Abstract
Background
Pheochromocytoma and paraganglioma (PPGL) are rare neuroendocrine tumours, often associated with germline mutations that influence the disease biology and clinical course. We aimed to describe the genotypic and phenotypic characteristics of a consecutive series of PPGL patients and correlate mutation status with clinical outcomes.
Methods
We performed a retrospective cohort study of all PPGL patients who presented to a tertiary referral centre between March 2005 and February 2022. Genotypic, phenotypic and follow-up data were analysed.
Results
A total of 140 patients were included. Of these, 94 (67%) patients underwent genetic testing and a mutation was detected in 36 (38%) patients. Mutation presence was associated with younger age, smaller tumour size and bilateral adrenal tumours. Disease recurrence occurred at a median time of 5.4 (IQR 2.8–11.0) years after treatment in 21 (15%) patients, of which 14 (67%) had a mutation in a susceptibility gene. Recurrence pattern was influenced by mutation type; higher local recurrence risk for SDHA, SDHB, and MEN2B disease, and higher metastatic risk for SDHB, VHL and MEN2A disease. Recurrence occurred in three (3%) patients with mutation absence. Multivariate analysis revealed that age ≤40 years and mutation presence were associated with increased risk of disease recurrence.
Conclusions
Genotypic characteristics strongly influence disease presentation and recurrence risk, which may occur more than 5 years after initial treatment. Routine genetic testing of PPGL patients is warranted given the high prevalence of mutations, allowing for prognostication and tailored follow-up. In the presence of germline mutations, follow-up should be life-long.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pheochromocytoma and paraganglioma (PPGL) are rare catecholamine-secreting tumours. Pheochromocytoma (PC) arises from the chromaffin cells of the adrenal medulla and is morphologically and functionally similar to paraganglioma (PG), which originates from extra-adrenal chromaffin cells in the sympathetic or parasympathetic paraganglia [1].
PPGL are associated with the highest known degree of heritability of all human neoplasms and may be associated with a mutation in any of the minimum 20 known susceptibility genes [2,3,4,5]. The most common mutations are of the succinate dehydrogenase (SDH) subunit genes, followed by VHL, RET and NF1 mutations [3]. The reported proportion of PPGL patients with germline mutations ranges from 7.5 to 53% [6, 7] and routine genetic testing is widely recommended in international clinical practice guidelines [4, 8].
In this study, we aim to describe the long-term outcomes of a consecutive series of PPGL patients treated at a tertiary referral centre in Australia and examine the relationship between genetic mutation status and clinical outcomes.
Materials and methods
All patients undergoing surgery for PPGL between March 2005 and December 2021 at a tertiary referral centre were identified from a prospectively maintained endocrine surgery database and included in the study. Perioperative data were collected and included patient demographic details, presenting symptoms, past medical history, family history, tumour location, imaging, biochemistry results, operative approach, tumour size, pathological details, immunohistochemical (IHC) staining results, genetic testing results, presence of recurrence, follow-up time, and mortality. Genetic testing was performed through the department of cancer genetics at our own institution. All patients who had undergone genetic testing at our institution were identified from this database. The genetic testing protocol at our institution evolved during the study period. Currently in 2022, we test all potentially implicated genes on a multigene exome panel, and this has been the approach for approximately 5 years. Prior to this, we followed the evidence-based algorithm described by Lenders et al., including SDHB, SDHD, SDHC, RET, VHL, NF1, TMEM127 and MAX genes [4], and if indicated by the clinical presentation, also analysed SDHA, FH, CDKN1B and SDHAF2 genes.
Patients had annual clinical follow-up with plasma metanephrines testing. Further imaging was performed in the event of recurrence of symptoms or elevated plasma metanephrines. Recurrence was defined as either radiologically or pathologically confirmed disease.
Statistical analysis was performed using SPSS (IBM Corp, Version 27.0. Armonk, NY: IBM Corp). Categorical variables were analysed using Fisher’s exact test and continuous variable means were analysed using the Student’s t test or Mann–Whitney U test. The Kruskal–Wallis test was used to compare medians between groups. The Kaplan–Meier method and log-rank test were used to compare disease-free survival between groups. Univariate and multivariate binomial logistic regression models were performed to identify independent predictors of disease-free survival. All p values were two-sided and values < 0.05 were considered statistically significant. Ethics approval was obtained from the Northern Sydney Local Health District (2020/ETH02787).
Results
A total of 140 patients, who underwent 155 procedures, met the inclusion criteria (Table 1). There were 72 (52%) females and 68 (48%) males with a mean (SD) age of 48.8 (16.7) years at diagnosis. For patients presenting with newly diagnosed PPGL, a minimally invasive surgical resection was performed in 93 (66%) cases, with 49 (35%) cases performed by a laparoscopic transperitoneal approach and 44 (31%) by a posterior retroperitoneoscopic approach. Patients presenting with recurrent disease were more commonly treated with an open procedure, with eight (30%) patients undergoing an anterior laparotomy. A total of seven (5%) deaths occurred during the follow-up period.
Phenotypic and tumour characteristics were analysed according to mutation status (Table 2). At initial presentation, patients with a germline mutation presented at a significantly younger age (SD), 38.5 (12.2) versus 53.6 (14.8) years (p < 0.001), and were more likely to have asymptomatic disease with lower preoperative levels of catecholamines at a median of 1.8 × ULN (IQR 0.5–6.0) versus 4.0 × ULN (IQR 1.8–9.7) (p = 0.011). At recurrent disease presentation, mutation carriers also presented at significantly younger age (SD) 40.8 (14.3 years). Mean tumour size was smaller among patients with germline mutations (33.3 vs 45.8 mm, p = 0.032), and patients were more likely to have bilateral disease (11% vs 0%, p = 0.002). Of the nine (6%) sympathetic paragangliomas that were localised to the Organ of Zuckerkandl, eight (89%) were associated with a germline mutation. Two patients presented with metastatic disease at initial diagnosis, both of whom had metastasis to bone and neither had a genetic mutation.
A total of 137 patients underwent IHC staining at the time of surgery and loss of the normal SDHB or SDHB and SDHA expression was observed in 12 (9%) and one (1%) cases, respectively, which were all associated with a germline mutation in one of the SDH genes.
The median overall follow-up time was 3.1 years (IQR 1.1–6.9) and median time to recurrence was 5.4 years (IQR 2.8–11.0). A total of 12 (9%) patients developed metastatic disease, of which four (33%) had synchronous disease (metastasis at or within six months of diagnosis) and eight (67%) had metachronous disease (metastasis development more than six months after diagnosis). Of the seven (5%) deaths recorded, five patients had developed metastatic disease. The date of death was available for four patients and median time to death was 5.8 years (IQR 0.9–10.6).
A total of 94 (67%) patients underwent genetic testing, who were identified by the availability of testing results within our medical records. A mutation detected in 36 (38%) of the patients tested. Of these, there were a total of 9 MEN2A, 7 SDHB, 6 VHL, 5 SDHD, 4 NF1, 2 TMEM127, 2 MEN2B and 1 SDHA gene mutations. All patients with positive mutation status tested positive to only one mutation, except for one patient who harboured pathogenic mutations for both MEN2A and SDHD. Of the 36 patients with positive mutation status, 10 patients had positive family history of adrenal or thyroid tumours, including six with MEN2 disease and four with PPGL. In the same cohort, 15 patients had positive past medical history of previous tumour diagnosis, of which eight had medullary thyroid cancer and ten had PPGL (three patients had both). All patients with a family history of MEN2 disease were confirmed to also have MEN2 disease themselves.
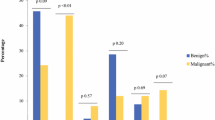
Overall, recurrence occurred in 21 (15%) patients and Table 3 describes disease course by mutation status. Among the 36 patients with a confirmed mutation, 14 (39%) developed disease recurrence. Recurrence was not observed in any patients with mutations in NF1 or TMEM127. Recurrence associated with germline mutation included four local recurrences, six s primary tumours, and five patients who developed metastatic disease. Of the 58 patients with a confirmed absence of germline mutation, three (5%) developed disease recurrence (Table 4); two had local recurrence and one developed metastatic recurrence. The remaining 46 patients did not undergo genetic testing and there were three metastatic recurrences and one recurrence of unknown nature in this cohort (recurrence rate 9%).
Kaplan–Meier estimates for disease-free survival stratified by mutation status are shown in Fig. 1a. Disease-free survival was significantly lower for patients with germline mutations. Kaplan–Meier estimates for metastatic disease-free survival are shown in Fig. 1b and did not demonstrate significant difference between mutation status groups.
Kaplan–Meier survival curves for patients with PPGL stratified according to mutation status. Curves are shown for disease-free survival (a) as well as for metastatic disease-free survival (b). Unknown mutation status was assumed as no mutation in (b) due to a large proportion of metastatic patients with unknown mutation status
Univariate analysis demonstrated that age ≤40 years (OR 9.227; 95% CI 2.832–30.066) and any germline mutation (OR 25.435; 95% CI 3.130–206.684) were significantly associated with reduced disease-free survival (Table 5). Asymptomatic presentation, preoperative catecholamine and metanephrines levels < 3 × ULN and tumour size is 40 mm all demonstrated a trend to reduced disease-free survival but did not reach statistical significance. Multivariate binomial regression analysis revealed that age ≤ 40 years (OR 9.668; 95% CI 1.077–86.774) and positive mutation status (OR 10.835; 95% CI 1.214–96.690) retained significance as independent predictors of recurrence.
Discussion
This 17-year retrospective cohort study of PPGL patients is the first to correlate genetic and follow-up data in an Australian population. We demonstrate that 38% of patients undergoing genetic testing have a confirmed germline mutation. At initial presentation, germline mutation carriers were more likely to present younger, with bilateral disease, asymptomatic disease, smaller tumours, lower preoperative catecholamines, and have a higher risk of disease recurrence. When examining recurrent disease, mutation carriers re-presented at younger age and were more likely to develop metastatic disease. Disease recurrence occurred in 21 (15%) of patients, 14 (67%) of whom were mutation carriers and seven (33%) were not or had not been tested. Independent predictors of disease recurrence on multivariate analysis included age at presentation ≤ 40 years and the presence of a germline mutation.
The prevalence of germline mutations in this cohort is consistent with previous studies, which report that at least one third of patients with clinically apparently sporadic disease have predisposing germline mutation [5, 9]. Of those with genetic disease, we confirm previously known associations with younger age at diagnosis, bilateral disease and higher recurrence risk [4, 10]. Patients with a family history or previously known genetic mutation are more likely to undergo imaging that leads to diagnosis before symptom development, which may explain why these patients also presented with more asymptomatic disease, smaller tumours and lower preoperative catecholamines.
The proportion of patients with recurrent disease in this cohort (15%) and the median time to recurrence of 5.4 years are comparable to other large cohort studies [11,12,13,14]. More than 50% of the patients with an SDHA or SDHD mutation or MEN2A/B syndromes experienced disease recurrence. In both the univariate and multivariate analysis, younger age and mutation status were strong predictors of disease recurrence, confirming previous reports [14,15,16,17]. Mutations in MEN2A, SDHB and VHL were the only genes associated with the development of metastatic disease, confirming previously known associations [7].
Three patients developed disease recurrence in the absence of a germline mutation. Two developed local recurrence, raising the possibility of capsular breach and tumour seeding at time of initial operation. The third patient developed metastatic disease, likely a result of aggressive tumour biology, suggested by a 120 mm tumour with a Pheochromocytoma of the Adrenal Gland Scaled Score (PASS) of 8. It has been suggested that PASS values greater than four indicate biologically aggressive tumour behaviour [18], however, there is high inter-observer and intra-observer variability associated with PASS and it is no longer routinely performed [19]. Contrary to previous studies, we did not find an association between tumour size and recurrence risk [14, 16].
Despite the increasing recognition of the impact of genotype on disease phenotype, the presenting characteristics of PPGL patients are not specific to mutation status. For example, in this cohort, there were three patients who were diagnosed with unilateral PC at age > 50 years (5% of patients diagnosed in this age category), without a family history of PPGL, who harboured a germline mutation. These findings support the position of the most recent clinical practice guidelines, that recommend germline testing be routinely performed for PPGL patients [4]. The results may have significant implications for family members and disease follow-up. Follow-up for PPGL patients should be at least 10 years and annual life-long follow-up is recommended for patients with a confirmed germline mutation [4, 9].
This study has several limitations. Due to the changing practices with respect to genetic testing and storage of data, not all patients underwent genetic testing. The retrospective nature of the study design impacted the completeness of the available data. Because the median follow-up time of 3.1 years was shorter than the time to recurrence, some recurrences may have been missed in our data collection. We also did not perform an overall survival analysis due to the low number of events in our cohort. The association between genotype and mortality represents an area of future research.
In conclusion, the presence of a germline mutation in PPGL patients is associated with extra-adrenal disease and higher risk of recurrence. The risk of recurrence may be stratified according to the specific mutation. Routine genetic testing of PPGL patients should be performed to allow enhanced prognostication as well as personalised treatment and follow-up pathways.
References
Mete O, Asa SL, Gill AJ et al (2022) Overview of the 2022 WHO classification of paragangliomas and pheochromocytomas. Endocr Pathol 33:90–114
Dahia PLM (2014) Pheochromocytoma and paraganglioma pathogenesis: learning from genetic heterogeneity. Nat Rev Cancer 14:108–119
Neumann HPH, Young WF, Eng C (2019) Pheochromocytoma and paraganglioma. NEJM 381:552–565
Lenders JWM, Duh Q-Y, Eisenhofer G et al (2014) Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocr 99:1915–1942
Favier J, Amar L, Gimenez-Roqueplo AP (2015) Paraganglioma and phaeochromocytoma: from genetics to personalized medicine. Nat Rev Endocrinol 11:101–111
Kim JH, Kim MJ, Kong SH et al (2022) Characteristics of germline mutations in Korean patients with pheochromocytoma/paraganglioma. J Med Genet 59:56–64
Liu Z, Ma J, Jimenez C et al (2021) Pheochromocytoma: a clinicopathologic and molecular study of 390 cases from a single center. Am J Surg Pathol 45:1155–1165
Fishbein L, Del Rivero J, Else T et al (2021) The North American neuroendocrine tumor society consensus guidelines for surveillance and management of metastatic and/or unresectable pheochromocytoma and paraganglioma. Pancreas 50:469–493
Plouin PF, Amar L, Dekkers OM et al (2016) European Society of Endocrinology Clinical Practice Guideline for long-term follow-up of patients operated on for a phaeochromocytoma or a paraganglioma. Eur J Endocrinol 174:G1–G10
Amar L, Bertherat J, Baudin E et al (2005) Genetic testing in pheochromocytoma or functional paraganglioma. J Clin Oncol 23:8812–8818
Press D, Akyuz M, Dural C et al (2014) Predictors of recurrence in pheochromocytoma. Surgery 156:1523–1527
Amar L, Servais A, Gimenez-Roqueplo A-P et al (2005) Year of diagnosis, features at presentation, and risk of recurrence in Patients with pheochromocytoma or secreting paraganglioma. J Clin Endocr 90:2110–2116
Gomella PT, Sanford TH, Pinto PA et al (2020) Long-term Functional and oncologic outcomes of partial adrenalectomy for pheochromocytoma. Urology 140:85–90
Dhir M, Li W, Hogg ME et al (2017) Clinical predictors of malignancy in patients with pheochromocytoma and paraganglioma. Ann Surg Oncol 24:3624–3630
Amar L, Baudin E, Burnichon N et al (2007) Succinate dehydrogenase B gene mutations predict survival in patients with malignant pheochromocytomas or paragangliomas. J Clin Endocr 92:3822–3828
Assadipour Y, Sadowski SM, Alimchandani M et al (2017) SDHB mutation status and tumor size but not tumor grade are important predictors of clinical outcome in pheochromocytoma and abdominal paraganglioma. Surgery 161:230–239
Parasiliti-Caprino M, Lucatello B, Lopez C et al (2020) Predictors of recurrence of pheochromocytoma and paraganglioma: a multicenter study in Piedmont, Italy. Hypertens Res 43:500–510
Thompson LDR (2002) Pheochromocytoma of the adrenal gland scaled score (pass) to separate benign from malignant neoplasms: a clinicopathologic and immunophenotypic study of 100 Cases. Am J Surg Pathol 26:551–566
Wu D, Tischler AS, Lloyd RV et al (2009) Observer variation in the application of the pheochromocytoma of the adrenal gland scaled score. Am J Surg Pathol 33:599–608
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, H., Papachristos, A.J., Gill, A.J. et al. Genotype–Phenotype Correlations and Clinical Outcomes in 155 Cases of Pheochromocytoma and Paraganglioma. World J Surg 47, 690–698 (2023). https://doi.org/10.1007/s00268-022-06862-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06862-w