Abstract
Background
Esophageal duplication cysts are a rare congenital cystic malformation from faulty intrauterine recanalization of the esophagus during the 4-8th weeks of development. They account for 20% of all gastrointestinal duplication cysts and commonly involve the distal esophagus. Presenting symptoms may be related to size and location.
Materials and Methods
Following the PRISMA guidelines, a systematic review was performed by searching published literature in various databases. Data from 97 reported case reports were pooled to present a descriptive and statistical analysis.
Results
Patient population was composed of 51(52.5%) males and 46 (47.5%) females, and mean ages was 42.3 years (18–77). Distal cysts were the most prevalent. Seventy-nine (81.4%) patients were symptomatic; common symptoms included dysphagia, chest pain, cough and weight loss. Fifteen (15.5%) patients were treated conservatively and 75 (84.5%) by surgical treatment, among them thoracotomy in 30 (30.9%) patients and VATS in 17 (17.5%) patients. Mean length of hospital stay was 8.6 days (range: 1–26 days). One fatality was registered. Location, unlike size, was not found to influence presenting symptoms or treatment employed. Frequency of conservative treatment was not significantly different between symptomatic and asymptomatic patients. Open approaches were associated with longer stays than their minimally invasive counterparts.
Conclusion
Esophageal duplication cysts remain rare in adults and are frequently located in the distal esophagus. Larger cysts are more likely to cause symptoms. Various surgical techniques may successfully be employed in the treatment of this pathology. Minimally invasive procedures have a shorter hospital stay.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Esophageal duplication cysts (EDCs) are congenital malformations of the posterior primitive foregut and often within the thoracic esophagus. EDC is a congenital cystic malformation of the alimentary tract consisting of a duplication of the segment to which it is adjacent, being the result of faulty intrauterine recanalization of the esophagus, during the fourth to eighth week of embryonic development [1]. EDC are the third most common esophageal mass after leiomyoma and benign polyps, accounting for 0.5% to 2.5% of all esophageal tumors. They have a male-to-female ratio of 2:1, and they are more commonly found in the distal esophagus [2]. Autopsy studies have shown a prevalence of approximately 1:4500 and esophageal duplications occur even less frequently, 1:8200. They account for 20% of all the gastrointestinal duplication cysts. Less than 7% of EDCs remain asymptomatic until adolescences. EDCs most frequently involve the distal esophagus and may generate a wide group of symptoms depending on their size and location [3]. These symptoms may include dysphagia, respiratory distress, failure to thrive and retrosternal pain [4]. Cysts may cause various complications such as esophageal stenosis, respiratory system compression, rupture, infarction or malignancy [5]. Diagnosis is usually made by an imaging study: furthermore, total surgical or endoscopic excision represents the treatment of choice for these cysts [4, 6].
A few case reports have been reported in the literature, with only one series consisting of 4 asymptomatic patients, which were no treated [4]. Herein, we present a systematic review of all adult patients that have been reported in the literature, to our knowledge, with EDC, describing demographics, form of presentation, treatment and perioperative outcomes. Furthermore, this review aims to summarize and analyze published data to determine possible relations in location with presentation, diagnosis, treatment and outcomes.
Materials and methods
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we searched for published manuscripts using the Mesh terms “esophageal duplication cyst,” “enteric cyst” “esophageal cyst” in PubMed, Google Scholar, Scopus, NCBI databases, using snowballing method as well as a manual search to avoid losing reports, with no language restrictions. Investigators were not blinded to the journal, author or institutions. We identified potentially eligible studies by examining titles and abstracts. Full articles were obtained to assess eligibility criteria before the critical appraisal. Data extraction of every case report or case series was performed and analyzed by all investigators to ensure quality data extraction. The primary analysis of adult patients with EDC included variables such as gender, age, comorbidities, main symptom, time of symptoms to diagnosis, image study, size, location, treatment, complications, length of hospital stayed and mortality. For those cases with a noticed successful treatment without complications, we assumed a favorable outcome.
We limited inclusion to published material of adult patients and of real EDC diagnosed by histopathologic examination. Studies whose histopathologic analysis was anything other than EDC were discarded. Studies not providing histopathologic analysis, but corresponding image diagnoses were included. We excluded any cyst or tumor mimicking EDC, patients who did not meet the established criteria for diagnosing an EDC, patients < 18 years old.
Palmer's pathologic criteria are useful for diagnosing this type of cyst; these criteria include (1) attachment to the esophageal wall; (2) presence of gastrointestinal tract epithelium; non-keratinizing squamous or ciliated columnar epithelium; and (3) existence of two layers of smooth muscle. [7] We excluded case reports that initially had a diagnosis of EDC, but final pathology did not meet Palmer's criteria, thus classifying them as bronchogenic cysts or other types of cysts.
A narrative description of findings was performed, and statistical analysis was carried out using the SPSS Statistics version 25 (IBM Corp., Armonk, USA) software. No assessment for risk of bias was performed. Kolmogorov–Smirnov test of normality was performed before data analysis to assess for normality of distribution. Testing of parametric variables was performed using Student T and ANOVA with Tukey's post hoc tests when applicable. Nonparametric testing was performed through Mann–Whitney U and Kruskall–Wallis. Nominal and ordinal variables were tested using Chi-square or Fisher’s exact where applicable. Continuous variables were expressed as means or medians when appropriate. Ordinal and nominal variables were expressed as frequencies and percentages. A P value< 0.05 was considered statistically significant.
All procedures performed in studies involving human participants were in accordance with the ethical standards of Tecnologico de Monterrey ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Results
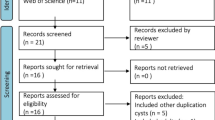
We carried out the systematic review until May 10, 2020. Shown in Fig. 1 is the flowchart, including the four phases of PRISMA, and obtained, eliminated and excluded duplicated records. In the identification phase, we collected 182 records from PubMed, Google Scholar and Scopus. We excluded a total of 104 of this first query. Due to incomplete information, no access to full text and pediatric patients, the pathology report came out inconclusive or did not include such information.
Remaining were 78 full-text articles that were assessed entirely for eligibility, which had basic and extended terms. We included another 14 articles from the NCBI database. We extracted evidence for this review, a total of 92 case reports and two case series, with the first case report published in 1973.
Patients characteristics, demographics, image studies and treatment
A total of 97 cases from 92 publications were included. The population was composed of 51 (52.5%) males and 46 (47.5%) females. Mean age was 42.3 years (range: 18 to 77 years). Cysts were located at various levels of the esophagus, being most frequently encountered in the distal third, middle third and proximal third of the esophagus, in 82 (84.5%), 10 (10.3%) and 5 (5.2%) of the cases, respectively (Fig. 2). Seventy-nine (81.4%) patients were symptomatic and 18 (18.5%) asymptomatic. Common symptoms included dysphagia, chest pain, cough and weight loss, which were presented in 50 (51.5%), 29 (29.8%), 5 (5.1%) and 15 (15.4%) of the cases, respectively. Six (6.1%) patients presented fever. Mean time from initial symptoms until diagnosis was 17.3 months (range 1 to 243.3 months). Several diagnostic studies were used, such as esophagogram in 72 (74.2%) patients, endoscopy in 49 (50.5%) patients, endoscopic ultrasound (EUS) in 54 (55.6%) patients, magnetic resonance imaging (MRI) in 16 (16.4%) patients, computed tomography in 77 (79.3%) patients and chest X-ray in 26 (26.8%) patients. Fine needle aspiration biopsy was performed in 17 (17.5%) patients.
a Coronal CT section illustrating complex loculated proximal oesophageal duplication cyst. Reprinted with permission. Prasai et al. Eur Arch Otorhinolaryngol. 2014;2. b Sagittal CT scan showing a cyst in the middle esophagus. Reprinted with permission. Espeso et al. Eur Arch Otorhinolaryngol. 2007; 264: 1357–60. c Sagittal CT scan showing a cyst in the distal esophagus. Reprinted with permission. Markinez-Gordobil et al. Cir Esp. 2011;89: 408–410
In regard to the treatment employed, 15 (15.5%) patients were managed conservatively (antibiotics, percutaneous drainage or expectant) and 75 (84.5%) by surgical treatment. The most common therapeutic choice was thoracotomy in 30 (30.9%) patients, followed by video-assisted thoracoscopic surgery (VATS) in 17 (17.5%) patients. Endoscopic primary excision or aspiration of the cyst was performed in 12 (12.4%) cases, and a laparoscopic approach was employed in 11 (11.3%) of the cases. Laparotomy was done in five (5.2%) cases. In seven (7.2%) patients, the surgical method was not specified. Figure 3 displays trends in the treatment during the years.
Mean length of hospital stayed (LOS) was 8.6 days (range: 1 to 26 days). There were seven spontaneous cyst complications, including two cyst infections, one rupture of the cyst, one hemorrhage from the cyst, one ischemic perforation of the cyst, one hematoma, one rupture of esophageal muscle, one postoperative esophagus leakage and one fatality.
Analysis by symptomatology and cyst location
Grouping patient data in symptomatic and asymptomatic and subsequent analysis revealed no significant differences in symptoms in gender, age or location. However symptomatic patients had larger cystic dimensions 3.70 ± 1.58 vs 5.81 ± 3.03 (P = 0.009). Group analysis by location revealed no differences in demographic data such as gender or age, nor morphological characteristics or symptoms (Table 1). Symptomatic cysts more frequently underwent surgical management (Table 2).
Analysis by Treatment Employed
Analyzing patient characteristics and outcomes of patients grouped into treatment type revealed no differences of statistical significance in age and location or certain cystic dimensions. Furthermore, when analyzing separately length of hospital stay between conventional method or minimally invasive surgery, differences were nonsignificant. There was only one postoperative complication and one mortality. These findings are summarized in Table 3.
Discussion
EDC are the second most common duplication cysts of the digestive tract after their ileal equivalents, and these types of cysts are rarely seen in adults [2, 7, 8]. In this systematic review, almost all of the patients had EDC in the distal part of the esophagus; nevertheless, the male-to-female ratio was nearly 1:1.
While the current literature suggests most cysts are asymptomatic, our review found the opposite, with 81% symptomatic cases, probably from reporting bias in that symptomatic cases are more likely to be diagnosed and treated, and thus most likely to be reported. In this review, 18% of patients were asymptomatic upon diagnosis, and most of these diagnoses were incidentally made when performing an imaging study. Some patients who underwent routine checkup with endoscopy [4, 9, 10] or chest X-ray [11] were diagnosed with an incidental mass. For other patients in whom a CT scan was performed for various reasons such as renal transplant protocol [6], urolithiasis [12], lumbar back pain [13], staging breast cancer [14] and pneumonia [15], incidental masses were also detected. For some other patients who underwent cardiac imaging studies such as cardiac MRI [16], echocardiography [17] or carotid ultrasound [18], masses in their esophagus were incidentally encountered.
EDC may cause symptoms like chest pain and dysphagia, because of direct compression of the esophagus. Moreover, patients may experience weight loss because of a lack of food intake due to fear of experiencing dysphagia [19,20,21,22,23,24,25,26]. If the cyst is not promptly diagnosed, it might cause severe complications such as perforation [20, 27,28,29,30], mild bleeding [31, 32] intramural hematoma [33] and massive hemorrhage into the pleura space [34]. Infection is another known complication of EDC [35,36,37,38]. Agarwal et al. [39] and Tomar et al. [40] reported two young adults who presented with an EDC masquerading pericarditis and post-infective bronchiectasis, respectively. Nasr et al. [27] reported a 30-year-old man with an EDC penetrating the thorax causing a pyothorax, and the final specimen revealed an EDC along with a squamous cell carcinoma. Malignant transformation within these cysts is extremely rare and has been rarely reported before. Two 61-year-old patients presented with dysphagia and significant weight loss, with a proximal and distal mass in the esophagus; on the former, biopsies were taken revealing a duplication cyst with squamous cell carcinoma, so chemo-radiation was given with complete response [41], and on the latter, a complete surgical resection by thoracotomy was achieved, with the same histopathologic diagnosis [8].
Several ways of resecting the cyst have been reported, including thoracotomy, VATS, abdominal approach or more recently endoscopic resection. In this systematic review, we observed patients with cysts in the distal [22, 42,43,44,45] and middle esophagus [21] who underwent endoscopic resections. In one patient, a VATS with an endoscopic approach was made for treating a bleeding caused during the surgical excision [46]. Laparotomy was performed in six patients with distal cysts [10, 26, 47, 48].
A laparoscopic approach was performed in 11 patients; most of them used intraoperative endoscopies to monitor the integrity of the esophageal walls [7, 13, 14, 24, 49,50,51,52]. One patient with an EDC at the lower left cervical region underwent surgical excision of the mass, through a “Y” cervical incision, completely enucleating the tumor, with a favorable postoperative evolution, without any complication [23].
A thoracic approach was chosen in half of the patients, being more frequently employed a conventional method [19, 30, 33, 34, 53,54,55,56,57]. There are known advantages associated with the minimally invasive approach, such as a short hospital stay, minimal postoperative discomfort, fast recovery and return to regular activities [11, 15, 17, 58,59,60,61,62].
Endoscopic therapeutic approaches were employed in 12 patients, of which 4 underwent endoscopic drainage [63,64,65]. Eight patients underwent endoscopic resection, in one of them a fully covered, lumen-apposing, metal stent was inserted transluminally into the lesion, creating an endoscopic cystogastrostomy to facilitate drainage [66]. In one patient, a cervical EDC drainage was made by a percutaneous ultrasound-guided method. [67]. On two patients, antibiotics were only given, and ten patients were expectantly managed [40, 68]. While we cannot draw strong recommendations when using an endoscopic approach for treating this disease, we can demonstrate that most patients who underwent endoscopic treatment had EDC in the distal third of the esophagus, with a mean size of 5.3 cm × 4.7 cm × 4.7 cm; however, we hope that this review allows for future higher-quality studies by pointing out new questions in treatment.
One postoperative complication was reported in a 35-year-old woman, who developed chest pain and fever on her POD 10. A swallow study revealed a leakage into the posterior mediastinum, which was successfully resolved by endoscopy applying metallic clips [35]. One 30-year-old male patient died in whom a thoracotomy was performed for resecting an EDC. On POD 5, the patient developed respiratory distress, and a chest CT scan showed large pleural effusion. The patient was reoperated, draining a pyothorax. The patient developed a septic shock and died on POD 10 [27].
Limitations of our study include the short number of patients, the long study period, which entails different imaging and treatment modalities. Another limitation is the nature of the case reports, and even though we advocate for the use of CARE guidelines to improve the quality of them, a potential loss of reports from search engines is possible. Another important limitation in our study is that our database was built using published cases; thus, publication bias may be present in cases with suboptimal outcomes or managed conservatively that were not reported/published. Furthermore, symptomatic patients are most likely to be worked up and treated, while asymptomatic patients may rely on an incidental diagnosis. Efforts must be made to estimate the prevalence and presenting symptoms of this disease.
In conclusion, this is the only review to date of EDC in adult patients, describing, to our knowledge, all published cases in the medical literature. EDC is more frequently found in the distal third of the esophagus. In this systematic review, most of the patient presented symptoms, being chest pain and dysphagia the most common of them. CT scan was the image modality more frequently employed in all the cases; nevertheless, some other image studies may be done to achieve the diagnosis, such as endoscopy or MRI. There are several ways to treat EDCs, and treatment should be individualized to each patient.
References
Duan X, Cui Y, He Y, Xu S (2018) Acute attack of recurrent esophageal duplication cyst in an adult : case report and literature review. J Thorac Dis 10(5):335–339
Bagheri R, Mohammad A, Asnaashari H (2015) Esophageal duplication cyst . Asian Cardiovasc Thorac Ann 23(3):332–334
Aldrink JH, Kenney BD (2011) Laparoscopic excision of an esophageal duplication cyst. Surg Laparosc Endosc Percutan Tech 21:e280–e283
Wiechowska-kozłowska A, Wunsch E, Majewski M, Milkiewicz P (2012) Esophageal duplication cysts : endosonographic findings in asymptomatic patients. World J Gastroenterol 18(11):1270–1272
Takemura M, Yoshida K, Morimura K (2011) Thoracoscopic resection of thoracic esophageal duplication cyst containing ectopic pancreatic tissue in adult. J Cardiothorac Surg 6:3–6
Shiozaki A, Fujiwara H, Murayama Y et al (2012) Hand-assisted laparoscopic transhiatal approach for mediastinal esophageal duplication cyst resection. Esophagus 9:247–251
Sebastianus P, Castelijns S, Woensdregt K et al (2014) Intra-abdominal esophageal duplication cyst : a case report and review of the literature. World J Gastrointest Surg 6(6):112–116
Dai Z-J, Kang H-F, Lin S et al (2013) Esophageal cancer with esophageal duplication cyst. Ann Thorac Surg 96:15–16
Mori M, Shuto K, Hirano A et al (2019) Laparoscopic surgery for an esophageal duplication cyst using a near-infrared indocyanine green fluorescence system : a case report. Asian J Endosc Surg 13(2):211–214
Kim YW, Il ST, Shim HS et al (2005) Intra-abdominal esophageal duplication cyst in an adult. Yonsei Med J 46(6):859–861
Al-riyami S, Al-sawafi Y (2015) True Intramural esophageal duplication cyst. Oman Med J 30(6):469–472
Angulo-Molina D, Salceda-Otero JC, Lozoya-González D et al (2012) Quiste de duplicación esofágica : un hallazgo poco común. Rev Gastroenterol México 77(3):141–2. https://doi.org/10.1016/j.rgmx.2012.04.006
Nelms CD, White R, Matthews BD et al (2002) Thoracoabdominal esophageal duplication cyst. Am Coll Surg 7515(02):674–675
Kin K, Iwase K, Higaki J et al (2003) Laparoscopic resection of intra-abdominal esophageal duplication cyst. Surg Laparosc Endosc Percutan Tech 13(3):208–211
Kang CU, Cho DG, Do CK et al (2008) Thoracoscopic stapled resection of multiple esophageal duplication cysts with different pathological findings. Eur J Cardio-thoracic Surg 34:216–218
Tsang J, Bowen FW, Dadhania M et al (2014) Esophageal duplication cyst : a rare cause of atrial fibrillation in a young adult patient. J Cardiovasc Electrophysiol 25(11):1259–1261
Accadia M, Ascione L, De MM et al (2004) Esophageal duplication cyst : a challenging diagnosis of a paracardiac mass. Ecocardiography 21(6):551–554
Gill AS, Long JL (2013) Transnasal esophagoscopy and the diagnosis of a mediastinal foregut duplication cyst. ENT-Ear, Nose Throat J 92(8):332–4
Pianzola HM, Otino A, Canestri M et al (2001) Cystic duplication of the esophagus. Acta Gastroenterol Latinoam 31(4):333–338
Herbella FAM, Tedesco P, Muthusamy R et al (2006) Thoracoscopic resection of esophageal duplication cysts. Dis Esophagus 19:132–134
Nishikawa J, Nagao M, Ogawa R et al (2017) Endoscopic treatment of an esophageal duplication cyst. Endoscopy 49:107–108
Joyce AM, Zhang PJ, Kochman ML (2006) Complete endoscopic resection of an esophageal duplication cyst (with video ). Gastrointest Endosc 64(2):288–289
Grozavu C, Iliaæ M, Pantile D (2015) Cervico-mediastinal Esophageal duplication cyst - case presentation. Chirugia 110(3):275–281
Bhamidipati C, Smeds M, Dexter E et al (2013) Laparoscopic excision of gastric mass yields intra-abdominal esophageal duplication cyst. Thorac Cardiovasc Surg 61(6):502–505
Sotoudehmanesh R, Behgam-Shadmehr M, Jamali R (2009) What is your diagnosis? Esophageal Duplication Cyst Arch Iran Med 12(4):4–5
Rico-morales MM, Ferrer-márquez M, Belda-lozano R et al (2007) Quiste por duplicación esofágica como causa inusual de disfagia en el adulto. Cir Esp 82(6):361–363
Nasr B, Derbel F, Ben MM et al (2015) Complicated esophagal duplication cyst in adult : a case report and review of the litterature. J Gastroenterol Hepatol Res 4(10):1801–1804
Mansard MJ, Rao U, Rebala P et al (2011) Esophageal duplication cyst masquerading as a stromal tumor in an adult. Indian J Surg 73(6):441–443
Neo EL, Watson DI, Bessell JR (2004) Acute ruptured esophageal duplication cyst. Dis Esophagus 17:109–111
Nakahara K, Fujii Y, Miyoshi S (1990) Acute symptoms due to a huge duplication cyst ruptured into the esophagus. Ann Thorac Surg 50(2):309–11. https://doi.org/10.1016/0003-4975(90)90761-T
Pisello F, Geraci G, Arnone E et al (2009) Acute onset of esophageal duplication cyst in adult. Case report G Chir 30:17–20
Sarkar M, Wood R, Oh Y et al (2008) Presentation and management of acute fistulization of a foregut duplication cyst. Gastrointest Endosc 68(4):52–54
Lee H-S, Jeon H-J, Song C-W et al (1994) Esophageal duplication cyst complicated with intramural hematoma. J Korean Med Sci 9(2):188–196
Gatzinsky P, Fasth S (1978) Intramural oesophageal cyst with massive mediastinal bleeding. Scan J Thor Cardiovasc Surg 12:143–145
Kochhar R, Saluja H, Singh RS et al (2006) Endoscopic clip application for postoperative residual esophageal duplication cyst. Endoscopy 38(4):424–425
Mcmaster WG, Mukherjee K (2014) Surgical management of a symptomatic foregut duplication cyst. Am Surg 6:306–307
Zdenek K, Vladimı P, Marke H (2007) Partial laparoscopic resection of inflamed mediastinal esophageal duplication cyst. Surg Laparosc Endosc Percutan Tech 17(4):311–312
Gopp AR (2005) Anesthetic management of a patient with a mediastinal foregut duplication cyst: a case report. AANA J 73(1):55–61
Agarwal A, Singla S, Bansal M et al (2012) Infected esophageal duplication cyst masquerading as pericarditis. Intern Med 51:689–690
Tomar AL, Mannar V, Pruthi S, Aggarwal A (2015) Asymptomatic thoracic esophageal duplication cyst in a young adult with bronchiectasis. Lung Ind: Off Organ Ind Chest Soc 32(4):404
Jacob R, Hawkes ND, Bch MB et al (2003) Case report squamous carcinoma in an oesophageal foregut cyst. Br J Radiol 76:343–346
Ramírez AMR, Bohórquez ÉJF, Molano LAA et al (2018) Manejo endoscópico de quiste de duplicación esofágico: descripción de un caso. Rev Colomb Gastroenterol 33(2):180–184
James TW, Grimm IS, Baron TH (2017) Endoscopic fenestration of a symptomatic esophageal duplication cyst. VideoGIE 2(8):191–2. https://doi.org/10.1016/j.vgie.2017.04.002
Mou Y, Wen D, Liu Q et al (2015) Endoscopic resection of an esophageal duplication cyst with spraying of anhydrous alcohol. Endoscopy 47:1–2
Ivekovic H, Jouret-Mourin A, Deprez P (2012) Endoscopic fenestration of esophageal duplication cysts. Endoscopy 44:404–405
Han IS, Kim GH, Lee SJ et al (2017) A case of hemorrhage of an esophageal duplication cyst improved by endoscopic drainage. Korean J Gastroenterol 69(6):363–367
Karahasanoglu T, Ozbal A, Alcicek S (1984) Giant intra abdominal esophageal duplication cyst. Unusual Cases Tech Notes 2:1–2
Vijayaraghavan R, Charalingappa S, Belagivi S (2002) True giant intra-abdominal esophageal cyst. Ind J Gastroenterol 21:198–199
Huang L, Gao S, Dai R et al (2015) Case report laparoscopic resection of intra-abdominal esophageal duplication cyst near spleen: a case report. Int J Clin Exp Pathol 8(2):2186–2190
Loo JLLM, So JB, Shabbir A (2012) Laparoscopic excision of intrathoracic oesophageal duplication cyst in a singaporean adult male. Ann Acad Med 41(3):129–131
Noguchi T, Hashimoto T, Takeno S et al (2003) Case report Laparoscopic resection of esophageal duplication cyst in an adult. Dis Esophagus 16:148–150
Ringley C, Bochkarev V, Oleynikov D et al (2006) Esophageal duplication cyst – a guest case in robotic and computer-assisted surgery from the university of nebraska medical center. MedGenMed 8(4):25–29
Kolomainen D, Hurley PR, Ebbs SR (1998) Esophageal duplication cyst : case report and review of the literature. Dis Esophagus 11:62–65
Borcar J, Hughes C (1988) Duplication of the cervical oesophagus in adults. Aust N Z J Surg 58:746–748
Weiss LM, Fagelman D, Warhit JM (1983) CT demostration of an esophageal duplication cyst. J Comput Assist Tomogr 7(4):716–718
Bhutani M, Hoffman B, Reed C (1996) Endosonographic diagnosis of an esophageal duplicacion cyst. Endoscopy 28:396–397
Fallazadeh H, Haiderer O (1973) Esophageal duplication cyst with unusual manifestations. Chest 63(5):827–8. https://doi.org/10.1378/chest.63.5.827
Kapoor AK, Arora A, Haq S (2014) Esophageal duplication cyst. Indian J Gastroenterol 33(2):198
Huang J, Yan Z (2017) Dysphagia caused by esophageal duplication cyst. Clin Gastroenterol Hepatol 15(2):51–2. https://doi.org/10.1016/j.cgh.2016.08.027
Gordobil IM, Elorza JL, Larburu S et al (2011) Thorascopic excision of an oesophageal duplication cyst. Cir Esp 89(6):408–410
Avaro JP, Gabaudan C, Lafolie T et al (2007) Résection par vidéo thoracoscopie chirurgicale d ’ une duplication de l ’ œsophage. J Chir 144(3):264–266
Gilg MM, Swatek P, Lutfi A et al (2013) Kongenitale zystische duplikatur des ösophagus. Pathologe 6:155–158
Kuhlman E, Fishman K, Wang K-P et al (1985) Esophageal duplication cyst : ct and transesophageal. Am J Roentgenol 145:531–532
Trojan J, Mousset S, Caspary WF et al (2005) Case report An infected esophageal duplication cyst in a patient with non-Hodgkin ’ s. Dis Esophagus 18:287–289
Somani P, Sharma M (2016) Endoscopic ultrasound of esophageal duplication cyst. Ind J Gastroenterol 35:497–8. https://doi.org/10.1007/s12664-016-0701-9
Khalid S, Gremida A, Rustagi T et al (2019) Seeing double : an unusual case of chronic recurrent nausea, vomiting and epigastric pain. Dig Dis Sci 9:1–4. https://doi.org/10.1007/s10620-018-5445-1
Prasai VTA, Durham FLL (2014) Oesophageal duplication cysts, a rare cause of neck lump treated by ultrasound guided drainage : case report and review of the literature. Eur Arch Otorhinolaryngol. 276(2):1543–1546
Ramamoorthy M, Fredrick T, Jayaraman Y (2016) Oesophageal duplication cysts a case report on diagnostic and therapeutic challenge. Stanley Med J 3(3):7–10
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
MGU and DEHG performed research database and wrote the first draft. DPPA collected and analyzed the data on the methods and result section. ALA wrote discussion section and edited the final version of the manuscript. MRS designed the manuscript and performed research database. JRM helped with the design of the figures and tables, as well as edited the final version of the manuscript. All authors contributed to the design and interpretation of the study and to further drafts. MGU is the guarantor.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare(s) that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gonzalez-Urquijo, M., Hinojosa-Gonzalez, D.E., Padilla-Armendariz, D.P. et al. Esophageal Duplication Cysts in 97 Adult Patients: A Systematic Review. World J Surg 46, 154–162 (2022). https://doi.org/10.1007/s00268-021-06325-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06325-8