Abstract
Purpose
Long-term extension of a previous randomized controlled clinical trial comparing open (OVHR) vs. laparoscopic (LVHR) ventral hernia repair, assessing recurrence, reoperation, mesh-related complications and self-reported quality of life with 10 years of follow-up.
Methods
Eighty-five patients were followed up to assess recurrence (main endpoint), reoperation, mesh complications and death, from the date of index until recurrence, death or study completion, whichever was first. Recurrence, reoperation rates and death were estimated by intention to treat. Mesh-related complications were only assessed in the LVHR group, excluding conversions (intraperitoneal onlay; n = 40). Quality of life, using the European Hernia Society Quality of Life score, was assessed in surviving non-reoperated patients (n = 47).
Results
The incidence rates with 10 person-years of follow-up were 21.01% (CI 13.24–33.36) for recurrence, 11.92% (CI: 6.60–21.53) for reoperation and 24.88% (CI 16.81–36.82) for death. Sixty-two percent of recurrences occurred within the first 2 years of follow-up. No significant differences between arms were found in any of the outcomes analyzed. Incidence rate of intraperitoneal mesh complications with 10 person-years of follow-up was 6.15% (CI 1.99–19.09). The mean EuraHS-QoL score with 13.8 years of mean follow-up for living non-reoperated patients was 6.63 (CI 4.50–8.78) over 90 possible points with no significant differences between arms.
Conclusion
In incisional ventral hernias with wall defects up to 15 cm wide, laparoscopic repair seems to be as safe and effective as open techniques, with no long-term differences in recurrence and reoperation rates or global quality of life, although lack of statistical power does not allow definitive conclusions on equivalence between alternatives.
Trial registration number
ClinicalTrial.gov (NCT04192838).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to a recent meta-analysis [1], the incidence of incisional hernias (IHs) following midline abdominal incisions is estimated to be 13% at 2 years after index surgery and almost 80% will eventually need a further operation [2]. Since its first description in 1993 [3], laparoscopic incisional ventral hernia repair (LVHR) has been shown to be safe and effective and many surgical teams have begun to place an intraperitoneal mesh utilizing trocar ports to correct wall defects [4].
Recent systematic reviews [5, 6] confirm the efficacy and safety of the LVRH approach but also the scarcity of long-term outcomes or studies reporting on quality of life. The recurrence rate of IH repair increases when follow-up is lengthened and is usually underestimated. Recurrence rates have been reported from 13 on short-term follow-up to 32% on those with long-term follow-up [7, 8]. Thus, long-term follow-up (from 5 to 10 years) should be considered after IH surgery to obtain consistent evidence in terms of recurrence. Additionally, the use of meshes in an intraperitoneal position may cause host complications and foreign body reactions. The long-term risks of intraperitoneal mesh-related complications are not well known.
While recurrence rates continue to be the core endpoint in the assessment of IH repair, many authors now consider health-related quality of life (HRQoL), to be of at least of equal importance in evaluating IH repair, but long-term HRQoL reports after IH repair are extremely rare. Several hernia-specific HRQoL questionnaires have been developed over the last decade, such as the Carolina Comfort Scale [9], the Ventral Hernia Pain Questionnaire [10] or the European Hernia Society Quality of Life (EuraHS-Qol) [11, 12].
We conducted a multicenter RCT during 2003–2006 comparing laparoscopic vs. open incisional hernia repair (OVHR) focused on postoperative results, HRQoL and recurrence with one year of follow-up [13]. The current study is a long-term extension of that trial, extending our previously reported data on recurrence, reoperation and self-reported HRQoL after 10–15 years of follow-up. This study also aims to explore the long-term risk of intraperitoneal mesh-related complications.
Patients and methods
Design
Long-term follow-up extension of a randomized, parallel controlled, multicenter, open clinical trial, comparing laparoscopic versus open incisional hernia repair. For the main analysis, patients were followed up to assess recurrence from the date of index surgery (between 2003 and 2006) until recurrence, death or study completion with a clinical revision (between 2017 and 2019), whichever was first.
Setting
The study was carried out in the surgical departments of three general hospitals belonging to the Valencia Health System (VHS) [14, 15].
Patients and background
Between February 2003 and February 2006, a total of 86 patients scheduled for elective IH repair were recruited into the original RCT with a pre-planned follow-up of 1 year [13]. Current data involve 2 patients not included in our earlier paper because the participating hospital sent their data after completion of the original study (one in each arm). Patient demographics at index surgery, inclusion and exclusion criteria and short-term outcomes were reported elsewhere [13]. Briefly, patients 18 years of age or older with IH between 5 and 15 cm in their largest diameter without any contraindication for laparoscopic surgery were randomly assigned to OVHR or LVHR mesh repair (see Electronic Supplementary Material for details) and prospectively followed up over one year to asses quality of life and recurrence. The current study extends the follow-up for 10–15 years.
Surgical technique in the original trial
For the laparoscopic technique (LG), a double-layer polypropylene-ePTFE mesh was chosen (Composix, Bard), allowing at least 3 cm overlap on all sides. After reducing abdominal pressure to 8 mm Hg, the mesh was placed into the peritoneal cavity with the ePTFE side against the viscera. The edge of the mesh was secured with titanium spiral tacks (ProTack, Covidien) in a double-ring shape at 1–2 cm intervals. A minimum of four transabdominal absorbable sutures were inserted to help prevent mesh migration and tied in the subcutaneous tissue. The hernia defect was not closed. No drains were used. For the anterior open technique (OG), a standard polypropylene mesh was positioned as an inlay, (i.e., under the rectal muscles, preperitoneally), as described by Rives/Stoppa [16] or as an onlay over the external oblique fascia (i.e., subcutaneously). The technique was chosen based on the surgeon's best experience. Drains were usually placed.
Main and secondary outcomes
The main outcome of this study was the presence of hernia recurrence assessed by: (1) clinical evaluation during the first year of follow-up, taking advantage of the original RCT data, available for all patients in the study; (2) clinical evaluation, accompanied when necessary by an abdominal CT scan, carried out between 2017 and 2019 for patients who accepted participation; (3) clinical record review, including available abdominal CT scans close to patients’ death, for patients deceased prior to the clinical evaluation of the extension study.
Secondary outcomes include: (1) surgical repair of the recurrent IH; (2) mesh-related complications including reoperation for intestinal obstruction or mesh extrusion, intestinal fistulas or adhesion syndrome treated conservatively; (3) death by any cause; (4) HRQoL assessed by the EuraHS-QoL in non-reoperated patients who accepted participation in the extension study.
Sample size and power
The sample size was determined for the original study. This was not sufficient to determine equivalence in the current extension study. (See Electronic Supplementary Material for details).
Instruments
We used a Spanish translation of the EuraHS-QoL scale [11, 12]. The EuraHS-QoL questions are divided into 3 domains: pain (3 questions, range 0–30), restriction of activities (4 questions, range 0–40) and cosmetic discomfort (2 questions, range 0–20). The total score ranges from 0–90, with the lower scores being the most favorable outcome. The missing values were treated according to the instructions of the validation study [11].
Operational process
During 2017–2019, living patients from the original RCT were contacted and after being informed of the study were invited to a new clinical examination. Patients that did not respond after two attempts were considered lost to follow-up, although data on recurrence from the first year of follow-up were incorporated into the study. If a recurrent hernia was detected at clinical examination, recurrence was registered and dated on the date of the review in the absence of previous evidence of recurrence. In suspected or doubtful recurrences, an abdominal CT scan was always performed. Mesh-related complications were assessed by a clinical examination, CT scan and review of clinical files. Medical records of all deceased patients were searched for recurrent hernia, reoperations and year of death. All abdominal CT scans performed for any cause close to the patient’s death were re-examined for recurrence.
Ethics
The original RCT protocol was approved by the Institutional Review Board (IRB) of the three participating hospitals. The extension study was approved by the IRB of the Arnau de Vilanova University Hospital (reference number: 16/2017). Informed written consent was obtained from all the patients before their inclusion in the trial. The extension trial protocol was registered in ClinicalTrial.gov (NCT04192838).
Analysis
The analysis was carried out by intention to treat, evaluating patients in the group they were randomized into, regardless of whether some of the patients in the LVHR group underwent a conversion and were finally operated on by open surgery. The only exception to this criterion was the analysis of mesh complications, in which only patients who received an intraperitoneal mesh were included (therefore excluding converted patients). Differences between groups at baseline were analyzed using the t test and the proportion differences test. Recurrence and reoperation rates, and death by 1000 person-year of follow-up were estimated with their respective 95% confidence intervals (CI), and survival to recurrence and reoperation were estimated using the Kaplan–Meier method. Differences between groups were evaluated using the log-rank test. Additionally, rates of mesh complications by 1000 person-year were estimated for the LVHR group, excluding conversions. Finally, between-group differences in EuraHS-QoL dimensions and total scores were analyzed using the t test. All analyses were performed using STATA 13.1 (Stata Corp, College Station, TX) statistical software.
Results
From the 86 patients participating in the original trial (OVHR: 40; LVHR: 46) (see the flow study diagram in Fig. 1), one patient (open group) withdrew from the study. Of the 85 remaining patients, 25 (29%) had died at the initiation of the extension study and were evaluated by review of the EMR and available abdominal CT scans; they contribute to the follow-up until the date of death. From the remaining 60, two did not respond after the second contact attempt (1 in each arm) and they only contribute to the study with the first year of follow-up of the original RCT. The remaining 58 patients (96.7% of all living patients) were clinically evaluated between 2017 and 2019 and, when appropriate, received an abdominal CT scan. From these 58 patients, 11 (19.0%) were excluded for HRQoL assessment due to a further abdominal operation during follow-up.
Table 1 shows the baseline characteristics of the included patients. There were no significant differences between the OVHR and the LVHR arms in all the variables analyzed. Conversion to open repair was required in 6 (13.0%) of the LVHR patients.
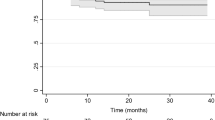
The 85 patients provided a total of 856.47 person-years of follow-up for the evaluation of recurrence, with an average of 10.08 years per patient (median: 12.88; interquartile range: 5.98–13.80). A total of 18 patients (9 in each group) presented recurrence during follow-up, with an incidence rate of 21.01% (95% CI 13.24–33.36) with 10 person-years of follow-up and no significant differences between arms (Table 2). Figure 2 shows the distribution of recurrences throughout the follow-up. Sixty-two percent of the recurrences (OVHR: 6 [66.7%] vs. LVHR: 5 [55.6%]) occurred within the first 2 years of follow-up. In 11 of the 18 patients with recurrence (61.1%; OVHR: 4 [44.4%] vs. LVHR: 7 [77.8%]), the recurrent IH was reoperated on during follow-up (incidence rate: 11.92% with 10 person-years of follow-up) with no significant differences between the OVHR and LVHR arms.
Of the 40 LVHR patients with an intraperitoneal mesh followed up with a median of 13.4 years, 3 complications were possibly related to the mesh (Table 2). One patient presented a chronic sinus due to partial mesh extrusion 12 years after the index surgery and 2 were reoperated for intestinal obstruction (7 and 9 years after the index surgery). No intestinal fistulas were recorded. All patients with an intraperitoneal mesh complication had intense adhesions registered during the index surgery. These figures represent an incidence rate of 6.15% mesh complications by 10 person-year of follow-up. The OVHR group did not present any mesh-related complications, but 2 patients, both with converted laparoscopies, presented an adhesion syndrome treated conservatively. Finally, 25 patients (OVHR: 13 [33.3%]; LVHR: 12 [26.1%]) died during follow-up, with a mean rate of 24.9% deaths by 10 person-year of follow-up and no significant differences between groups.
The results of the EuraHS-QoL questionnaire for the 47 patients without reoperations, with 13.8 years of mean follow-up (range: 12.0–15.6 years), are reported in Table 3. Global patients’ scores show a mean of 6.63 (95% CI 4.50–8.78) over 90 possible points and no statistically significant differences between arms. Nevertheless, LVHR shows a better global score close to statistical significance. Noticeably, the cosmetic discomfort dimension was the one that most affected the EuraHS-QoL scoring. In EuraHS-QoL dimensions, LHVR scored better in all dimensions but differences were only significant regarding ADL restriction (OVHR: 1.09; LVHR: 0.16) and their clinical relevance over 40 possible scoring points in this dimension is uncertain.
Discussion
The most remarkable result of the study is a recurrence rate of 21.0% with 10 person-years of follow-up and no differences between open and laparoscopic approaches. However, this last result must be taken cautiously due to a lack of statistical power, reflected in the wide confidence intervals of the estimated event rates.
The 21% recurrence rate is compatible with previous series with long follow-up [7, 8, 17]. In this regard, short-term studies (one-third of our recurrences were diagnosed 2 years after index surgery) or studies that do not include a clinical examination using only reoperation as a proxy for recurrence [18], fail to identify an accurate long-term recurrence rate. In the same way, studies that attribute the same follow-up time to all patients, without censoring cases that die or suffer a recurrence, tend to underestimate the incidence rates.
Our initial study is one of the first designed according to an accurate formal randomization, regarding the laparoscopic approach to ventral hernias using highly standardized procedures. Consequently, follow-up in this study, focusing on recurrence, HRQoL and intraperitoneal mesh behavior, is one of the longest reported in the literature. A recent meta-analysis of comparative trials and a Cochrane review have found significant advantages of the laparoscopic technique over conventional surgery [4, 19], especially when considering the decreases in wound infections and length of hospital stay. In contrast, others [20, 21] have reported a lack of relevant advantages for the laparoscopic approach. The similarity in estimated rates of recurrence, reoperation, complications and death between groups in our study would strengthen this last opinion, but due to small sample size and lack of power these results should be taken as simply exploratory.
The placement of an intraperitoneal mesh and its behavior is a matter of concern. Mesh-related complications have been reported previously [8, 22, 23] with complication rates between 6 and 20%, including bowel obstruction, enterocutaneous fistulas and the development of chronic sinus tracts. Only one of these studies [22], with 29 cases, evaluated long-term complications following laparoscopic mesh repair. Our study includes 40 cases of intraperitoneal mesh placement for long-term evaluation recording only 3 complications broadly attributable to mesh. We believe that using a double-layer mesh, with polypropylene on its parietal face and PTFE on its visceral face, has minimized complications due to its intraperitoneal situation, given the proven low adhesiveness of PTFE [24,25,26].
Outcomes after IH repair are most often measured by recurrence rate, but this may be insufficient to allow for an accurate description of what patients perceive as successful treatment. In recent years, patient HRQoL has become a new dimension for measuring operative success. Although pain is an important parameter determining success, restriction of activities and cosmetic outcomes are also of importance. It has even been postulated that patient-reported HRQoL outcomes are superior to clinical ratings by avoiding observer bias [27,28,29]. Interestingly, in our study, global HRQoL scores with more than 13 years of mean follow-up showed no significant differences between laparoscopic and open groups, but restriction of activities and cosmetic discomfort seem to be less after laparoscopic repair. Comorbidities other than recurrent or repaired incisional hernia can affect HRQoL, especially in patients with a mean age of around 70 at the end of follow-up. We were unable to rule out this factor since these comorbidities were not registered in our data. Mortality, with 13 years of median follow-up, was, as expected, high, but our design was not oriented toward the identification of the causes of death.
Loss to follow-up is common in clinical studies which seriously limits conclusions. A degree of follow-up over 80% is considered optimal, a percentage rarely achieved in published studies [30, 31]. Because of our design, 96.7% of the living patients could be clinically examined, thus reinforcing the soundness of our results.
As for the limitations, the reduced sample size (with the subsequent lack of statistical power to ensure equivalence or differences between groups in the relevant endpoints) and the retrospective evaluation of deceased patients are probably the most important. The direct translation of the EuraHS-QoL (a cross-cultural adaptation to Spanish was not available) and the lack of information on other variables, such as comorbidity, that could influence quality of life, are also relevant when considering the HRQoL results.
The comparison against two different open techniques is another possible weakness. However, due to the participation of multiple centers and surgeons, we decided to compare laparoscopic repair against the technique with which the team had maximal experience.
Conclusions
With the above limitations, in wall defects up to 15 cm wide laparoscopic IH repair seems to be as safe and effective as open techniques in terms of recurrence, reoperation rates or global HRQoL. Restriction of activities and cosmetic results seem to be better in laparoscopic approaches, but the clinical relevance of these differences is uncertain. The complication rate after intraperitoneal placement of PTFE-coated meshes was low, late in time and could be related to previous abdominal surgeries rather than to the direct contact of the mesh with abdominal contents.
References
Bosanquet DC, Ansell J, Abdelrahman T, Cornish J, Harries R, Stimpson A et al (2015) Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14,618 patients. PLoS One 10(9):e0138745
Nieuwenhuizen J, Kleinrensink GJ, Hop WC, Jeekel J, Lange JF (2008) Indications for incisional hernia repair: an international questionnaire among hernia surgeons. Hernia 12(3):223–225
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc 3(1):39–41
Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD007781.pub2
Zhang Y, Zhou H, Chai Y, Cao C, Jin K, Hu Z (2014) Laparoscopic versus open incisional and ventral hernia repair: a systematic review and meta-analysis. World J Surg 38(9):2233–2240. https://doi.org/10.1007/s00268-014-2578-z
Kössler-Ebs JB, Grummich K, Jensen K, Hüttner FJ, Müller-Stich B, Seiler CM et al (2016) Incisional hernia rates after laparoscopic or open abdominal surgery-a systematic review and meta-analysis. World J Surg 40(10):2319–2330. https://doi.org/10.1007/s00268-016-3520-3
Andersen LP, Klein M, Gögenur I, Rosenberg J (2009) Long-term recurrence and complication rates after incisional hernia repair with the open onlay technique. BMC Surg 9:6
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240(4):578–583
Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW (2008) Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg 206(4):638–644
Clay L, Fränneby U, Sandblom G, Gunnarsson U, Strigård K (2012) Validation of a questionnaire for the assessment of pain following ventral hernia repair—the VHPQ. Langenbecks Arch Surg 397(8):1219–1224
Muysoms FE, Vanlander A, Ceulemans R, Kyle-Leinhase I, Michiels M, Jacobs I et al (2016) A prospective, multicenter, observational study on quality of life after laparoscopic inguinal hernia repair with ProGrip laparoscopic, self-fixating mesh according to the European registry for abdominal wall hernias quality of life instrument. Surgery 160(5):1344–1357
Muysoms F, Campanelli G, Champault GG, DeBeaux AC, Dietz UA, Jeekel J et al (2012) EuraHS: the development of an international online platform for registration and outcome measurement of ventral abdominal wall hernia repair. Hernia 16(3):239–250
Asencio F, Aguiló J, Peiró S, Carbó J, Ferri R, Caro F, Ahmad M (2009) Open randomized clinical trial of laparoscopic versus open incisional hernia repair. Surg Endosc 23(7):1441–1448
Martin-Moreno JM, Alonso P, Clavería A, Gorgojo L, Peiró S (2009) Spain: a decentralised health system in constant flux. BMJ 338:b1170
García-Sempere A, Orrico-Sánchez A, Muñoz-Quiles C, Hurtado I, Peiró S, Sanfélix-Gimeno G et al (2020) Data resource profile: the valencia health system integrated database (VID). Int J Epidemiol 49(3):740–741e
Chevrel JP, Flament JB (1995) Traitement des eventrations de la paroi abdominale. Encycl med chir (Paris France). Tech Chir Appar Dig 6:40–165
Juvany M, Hoyuela C, Carvajal F, Trias M, Martrat A, Ardid J (2018) Long-term follow-up (at 5 years) of midline incisional hernia repairs using a primary closure and prosthetic onlay technique: recurrence and quality of life. Hernia 22(2):319–324
Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T (2012) Reoperation versus clinical recurrence rate after ventral hernia repair. Ann Surg 256(6):955–958
Arita NA, Nguyen MT, Nguyen DH, Berger RL, Lew DF, Suliburk JT et al (2015) Laparoscopic repair reduces incidence of surgical site infections for all ventral hernias. Surg Endosc 29(7):1769–1780
Al Chalabi H, Larkin J, Mehigan B, McCormick P (2015) A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg 20:65–74
Awaiz A, Rahman F, Hossain MB, Yunus RM, Khan S, Memon B, Memon MA (2015) Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Hernia 19(3):449–463
Fortelny RH, Petter-Puchner AH, Glaser KS, Offner F, Benesch T, Rohr M (2010) Adverse effects of polyvinylidene fluoride-coated polypropylene mesh used for laparoscopic intraperitoneal onlay repair of incisional hernia. Br J Surg 97(7):1140–1145
Leber GE, Garb JL, Alexander AI, Reed WP (1998) Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 133(4):378–382
Bellón J, García-Carranza A, Jurado F, García-Honduvilla N, Carrera A, Buján J (2001) Peritoneal regeneration after implant of a composite prosthesis in the abdominal wall. World J Surg 25:147–152
Bachman S, Ramshaw B (2008) Prosthetic material in ventral hernia repair: how do I choose? Surg Clin N Am 88:101–112
Novitsky Y, Harrell A, Cristiano J et al (2007) Comparative evaluation of adhesion formation, strength of ingrowth and textile properties of prosthetic meshes after long-term intra-abdominal implantation in a rabit. J Surg Res 140:6–11
Itani KM, Neumayer L, Reda D, Kim L, Anthony T (2004) Repair of ventral incisional hernia: the design of a randomized trial to compare open and laparoscopic surgical techniques. Am J Surg 188(6A Suppl):22S-29S
Pell JP (1995) Impact of intermittent claudication on quality of life. Eur J Vasc Endovasc Surg 9(4):469–72
Colavita PD, Tsirline VB, Belyansky I, Walters AL, Lincourt AE, Sing RF et al (2012) Prospective, long-term comparison of quality of life in laparoscopic versus open ventral hernia repair. Ann Surg 256(5):714–722
Fewtrell MS, Kennedy K, Singhal A, Martin RM, Ness A, Hadders-Algra M et al (2008) How much loss to follow-up is acceptable in long-term randomised trials and prospective studies? Arch Dis Child 93(6):458–461
Kristman V, Manno M, Côté P (2004) Loss to follow-up in cohort studies: how much is too much? Eur J Epidemiol 19(8):751–760
Author information
Authors and Affiliations
Contributions
All authors have participated in the conception and design, or analysis and interpretation of the data, drafting the article or revising it critically for important intellectual content; and approval of the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts or interests or disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Asencio, F., Carbó, J., Ferri, R. et al. Laparoscopic Versus Open Incisional Hernia Repair: Long-Term Follow-up Results of a Randomized Clinical Trial. World J Surg 45, 2734–2741 (2021). https://doi.org/10.1007/s00268-021-06164-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06164-7