Abstract
Background
In under-resourced settings, general surgeons may be called upon to perform emergency operations within other specialties. Accordingly, we aimed to characterise patient outcomes after emergency neurosurgery performed by a general surgeon or general surgery trainee.
Methods
PubMed, Embase and the Cochrane Library were searched to 30 May 2021 for observational studies reporting outcomes after emergency neurosurgery performed by a general surgeon. Study screening, data extraction, and risk of bias using the Downs and Black checklist were performed in duplicate. Data on setting, operation undertaken, mortality rates and complications were extracted. Meta-analysis was planned but not possible due to heterogeneity. This study is registered with PROSPERO, CRD42021258097.
Results
From 632 records, 14 retrospective observational studies were included, covering a total sample of 1,988 operations. Four studies were from Australia, and the remaining 10 were, respectively, from 10 other countries. Most common operations performed were decompressive surgery with burr holes or craniectomy for head trauma and insertion of intracranial pressure monitors. Rural hospitals were the most common settings. Mortality rates for procedures performed by general surgeons at latest follow-up were heterogenous, ranging from 5% for evacuation of chronic subdural haematoma in Kenya to 81% in head injured patients in a Hong Kong study.
Conclusions
This is the first systematic review that synthesises the literature to characterise patient outcomes after neurosurgical operations performed by a general surgeon. Findings from this study may benefit global surgery performed in rural, remote, military or humanitarian settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In under resourced settings that lack specialised infrastructure, general surgeons may be called upon to perform operations outside the usual scope of modern general surgery. A globally important example is emergency neurosurgery in rural or remote settings. Survival in certain neurosurgical presentations, such as traumatic brain injury, depends on time-critical surgical intervention [1, 2]. In rural or remote locations, specialist neurosurgeons may not be available to perform such operations, leading to these interventions being carried out by a general surgeon without specialty-level neurosurgical training. Several case series exist discussing outcomes of patients having neurosurgical procedures performed under these conditions [3, 4]; however, the body of evidence on the topic has not been synthesised.
Though training in emergency neurotrauma is a part of the curriculum in general surgery for Australian trainees, particularly for those planning to practice in rural locations, [5] it is unlikely all graduating general surgeons have significant experience operating in these situations. The Neurosurgical Society of Australasia’s guidelines on management of neurotrauma in rural and remote locations call for burr hole evacuation of clots in the local setting where transfer time to a specialist neurosurgeon is over two hours and provide basic instructions on technique [6]. In developing countries and other settings unable support a resident neurosurgeon, general surgeons may even be required to perform elective neurosurgical procedures. [7] Accordingly, to inform global surgery, we performed a systematic review aiming to characterise the outcomes of patients undergoing a neurosurgical procedure performed by a general surgeon.
Methods
We undertook a systematic review of the literature according to a protocol registered a priori with PROSPERO (CRD42021258097) including the review question, search strategy, inclusion and exclusion criteria, and risk of bias assessment. Results were reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses 2020 (PRISMA 2020) reporting guidelines [8].
Search strategy, inclusion and exclusion criteria
A research question was formulated in accordance with the PICO structure. The population for our review comprised patients with neurosurgical conditions requiring urgent surgery in remote hospitals. The intervention was any emergency neurosurgery procedure performed by a general surgeon. Cranial and non-cranial neurosurgery was included. Operations carried out by general surgery trainees were included. The comparator, if reported, was performance of the same procedure by a specialist neurosurgeon or neurosurgery trainee. The primary outcome was in-hospital mortality. Secondary outcomes assessed included 30-day post-operative mortality, 90-day mortality, hospital length of stay, failure-to-rescue (composite outcome: post-operative death due to major surgical complications), post-operative complications and their severity, readmission and reoperations, and population of centre performing procedure. Studies were excluded if they only described elective operations or conditions. Only randomised controlled trials or cohort studies were considered for inclusion. Case reports, editorials and literature reviews were excluded due to the low levels of evidence they present.
PubMed (incorporating MEDLINE), Embase, and the Cochrane library were searched from database inception to the 30th of May 2021. No language restrictions were placed on searches. Search terms varied by database. PubMed was searched for (neurosurg* OR "neuro surg*" OR "neuro-surg*") AND ("general surg*")) AND (emergen* OR urgen* OR acute* OR remote* OR rural* OR regional*). EMBASE for neurosurgery AND 'general surgery' AND 'emergency surgery'. The Cochrane database was searched with MeSH heading ‘neurosurgery’ trees exploded. This was supplemented with several targeted searches of Google Scholar for rural neurosurgery, neurosurgery general surgeon, and brain injury general surgeon.
Data extraction
Title and abstract screening were performed independently by two reviewers (JNH and JMG). Studies were uploaded to an online tool to facilitate the screening process (Rayyan, Qatar Computing Research Institute, Ar-Rayyan, Qatar). The same two reviewers (JNH and JMG) then independently screened full texts of studies. Disagreements at any stage of screening were resolved by a third reviewer (CDO). Data extraction was performed by two reviewers using a pre-specified data extraction form (JNH and CDO). Data were extracted for country, study design, setting, population characteristics, intervention and pathology characteristics, comparator characteristics, mortality, complications, source of funding and reported conflicts of interest, methodological quality information, and other information relevant to the review questions.
Data analysis
Data were synthesised in both narrative and tabular formats. Methodological quality was assessed using the Downs and Black risk of bias checklist [9] for non-randomised studies by two authors (JMG and AS). Meta-analysis was planned and, however, was not conducted due to considerable heterogeneity within the included studies.
Results
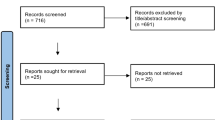
A total of 632 potentially relevant records were identified by the search strategy. A total of 448 records were drawn from PubMed, 107 from Embase and 77 from the Cochrane library. A total of 14 studies were eventually included in the review, all of which were retrospective observational studies. Targeted Google Scholar searches revealed no further studies. Figure 1 shows a flow chart of the study screening process. Table 1 shows the characteristics of included studies.
Global distribution
Four studies were from Australian settings. Two described the experience of the Royal Darwin Hospital [3, 10] and 2 discussed patients retrieved to South Australian hospitals [4, 11]. The resources for the general surgeon remaining studies were drawn from the Democratic Republic of Congo [12], Hong Kong [13], Kenya [14], Malaysia [15], New Zealand [16], Norway [17], the Philippines [18], Sweden [19], Tanzania [20] and the USA [21]. Most papers described a geographical setting where a patient would have to be retrieved significant distances to access a specialist neurosurgical service. Yue et al. however described a large Hong Kong hospital which after 1976 was joined by a neurosurgical specialist and prior to this relied on general surgeons [13]. Robertson et al. described a metropolitan hospital in the Philippines where a specialist neurosurgeon was available but due to shortage of neurosurgical workforce, could not provide universal coverage [18]. Likewise, Barber et al. described a metropolitan level 1 trauma centre in the USA where general surgery residents placed intra-cranial pressure monitors despite the availability of specialist neurosurgeons [21].
Interventions
In total, 1,988 interventions were included in our review with at least 1,673 performed by general surgeons. Some studies did not provide exact breakdowns of procedure description.
The main groups of procedures were CSF diversion for hydrocephalus (132 shunt, 32 EVD), evacuation of traumatic intracranial haematoma (329 operations) or insertion of an intracranial pressure monitor in the setting of trauma (546 operations). For studies in which the exact delineation of procedure performed was available, the most common procedure was ICP monitor placement (546 operations, 492 by general surgeons). Other common procedures were burr holes, evacuation of subdural and epidural haematoma, craniotomy, craniectomy and placement of ventriculoperitoneal shunt.
Mortality
Heterogeneity in reporting within the included studies made in-hospital, 30-day and 90-day mortality rates difficult to extract. The composite outcome of mortality at latest available follow-up for patients operated on by general surgeons is reported in Table 1. In studies where neurosurgeons also performed procedures and mortality was reported, this rate is also listed although care should be taken not to draw conclusions from comparison with mortality rates attributed to general surgeons. The lowest reported mortality rate for procedures performed by a general surgeon was 5%, which was for patients undergoing burr hole evacuation of chronic subdural haematoma [14]. The highest reported mortality rate for procedures performed by a general surgeon was 81%, for patients suffering a head injury prior to the introduction of specialist neurosurgical services in 1977 in a hospital in Hong Kong [13]. The pooled mortality rate for procedures carried out by a general surgeon across this review was 24%. Excluding studies published prior to the year 2000 results in a pooled mortality rate of 21%.
Complications
Complication rates, where reported, were rarely in detail. Multiple studies commented on patients initially operated on by a general surgeon requiring re-operation [4, 10, 11, 17]. In the Gilligan et al. series of patients retrieved to a South Australian trauma centre 2 of the 9 patients operated on in rural hospitals required repeat evacuation of haematoma by a neurosurgeon [4]. In an earlier series of patients with extradural haematoma treated at the same hospital, 2 of 6 patients undergoing a primary operation in a rural hospital by a general surgeon sustained haematoma that were “missed or inadequately evacuated by burr hole surgery.” [11] Wester et al. do not give reasons for the 2 reoperations required after retrieval in their cohort of patients treated by general surgeons in Norway [17]. Treacy et al. give a breakdown of patients requiring repeat surgery by diagnosis. 5/32 (16%) procedures performed for extradural haematoma, 13/94 (14%) for acute subdural haematoma, 17/78 (22%) for chronic subdural haematoma, 5/21 (24%) for intracerebral haemorrhage, 3/27 (11%) for hydrocephalus and 4/53 (8%) for other conditions were repeat operations [10]. In that cohort, repeat operations were performed by general surgeons as patients were not transferred to another hospital [10]. A later cohort of patients operated in the same hospital, reported by Luck et al., had 28 returns to theatre from a total of 195 operations [3]. Twelve of these were for acute subdural haematoma [3].
Risk of bias
The methodological quality of included studies as assessed by the Downs and Black risk of bias checklist is shown in both Table 1 (total score expressed as a percentage) and Table 2 (individual reviewer scores). The mean overall score was 18.3 ± 3.9 out of a possible 32 indicating fair quality.
Discussion
To our knowledge, this is the first systematic review examining outcomes of emergency neurosurgical procedures performed by general surgeons. Accordingly, findings may benefit global surgery performed in rural, remote, humanitarian, military or low-resource settings. Our findings are heterogenous and representative of the heterogeneity of circumstances, treated conditions and operations which were examined. 37 years elapsed between the publication of first and last studies included in this review during which time advances were made not only in neurosurgical techniques, training and equipment but also ambulance services, emergency medicine and neurocritical care. The studies are drawn from different countries with different healthcare systems and different systems of training for general and neurosurgeons. Caution should therefore be applied judiciously in comparing results between studies. For many patients also, outcome may be more strongly dependent on severity of injury or pathology than variations between surgeons. It is highly likely that the vast majority of neurosurgical procedures performed by general surgeons in low- and middle-income countries go unreported in the literature. This is emphasised by results of a survey published in 2020 finding “task-sharing” or “task-shifting” for neurosurgery occurred in at least 20 low- and middle-income countries, especially in emergency situations [22]. Nevertheless, this review provides the most up to date and complete summary of the literature. It can therefore be used as a preliminary benchmark to which future studies can refer to.
For ease of crude comparison with patients treated with modern neurosurgical and critical care techniques, one estimate of outcomes at one year after traumatic brain injury found a good recovery in 32%, moderate disability in 14%, severe disability in 24%, vegetative status in 1%, and death in 29% [23]. For patients with traumatic brain injury who undergo an operation, survival to hospital discharge can be expected in roughly 75% and to one year in roughly 67% [24].
The most common operations performed were for CSF diversion (EVD or VP shunt) or craniotomy/craniectomy or pressure monitoring for trauma (ICP monitor insertion, evacuation of haematoma). This is representative of the time critical nature of most emergency neurosurgical interventions. It is well recognised that good outcomes after evacuation of traumatic intra-cranial haematoma are time dependent [1, 2]. Hydrocephalus is another condition in which neurological state can precipitously decline, necessitating urgent operative intervention. An external ventricular drain in these circumstances is a relatively simple and potentially lifesaving intervention that can temporise patients before a definitive CSF diverting procedure can be performed [25]. In all of these situations, emergent intervention by a general surgeon may be lifesaving.
We are aware of at least one study published since our search was conducted which describes outcomes for patients undergoing a neurosurgical procedure by a non-specialist [26]. The same study surveyed regional and rural hospitals that provide surgical services in New South Wales and found less than half had basic equipment needed to deal with neurotrauma stocked [26]. Our findings emphasise the feasibility of emergency neurosurgical procedures being carried out by non-specialists. If this is supported by policy or guidelines, then this should be formalised, and correct equipment and training provided. If guidelines or training for the management of neurotrauma in rural or remote locations are updated, these should be informed by accurate knowledge of current outcomes reported in the literature. We include a short list of resources which the general surgeon may find useful in carrying out emergency neurosurgery in Table 3.
Of particular relevance to the Australian context are the reports drawn from the Royal Darwin Hospital [3, 10]. In a country such as Australia where such vast distances exist between specialist neurosurgeons, these studies demonstrate that an acceptable mortality rate can be achieved, at least a temporising measure in an emergency. The authors acknowledge that Royal Darwin Hospital now has a resident neurosurgical specialist, but the principles are still relevant to other centres without a specialist neurosurgeon or in the future if specialist neurosurgical support does not continue.
With the evolution of telehealth modalities enabling real-time audio-visual communication, rural hospitals and state- or country-wide health networks should consider implementing arrangements which would allow a consultant neurosurgeon to assist with both patient assessment and any potential operative intervention. The utility of such systems in treating patients with acute neurological conditions has been demonstrated with the widespread uptake of telehealth systems for stroke care [27]. Tele-mentoring by consultant neurosurgeons of general surgeons performing emergency neurosurgery may also be facilitated via simulation modalities such as augmented reality [28].
Our study has several limitations. Chief among them is the heterogeneity in settings, conditions and procedures examined which in turn leads to heterogeneity in outcomes. This heterogeneity, whilst not unexpected, precluded meta-analysis. There may be little that can be concluded from comparing mortality rates between studies for example and within one study this overall mortality rate may represent several different conditions and operations pooled together. It is possible other studies exist which should have been included, and as already mentioned, it is likely that many procedures go unreported in the literature entirely which introduces a bias into our results. Though the quality of included studies was fair as assessed by the Downs and Black checklist, all studies were retrospectively undertaken with all the attendant limitations of such a study design. The quality of evidence on this topic could be enhanced by conducting a prospective study, which could be linked to existing trauma databases.
Emergency neurosurgery performed by general surgeons can be lifesaving for patients with time-critical neurosurgical conditions in under-resourced settings. This study provides the first synthesis of the global literature on this topic to characterise patient outcomes in these clinical scenarios. Future research may benefit from strong studies investigating interventions, such as tele-mentoring, by which surgical systems can facilitate surgeon competence and information in these situations.
References
Seelig JM, Greenberg RP, Becker DP, Miller JD, Choi SC (1981) Reversible brain-stem dysfunction following acute traumatic subdural hematoma: a clinical and electrophysiological study. J Neurosurg 55:516–523
Mendelow AD, Karmi MZ, Paul KS, Fuller GA, Gillingham FJ (1979) Extradural haematoma: effect of delayed treatment. Br Med J 1:1240–1242
Luck T, Treacy PJ, Mathieson M, Sandilands J, Weidlich S, Read D (2015) Emergency neurosurgery in Darwin: still the generalist surgeons’ responsibility. ANZ J Surg 85:610–614
Gilligan J, Reilly P, Pearce A, Taylor D (2017) Management of acute traumatic intracranial haematoma in rural and remote areas of Australia. ANZ J Surg 87:80–85
General Surgeons Australia (2016) General surgery curriculum: Trauma. Melbourne.
Neurosurgical Society of Australasia (2009) The management of acute Neurotrauma in rural and remote locations. Melbourne
Park BE (2016) Surgical treatment of degenerative lumbar spine disease in rural sub-saharan Africa: A retrospective study of 450 cases and its future implications. World Neurosurg 87:417–421
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52:377–384
Treacy PJ, Reilly P, Brophy B (2005) Emergency neurosurgery by general surgeons at a remote major hospital. ANZ J Surg 75:852–857
Simpson DA, Heyworth JS, McLean AJ, Gilligan JE, North JB (1988) Extradural haemorrhage: strategies for management in remote places. Injury 19:307–312
Cairo SB, Agyei J, Nyavandu K, Rothstein DH, Kalisya LM (2018) Neurosurgical management of hydrocephalus by a general surgeon in an extremely low resource setting: initial experience in North Kivu province of Eastern Democratic Republic of Congo. Pediatr Surg Int 34:467–473
Yue CP, Mann KS, Ong GB (1983) Acute subdural haematoma: better results with neurosurgeons than general surgeons. Injury 14:489–492
Kanyi JK, Ogada TV, Oloo MJ, Parker RK (2018) Burr-hole craniostomy for chronic subdural hematomas by general surgeons in rural kenya. World J Surg 42:40–45
Visvanathan R (1994) Severe head injury management in a general surgical department. Aust N Z J Surg 64:527–529
Havill JH, Sleigh J (1998) Management and outcomes of patients with brain trauma in a tertiary referral trauma hospital without neurosurgeons on site. Anaesth Intensive Care 26:642–647
Wester T, Fevang LT, Wester K (1999) Decompressive surgery in acute head injuries: where should it be performed? J Trauma 46:914–919
Robertson FC, Briones R, Mekary RA et al (2020) Task-sharing for emergency neurosurgery: a retrospective cohort study in the philippines. World Neurosurg X. 6:100058
Fischerstrom A, Nyholm L, Lewen A, Enblad P (2014) Acute neurosurgery for traumatic brain injury by general surgeons in Swedish county hospitals: a regional study. Acta Neurochir (Wien) 156:177–185
Attebery JE, Mayegga E, Louis RG, Chard R, Kinasha A, Ellegala DB (2010) Initial audit of a basic and emergency neurosurgical training program in rural Tanzania. World Neurosurg 73:290–295
Barber MA, Helmer SD, Morgan JT, Haan JM (2012) Placement of intracranial pressure monitors by non-neurosurgeons: excellent outcomes can be achieved. J Trauma Acute Care Surg 73:558–563
Robertson FC, Esene IN, Kolias AG et al (2020) Task-shifting and task-sharing in neurosurgery: an international survey of current practices in low- and middle-income countries. World Neurosurg X 6:100059
Jiang JY, Gao GY, Li WP, Yu MK, Zhu C (2002) Early indicators of prognosis in 846 cases of severe traumatic brain injury. J Neurotrauma 19:869–874
Shi HY, Hwang SL, Lee IC, Chen IT, Lee KT, Lin CL (2014) Trends and outcome predictors after traumatic brain injury surgery: a nationwide population-based study in Taiwan. J Neurosurg 121:1323–1330
Sumer MM, Acikgoz B, Akpinar G (2002) External ventricular drainage for acute obstructive hydrocephalus developing following spontaneous intracerebral haemorrhages. Neurol Sci 23:29–33
Yusof Vessey J, Shivapathasundram G, Francis N, Sheridan M (2021) Is neurotrauma training in rural New South Wales still required following the implementation of the New South Wales State Trauma Plan? ANZ J Surg 91(9):1881–1885
Bladin CF, Kim J, Bagot KL et al (2020) Improving acute stroke care in regional hospitals: clinical evaluation of the victorian stroke telemedicine program. Med J Aust 212:371–377
Kovoor JG, Gupta AK, Gladman MA (2021) Validity and effectiveness of augmented reality in surgical education: a systematic review. Surgery 170:88–98
World Health Organization. (2003) Surgical care at the district hospital: World Health Organization
Giannou C, Baldan M (2010) War surgery, vol 1. The Royal College of Surgeons of England
Rosenfeld JV, Watters DA (2001) Neurosurgery in the tropics
Boffard KD (2011) Manual of definitive surgical trauma care 3E: CRC Press
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hewitt, J.N., Ovenden, C.D., Glynatsis, J.M. et al. Emergency Neurosurgery Performed by General Surgeons: A Systematic Review. World J Surg 46, 347–355 (2022). https://doi.org/10.1007/s00268-021-06363-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06363-2