: a review of ballistics, bullets, weapons, and myths. J Trauma Acute Care Surg 80(6):853–867
Christoffel KK (2007) Firearm injuries: epidemic then, endemic now. Am J Public Health 97(4):626–629
Pinto A, Russo A, Reginelli A et al (2019) Gunshot wounds: ballistics and imaging findings. Semin Ultrasound CT MR 40(1):25–35
Ngwisanyi W, Moeng SFAP, Moeng M (2021) Shockwave cardiac injury in thoracoabdominal gunshot wound. Int J Surg Case Rep 80:105673. https://doi.org/10.1016/j.ijscr.2021.105673
Tran HV, Charles M, Garrett RC et al (2020) Ten-year trends in traumatic cardiac injury and outcomes: a trauma registry analysis. Ann Thorac Surg 110(3):844–848
Tyburski JG, Astra L, Wilson RF et al (2000) Factors affecting prognosis with penetrating wounds of the heart. J Trauma Injury Infect Crit Care 48(4):587–590
Morse BC, Mina MJ, Carr JS et al (2016) Penetrating cardiac injuries: a 36-year perspective at an urban, level I trauma center. J Trauma Acute Care Surg 81(4):623–631
Castriconi M, Festa P, Bartone G, et al (2013) Penetrating cardiac injuries. Two case reports. Ann Ital Chir 84 (ePub):S2239253X13020987
Grabinsky A, Williamson K, Ramesh R (2011) Advances in prehospital trauma care. Int J Crit Illn Inj Sci 1(1):44–50
Naidoo S, van As AB (2011) Vulnerability of children to gunshot trauma in violence-prone environment: the case of South Africa. Afr J Paediatr Surg 8(1):101–104
Moeng M, Boffard K (2017) Baliistics in Trauma. In: George V, Elias D, Dietrich D (eds) Penetrating trauma a practical guide on operative techniques and peri_operative management, 2nd edn. Springer Nature, Berlin Heidelberg
Monzon BI, del Ortega MC, Goosen J et al (2021) Emergency room thoracotomy (ERT): a retrospective audit of results. Albanian J Trauma Emerg Surg 5(1):745–749
DuBose JJ, Morrison J, Moore L et al (2020) Does clamshell thoracotomy better facilitate thoracic life-saving procedures without increased complication compared with an anterolateral approach to resuscitative thoracotomy? Results from the American Association for the surgery of trauma aortic occlusion for resuscitation in trauma and acute care surgery registry. J Am Coll Surg 231(6):713–719
Tang AL, Inaba K, Branco BC et al (2011) Postdischarge complications after penetrating cardiac injury: a survivable injury with a high postdischarge complication rate. Arch of Surg 146(9):1061–1066. https://doi.org/10.1001/archsurg.2011.226
Carr JA, Buterakos R, Bowling WM et al (2011) Long-term functional and echocardiographic assessment after penetrating cardiac injury: 5-year follow-up results. J Trauma 70(3):701–704. https://doi.org/10.1097/TA.0b013e31820c405a
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moeng, M.S., Makhadi, S. & Molewa, M.C. Outcomes of Cardiac Gunshot Injuries Presenting at an Urban Trauma Facility in Johannesburg, South Africa. World J Surg 47, 863–869 (2023). https://doi.org/10.1007/s00268-022-06879-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06879-1