Abstract
Background
We aimed to compare multifunctional irrigation-assisted vacuum drainage (MIVD), vacuum sealing drainage (VSD) and the Penrose drain in treating severe multi-space deep fascial infection (DFI) in head and neck.
Methods
A retrospective study was conducted on 113 patients who had suffered from severe multi-space DFI in head and neck and underwent surgical treatment. Patients were divided into the MIVD group, the VSD group, and the Penrose group according to their treatment. Baseline characteristics and clinical outcome data regarding infection control, clinicians’ workload, surgical procedure required, and cost were analyzed.
Results
Duration of antibiotic administration was significantly shorter using MIVD and VSD than Penrose drains (p = 0.002 with MIVD, p = 0.008 with VSD). Hospital stay in the MIVD group was shorter than the Penrose group (p = 0.034). Compared to the other two groups, more times of manual irrigation were needed in higher frequency in the Penrose group (p < 0.001). Longer Incision and more surgical operation were required in the VSD group than the other two groups (p < 0.001). The treatment cost in the VSD group was higher than the MIVD group (p = 0.045) and the Penrose group (p < 0.001).
Conclusions
In the treatment of severe multi-space DFI in head and neck, MIVD and VSD are superior to the Penrose drain in infection control and reduction in clinicians’ workload. Meanwhile, MIVD, with fewer surgical procedures required and less cost, seems to be a more promising method than VSD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Deep fascial infection (DFI) in head and neck is a difficult and lethal clinical problem referring to the infection in the potential spaces of maxillofacial and cervical region [1]. Mostly, these infections are secondary to odontogenic infections, such as carious mandibular molars. As bacteria and their byproduct penetrate through the surrounding tissue, the infection spreads rapidly among the potential spaces due to loose anatomical structure of soft tissues, causing symptoms such as swelling and erythema of involved skin, limited mouth opening and swallowing difficulty [2]. For infections in lower head and neck, the airway could even be obstructed [3,4,5]. Other life-threatening complications include osteomyelitis, descending mediastinitis, necrotizing fasciitis, sepsis and Lemierre's syndrome [6,7,8,9,10].
Surgical access to the abscess cavity should be established immediately to discharge the purulence, and effective drainage is indispensable afterward to prevent purulence re-accumulation [11]. Although the Penrose drain method remains the most acknowledged for DFI, clinicians have been seeking alternatives with higher efficiency [2, 12].
In recent years, negative pressure wound therapy has been proven effective for treating soft tissue damage and abdominal infection [13,14,15]. Clinicians also increasingly apply vacuum sealing drainage (VSD) to maxillofacial space infection treatment [16,17,18]. Three years ago, we designed a type of multifunctional irrigation-assisted vacuum drainage (MIVD) which combined vacuum drainage with continuous irrigation and applied it to treat multi-space DFI. It is assumed that MIVD and VSD have potential advantages over Penrose drain in which include but not limited to accelerating healing and reducing clinicians’ workload. However, no study has been conducted to prove it. The purpose of this study was therefore to compare the clinical effect of MIVD, VSD and the Penrose drain in treating severe multi-space DFI in head and neck, hoping to provide references for clinical practices.
Subjects and methods
This study was approved by Human Research Ethics Committee of Second Affiliated Hospital, Zhejiang University School of Medicine (No.20210887). We strictly followed the Declaration of Helsinki throughout the study.
Patients
We performed a retrospective study of patients diagnosed with multi-space DFI in head and neck from January 2018 to August 2021, at Department of Oral and Maxillofacial Surgery, Second Affiliated Hospital, Zhejiang University School of Medicine, P. R. China. Inclusion criteria were: (a) at least two infected spaces were found, (b) surgical drainage was performed and (c) the patient’s clinical data were complete. Patients were excluded if they met one of the following criteria: (a) they did not undergo surgery due to severe systemic diseases or refused surgical treatment, (b) they suffered from uncontrolled mental disorders or (c) they were diagnosed with infraorbital space infection or mild buccal space infection for which clinicians used simple intraoral incisions.
Before treatment, clinicians fully described MIVD, VSD and the Penrose drain objectively, including potential advantages and disadvantages. Patients made their choices after being fully informed and then were, according to the treatment method, divided into three groups: the MIVD group, the VSD group and the Penrose group. Informed consent was obtained.
Treatment methods
All patients were examined by contrast-enhanced computed tomography preoperatively. Incisions were designed to facilitate full exploration of the abscess and adequate drainage. The most frequently used incision was a submandibular incision, 1.5–2 cm below and parallel to the mandibular body’s lower edge. After careful incision through the skin and platysma muscle, clinicians used hemostats to make blunt dissection into the abscess cavity. A small amount of pus was collected for culture and drug sensitivity test before the abscess cavity was alternately irrigated with 1–3% hydrogen peroxide, 0.5% iodophor and saline (Fig. 1). Then, MIVD, VSD or the Penrose drain was applied according to the patient’s choice. All patients were prescribed antibiotics and monitored closely after the surgery. Additional surgeries were needed if there was no apparent decline or even an increase in the C-reactive protein (CRP) or white blood cell count (WBC) level for 3 consecutive days and abscess re-accumulation was further confirmed by contrast-enhanced computed tomography. The drainage device was removed when no purulence was observed in the drainage fluid, and CRP and WBC approached normal levels. Antibiotics administration ceased when CRP and WBC decreased to normal levels and previous symptoms of infection vanished, and the patient was discharged 1–2 days afterward if no symptom recurred.
The surgical procedure of treating deep fascial infection in head and neck. (a) A submandibular incision was designed. (b) After a careful incision through the skin and the platysma muscle, clinicians used hemostats to make blunt dissection into the abscess cavity. (c) Purulence was observed from the abscess cavity. (d) Thorough irrigation was performed
MIVD group
The MIVD device consisted of one silicone catheter (Suzhou McLean medical equipment co., Ltd., Jiangsu, China) and two PVC plastic catheters (Suzhou Jingle polymer medical apparatus co., Ltd., Jiangsu, China). The silicone catheter served as the drainage tube. Side holes were placed on the tube wall near its top, providing additional access for purulence. Two PVC plastic catheters were placed within the drainage tube: one served as the external irrigation with its top extending outwards from either a side hole or the top of the drainage tube, and the other as the internal irrigation tube with its top remained in the drainage tube (Fig. 2). After the MIVD device was put into the abscess cavity, the incision was closely sutured. The surgical area was covered with gauze and sealed with adhesive films (Fig. 3).
The structure of multifunctional irrigation-assisted vacuum drainage (MIVD). (a) The technical drawing of the MIVD device showed its structure: the drainage tube (a, 1), the internal irrigation tube (a,2), the external irrigation tube (a,3), and the side holes (a,4). (b) The MIVD system was composed of the drainage tube (b, the white arrow), the external irrigation tube (b, the blue arrow), and the internal irrigation tube (b, the black arrow)
Surgical pictures and imaging of MIVD. (a) MIVD was put into the abscess cavity. (b) The incision was closely sutured. (c) The surgical area was covered with gauze and sealed with adhesive films. (d–e) Contrast-enhanced computed tomography scan and its three-dimensional reconstructed image displayed the location of the MIVD device (inferior horizontal view) (d–e, the white arrow)
Then, the drainage tube was connected to a negative pressure system (150–200 kpa). The external irrigation tube was connected to large amounts of saline (125 ml/h, 3000 ml/a day) to achieve continuous irrigation. Clinicians manually infused 100 ml of saline through the internal irrigation tube to prevent potential tube blockage once thick purulence or debris was found remaining in the drainage tube. MIVD was directly extracted when no more drainage was needed.
VSD group
The VSD device (Smith &Nephew Medical Ltd., United Kingdom) consisted of foam dressing, a drainage tube and an internal irrigation tube. The drainage tube was embedded within the foam dressing. After the foam dressing was shaped to fit the abscess cavity, it was put into the abscess cavity together with the drainage tube and the irrigation tube. Then, the surgical area was sealed with adhesive films, leaving the drainage tube to be connected to a negative pressure system (150–200 kpa) (Fig. 4). When thick purulence or debris remained in the drainage tube, manual irrigation by clinicians (MIC) was performed through the irrigation tube to prevent tube blockage. Besides the common criteria for additional surgeries as described above, more surgeries were needed for the regular change of the VSD device every 5–7 days as well as the removal of the device when drainage ceased.
The structure and clinical pictures of vacuum sealing drainage (VSD). (a) The VSD system consisted of the foam dressing (a, the yellow arrow), the drainage tube (a, the white arrow), and the irrigation tube (a, the black arrow). The drainage tube was embedded in the foam dressing. (b) Surgical picture of the placement of VSD including the foam dressing (b, the yellow arrow), the drainage tube (b, the white arrow), and the irrigation tube (b, the black arrow). (c) The whole surgical area was sealed with adhesive films. (d–e) Contrast-enhanced computed tomography scan showing the abscess cavity (d, the white arrow) and VSD after it was put into the abscess cavity (e, the white arrow)
Penrose group
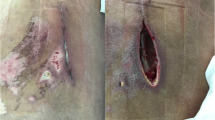
The Penrose drains in this study were manufactured by Well Lead medical co., Ltd., Guangzhou, China. After the drain was placed, the incision was sutured intermittently and covered with sterile gauze to protect the surgical area (Fig. 5). MIC was performed once the gauze was soaked through by the drainage fluid. The Penrose drain was eventually extracted directly, and the incision was left to heal without additional stitches.
The picture of the Penrose drain we used in this study and a patient from the Penrose group. (a) The Penrose drain. (b) The picture of a patient with the Penrose drain. (c–d) Contrast-enhanced computed tomography scan showing the abscess cavity (c, the white arrow) and the path of the Penrose drain into the abscess cavity (d, the white arrow)
Variables
Baseline characteristics and clinical outcome data were recorded from all patients. Baseline characteristics included age, sex, diabetes, other systemic diseases, tobacco use, etiology, the number of infected spaces and preoperative WBC and CRP. Clinical outcome data included variables related to infection control (duration of antibiotic administration and hospital stay), clinicians’ workload (times and frequency of MIC), surgical procedure required (times of operation and incision length) and hospitalization cost.
Statistical analysis
Categorical variables were presented as absolute numbers and numerical variables as mean ± standard deviation. Pearson Chi-square test was used to analyze categorical variables. For numerical variables, Analysis of Variance was used to compare those with normal distribution, and Kruskal–Wallis test for those with abnormal distribution. The statistical analysis was performed using SPSS 21.0. We considered p values less than 0.05 statistically significant.
Results
Patient’s characteristics
A total of 113 patients (72 males and 41 females) were included in this study, with the MIVD group 30 patients, the VSD group 31 patients and the Penrose group 52 patients. Baseline characteristics are summarized in Table 1. Involved spaces were submandibular space, pterygomandibular space, masseteric space, parapharyngeal space, submental space, buccal space, sublingual space and temporal space (Table 2). No significant difference was found among groups (p > 0.05).
Infection control
The duration of antibiotic administration in the MIVD group (11.83 ± 3.66 days) and the VSD group (12.58 ± 4.97 days) was shorter than that of the Penrose group (15.54 ± 5.09 days) (MIVD versus Penrose drains, p = 0.002; VSD versus Penrose drains, p = 0.008) (Table 3). No significant difference was observed between the MIVD group and the VSD group (p > 0.05).
Hospital stays of the MIVD group, the VSD group and the Penrose group were 13.60 ± 4.26 days, 15.53 ± 5.82 days and 16.40 ± 5.30 days. There was a significant reduction in the MIVD group compared to the Penrose group (p = 0.034). No significant difference was observed between the VSD group and the other groups (p > 0.05).
Clinician’s workload
In average, 21.88 ± 9.26 times of MIC with 1.32 ± 0.38 times/a day were performed in the Penrose group, significantly more and in higher frequency than those in the MIVD group (4.90 ± 1.63 times, 0.37 ± 0.10 times/a day) (p < 0.001) and those in the VSD group (5.29 ± 3.29 times, 0.34 ± 0.13 times/ a day) (p < 0.001). There was no significant difference between the MIVD group and the VSD group (p > 0.05) (Table 3).
Surgical procedure required
The Incision lengths of the MIVD group (5.00 ± 2.49 cm) and Penrose group (5.37 ± 3.48 cm) were significantly smaller than that of the VSD group (8.18 ± 2.66 cm) (p < 0.001). Differences between the MIVD group and the Penrose group were not significant (p > 0.05) (Table 3).
The numbers of operation of the MIVD group, the VSD group and the Penrose group were 1.13 ± 0.35 times, 2.58 ± 0.72 times and 1.25 ± 0.59 times, respectively. More operations were performed in the VSD group as compared with the other two groups (p < 0.001); however, no significant difference was found between the MIVD group and the Penrose group (p > 0.05) (Table 3).
Hospitalization cost
The hospitalization costs of the MIVD group, the VSD group and the Penrose group were 35,743.73 ± 20,087.72 CNY (Chinese currency), 56,144.14 ± 36,841.75 CNY and 33,137.33 ± 41,214.60 CNY (Table 3). The VSD group showed a higher cost as compared with the MIVD group (p = 0.045) and the Penrose group (p < 0.001). The difference between the MIVD group and the Penrose group was insignificant (p > 0.05).
Discussion
DFI in head and neck is a lethal problem that progresses rapidly unless managed properly. Prompt surgical management is imperative[19]. Penrose drains are the most frequently used form of drainage [2]. Clinicians have also applied negative pressure to drainage recently, which has been proved can not only timely remove purulence and necrotic tissues, but also promote wound healing by increasing microvascular blood flow [13, 20, 21]. In the meantime, continuous abscess irrigation effectively destroys the environment for microbiologic colonization due to ongoing bacterial reduction [22,23,24,25]. In this study, we compared the clinical effect of MIVD, VSD and the Penrose drain in treating severe multi-space DFI in head and neck. The results showed that although MIVD, VSD and the Penrose drain are all feasible, there were differences in infection control, clinicians’ workload, surgical procedure required and hospitalization cost, which is elaborated as follows.
Duration of antibiotic administration was found shorter in the MIVD group and VSD group than the Penrose group, demonstrating that both MIVD and VSD outperformed the Penrose drain in infection control. The hospital stay of patients with MIVD was significantly shorter than those with the Penrose drain, with no significant difference between VSD and the Penrose drain. In combination, these indicated that MIVD, with its continuous abscess irrigation, seemed to be a more effective method.
Both MIVD and VSD showed advantages over the Penrose drain in reducing clinician’s workload. MIC was usually necessary at least 1–2 times a day with the Penrose drain to prevent purulence re-accumulation. With MIVD and VSD, however, thanks to negative pressure continuous irrigation which played a major role in purulence evacuation, MIC was only needed once every other day to avoid device blockage. It should be noted that the reduction in MIC does not suggest a less clinical evaluation by clinicians. All patients were checked at least twice a day for any swelling of the surgical area, dressing status and functioning of the drainage devices.
In terms of surgical procedure, the VSD group had the longest incision in our study. Unlike MIVD and the Penrose drain, VSD depends on the foam dressing to absorb purulence. Incision length should be sufficient for the foam dressing to fully cover the abscess cavity. Additionally, the foam dressing needs to be changed several times to ensure effective drainage, and eventually be surgically removed. The VSD method, therefore, necessitates several times of surgical operations, consequently increasing the cost and trauma. MIVD and the Penrose drain, however, can be directly removed at the end of drainage, causing mild surgical trauma.
Although hospitalization costs varied from patient to patient, it was found the highest with VSD. This was largely due to the costly device and multiple surgical operations. Therefore, VSD may not be the best option for economically disadvantaged patients.
There are other aspects worth discussing. Firstly, incision design was more flexible with MIVD and VSD. The Penrose drain method is gravity-dependent, requiring the incision to be placed at the site lower to the infection. At the same time, potential injury to important nerves and vessels should be avoided. This made the incision design a dilemma in some cases. MIVD and VSD relied on negative pressure drainage systems, which effectively minimized functional damage when placing incisions. Secondly, the skin scars of the patients who underwent MIVD and VSD met the aesthetic requirement better than those with the Penrose drain. The incision with the Penrose drain usually led to pit-shaped scars due to second-intention healing. As for the other two groups, the incision was sutured closely in the first operation with MIVD, or sutured closely after device removal with VSD. Primary-intention healing of incision with these two methods led to minimum scar. But the VSD method usually had relatively long incision scar. Although the VSD method usually had relatively long scar, aesthetic differences were not specifically studied.
The limitations of this study are: (a) This was a non-randomized retrospective study. Though multivariable adjustment was used in statistical analysis, the possibility of residual confounding cannot be eliminated. (b) This study was conducted in a single center. The sample size might not be large enough, and the results might not be generalizable to all populations. In light of the limitations above, we have planned to conduct a multi-centered randomized controlled trial to further support the results of this study.
In conclusion, although all three methods are feasible for treating DFI, MIVD and VSD outperform the Penrose drain in accelerating infection control and reducing clinicians’ workload. Meanwhile, MIVD seems to be a more promising treatment method for DFI for its fewer surgical procedures and less hospitalization cost as compared with VSD.
References
Janecka IP (1979) Maxillofacial infections. Clin Plast Surg 6:553–573
James R, Hupp MRT, Edward E (2020) Contemporary oral and maxillofacial surgery. Mosby, Philadelphia, PA
Lim HK, Wang JM, Hung ST et al (2021) A dangerous cause of airway obstruction: deep neck infection. Signa Vitae 17:4–9
Jundt JS, Gutta R (2012) Characteristics and cost impact of severe odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol 114:558–566
Miyazaki R, Nakai Y, Houchi Y et al (2019) Brain abscess of a very elderly patient likely caused by maxillary osteomyelitis from odontogenic infection: a case report. J Oral Maxillofac Surg Med Pathol 31:118–120
Diamantis S, Giannakopoulos H, Chou J et al (2011) Descending necrotizing mediastinitis as a complication of odontogenic infection. Int J Surg Case Rep 2:65–67
Biasotto M, Pellis T, Cadenaro M et al (2004) Odontogenic infections and descending necrotising mediastinitis: case report and review of the literature. Int Dent J 54:97–102
Gore MR (2018) Odontogenic necrotizing fasciitis: a systematic review of the literature. BMC Ear Nose Throat Disord 18(1):1–7
Jevon P, Abdelrahman A, Pigadas N (2020) Management of odontogenic infections and sepsis: an update. Br Dent J 229:363–370
Gromov AL, Gubin MA, Ivanov SV et al (2018) New algorithms of diagnostics of heavy complications of acute odontogenic infection. Russian J Dent 22:82–87
Taub D, Yampolsky A, Diecidue R et al (2017) Controversies in the management of oral and maxillofacial infections. Oral Maxillofac Surg Clinics N Am 29:465–473
Furness J (2013) Contemporary oral and maxillofacial surgery 6th edition. Br Dent J 215(2):99
Azzopardi EA, Boyce DE, Dickson WA et al (2013) Application of topical negative pressure (vacuum-assisted closure) to split-thickness skin grafts: a structured evidence-based review. Ann Plast Surg 70:23–29
Armstrong DG, Lavery LA (2005) Negative pressure wound therapy after partial diabetic foot amputation: a multicentre, randomised controlled trial. Lancet 366:1704–1710
Li P-Y, Yang D, Liu D et al (2017) Reducing surgical site infection with negative-pressure wound therapy after open abdominal surgery: a prospective randomized controlled study. Scand J Surg 106:189–195
Cao J, Liu Z, Ma D et al (2020) Modified usage of negative pressure wound therapy for the management of severe deep fascial space infections in the head and neck. Infect Drug Resist 13:781–788
Qiu Y, Li Y, Gao B et al (2019) Therapeutic efficacy of vacuum sealing drainage-assisted irrigation in patients with severe multiple-space infections in the oral, maxillofacial and cervical regions. J Cranio Maxillofac Surg 47:837–841
Chopra K, Gowda AU, Morrow C et al (2016) The economic impact of closed-incision negative-pressure therapy in high-risk abdominal incisions: a cost-utility analysis. Plast Reconstr Surg 137:1284–1289
Keswani ES, Venkateshwar G (2019) Odontogenic maxillofacial space infections: a 5-year retrospective review in navi Mumbai. J Maxillofac Oral Surg 18:345–353
Anesäter E, Borgquist O, Torbrand C et al (2012) The use of a rigid disc to protect exposed structures in wounds treated with negative pressure wound therapy: effects on wound bed pressure and microvascular blood flow. Wound Repair Regen 20(4):611–616
Malmsjo M, Ingemansson R, Martin R et al (2009) Wound edge microvascular blood flow effects of negative pressure wound therapy using gauze or polyurethane foam. Ann Plast Surg 63:676–681
Thermann F, Wollert U (2014) Continuous irrigation as a therapeutic option for graft infections of the groin. World J Surg 38:2589–2596. https://doi.org/10.1007/s00268-014-2650-8
Hsieh H-S, Lee C-Y, Chang G-H et al (2021) innovative continuous wound irrigation approach for postoperative treatment of masticator space abscess. Ear Nose Throat J 80:014556132198944
Kim PJ, Attinger CE, Steinberg JS et al (2014) The impact of negative- pressure wound therapy with instillation compared with standard negative-pressure wound therapy: a retrospective, historical, cohort, controlled study. Plast Reconstr Surg 133:709–716
Brinkert D, Ali M, Naud M et al (2013) Negative pressure wound therapy with saline instillation: 131 patient case series. Int Wound J 10:56–60
Funding
This study was supported by the Fund of Basic Public Welfare Research Program of Zhejiang Province (LGF21H140002) and Joint Foundation for Key Program of Medical Health Science and Technology Project of Zhejiang Provincial Health Commission and National Health and Family Planning Commission of the People’s Republic of China (WKJ-ZJ-1718).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors reported no conflicts of interest.
Patient consent
Informed consent was obtained from all patients.
Ethics approval
This study was approved by the Human Research Ethics Committee of the Second Affiliated Hospital, Zhejiang University School of Medicine (No.20210887). We strictly followed the Declaration of Helsinki through all stages of this study. All authors comply with the journal’s ethical policies.
The final word count: 2500.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qian, Y., He, D., Qi, H. et al. Comparative Study of Multifunctional Irrigation-assisted Vacuum Drainage, Vacuum Sealing Drainage and the Penrose Drain in Treating Severe Multi-space Deep Fascial Infection in the Head and Neck. World J Surg 46, 2973–2983 (2022). https://doi.org/10.1007/s00268-022-06758-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06758-9