Abstract
Background
Lymph node metastasis (LNM) has been regarded as one of the prognostic factors in patients with ampulla of Vater carcinoma (AC). However, the consensus about an optimal cutoff value of the number of LNMs and the definition of the regional lymph nodes (RLNs) has not been achieved.
Methods
This study included 114 consecutive patients who underwent pancreatoduodenectomy for AC between January 2002 and March 2019.
Results
The minimum p value approach for the greatest difference in the overall survival classified the number of LNM into none (N0, n = 66), from 1 to 2 (N1, n = 32), and ≥3 LNM (N2, n = 11) (p = 0.004). Distant LNM was defined as M1 (n = 5). Significant differences in relapse-free survival (RFS) were found between N0 and N1 (p < 0.001), N1 and N2 (p = 0.047), and N1 and M1 (p = 0.044) but not between N2 and M1 (p = 0.683). Moreover, the patients with regional LNM were classified into two groups: Np group (n = 35, LNM only in pancreatic head region) and Nd group (n = 8, LNM in other regional location). Significant differences in the RFS were found between N0 and Np (p < 0.001), Np and Nd (p = 0.004), and Np and M1 (p = 0.033) but not between Nd and M1 (p = 0.883). A Cox proportional hazards analysis for RFS revealed that ≥ 3 LNMs (hazards ratio [HR], 3.22) and LNM except for pancreatic head region (HR, 4.27) were individually independent worse prognostic factors.
Conclusions
≥3 LNMs and regional LNM except for pancreatic head region were associated with poor prognosis comparable to that of the patients with M1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ampulla of Vater carcinoma (AC) is rare, accounting for only 0.2% of gastrointestinal cancers and approximately 7% of all periampullary cancers [1]. AC presents with symptoms in the early phase of the disease course due to biliary obstruction; therefore, it has been known to have a comparatively favorable prognosis among periampullary malignancies, with reported 5-year OS rates of 30–70% after resection [2, 3]. However, the low incidence of AC makes it difficult to establish evidence on clinical practice and outcomes.
Lymph node metastasis (LNM) has been recognized as one of the pivotal prognostic factors [4]. LNMs are observed in 20–50% of resected AC, and survival rates of patients with LNM decrease by more than half compared to that of the patients without LNM [5,6,7]. Moreover, previous studies reported that the number of LNM is associated with survival; however, the cutoff values varied among these studies [8,9,10]. The current 8th edition of the Union for International Cancer Control (UICC) and American Joint Committee on Cancer (AJCC) classification classified N-status into N0 (node negative), N1 (1 to 3 LNMs), and N2 (4 or more LNMs). However, Kang et al. reported that stratifying positive LNM as N1 (1 to 2 LNMs) versus N2 (3 or more LNMs) had significant prognostic value [11].
Other than the number of LNM, there are some reports to show the prognostic significance of the location of LNM in AC [12,13,14]. However, the classification of LNM according to its location has not been widely applied in clinical settings and the significance remains unclear. The reason for this is that the definitions of regional lymph node (RLN) varied among the staging systems, such as the UICC/AJCC classification and the staging systems of the Japanese Society of Hepato-Biliary-Pancreatic Surgery [15]. There is no evidence supporting the definition of RLN for AC in each classification. Furthermore, AC is not mentioned in the National Comprehensive Cancer Network guidelines [16]. Therefore, there is an urgent need to define RLN internationally and make the guideline regarding AC.
The aim of this study was to investigate the clinical relevance of the number of LNM and identified optimal cutoff value for further classification of N-status. Furthermore, to achieve consensus about RLN for AC, the prognostic impact of LNM according to its location was investigated.
Methods
Patient population
The study was approved by the institutional review board (J2019-130-2019-1), and each study subject provided their written informed consent. A retrospective review was performed of a prospectively maintained AC database. A total of 114 patients were diagnosed with AC between January 2002 and March 2019 and underwent pancreatoduodenectomy (PD). The patients diagnosed with neuroendocrine neoplasms, mucinous cystic neoplasms and unclassified tumors were excluded from the present study. The patients who underwent local resection, such as ampullectomy or pancreas-sparing duodenectomy, were also excluded.
Surgical strategy and procedures
PD with lymph nodes dissection was performed as the standard treatment for AC, as previously described [17]. Routine dissection of lymph nodes was performed in the following areas: lymph nodes along the common bile duct, common hepatic artery, portal vein, pyloric, infrapyloric, subpyloric, proximal mesenteric, posterior and anterior pancreaticoduodenal vessels, and the superior mesenteric vein and artery. In our institution, for all patients undergoing PD, para-aortic lymph node sampling procedures were routinely performed. When the frozen sections of sampled para-aortic lymph nodes were positive for cancer, we basically abandoned resection. However, PDs with para-aortic lymphadenectomies were performed in 5 patients with good performance status, and other tumor factors were relatively preferable for prognosis including negative lavage cytology.
Postoperative follow-up
All resected specimens were examined by a pathologist (K.S.) and evaluated based on the 8th UICC/AJCC staging system. In this study, RLNs were defined by UICC/AJCC staging system. The final surgical margins were considered positive if tumor cells were microscopically detectable at any of the resected margins. Para-aortic LNM was defined as M1. Adjuvant therapy after surgery was not performed as a standard treatment during the study periods, except for clinical trials. All patients were followed using computed tomographic scanning or abdominal ultrasound scans every 3–6 months after surgery.
Statistical analyses
Categorical variables were compared using Fisher’s exact test. Survival curves were estimated using the Kaplan–Meier method, and statistical differences were examined using the log-rank test. The Cox proportional-hazards model was used for further evaluations of a multivariate analysis. The cutoff value for the number of LNM was evaluated based on a minimum p value approach [18]. Statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan)—a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). p < 0.050 was considered statistically significant.
Results
Clinicopathologic and treatment factors
Clinicopathologic and treatment factors in the patients are described in Table 1. All the five patients with M1 disease had para-aortic LNM. No patient received neoadjuvant therapy, and nine patients (7.9%) received adjuvant chemotherapy with S-1 according to the protocol of the clinical trials for the evaluation of the efficacy of adjuvant therapy for cholangiocarcinoma. Of these patients, 36 of them (31.6%) experienced disease recurrence during the study period. For recurrent disease, gemcitabine-based chemotherapy was generally performed. The median follow-up time was 33.2 months (range 1.1–170.2). The 5-year RFS and OS rate was 62.4% and 67.4%, respectively.
Lymph node analysis
A total of 48 cases (42.1%) had LNM. The locations of LNMs are shown in Table 2. All of the patients with LNM had LNM along the posterior and anterior pancreaticoduodenal vessels (PHLN, peripancreatic head lymph node). PHLN are defined as lymph node groups 13 and 17 in the staging systems of the Japanese Society of Hepato-Biliary-Pancreatic Surgery [15]. PHLN are located on the anterior and posterior surface of the head of the pancreas. The upper borderline was the upper border of the pancreas (Fig. 1a). Patients with only PHLN metastasis are classified into the proximal node group (Np group: n = 35) in this study. In contrast, there were 8 cases with regional LNM that were not PHLNs. They are classified into distal node group (Nd group) in this study (Fig. 1b).
Np and Nd classification a Np group. Peripancreatic head lymph nodes (PHLNs) are located on the anterior and posterior surface of the head of the pancreas. Moreover, the upper borderline is the upper border of the pancreas. Patients with only PHLN metastasis are classified into Np group. b Nd group. The patients with regional LNM that are not PHLN but are lymph nodes along the common bile duct, common hepatic artery, portal vein, pyloric, infrapyloric, subpyloric, proximal mesenteric, and the superior mesenteric vein and artery are classified into the Nd group. The lymph nodes along the pyloric, infrapyloric, and subpyloric regions are omitted in this figure. Abbreviations: AIPDA, anterior inferior pancreaticoduodenal artery; Ao, Aorta; ASPDA, anterior superior pancreaticoduodenal artery; CHA, common hepatic artery; GDA, gastroduodenal artery; PIPDA, posterior inferior pancreaticoduodenal artery; PSPDA, posterior superior pancreaticoduodenal artery; PV, portal vein; SMA, superior mesenteric artery; SMV, superior mesenteric vein; SpA, splenic artery; 1stJA, first jejunal artery
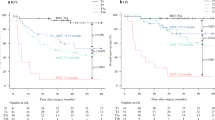
A comparison of the prognosis according to the number of lymph node metastasis
The optimal number of LNM cutoff value for nodal classification was determined using the prognostic differences of 48 patients with LNM. The optimal number of LNM for dividing patients into two groups using the greatest difference in OS was 3 or more (p = 0.004) when using the minimum p value approach (Fig. 2). Based on this result, we proposed a new nodal classification as N0 (node negative), N1 (1–2 LNMs, n = 32), and N2 (3 or more LNMs, n = 11). When this proposed classification was applied, significant differences in the RFS and OS were found between N0 and N1 (RFS, p < 0.001; OS, p = 0.003), N1 and N2 (RFS, p = 0.047; OS, p = 0.007), and N1 and M1 (RFS, p = 0.044; OS, p = 0.040) but not between N2 and M1 (RFS, p = 0.683; OS, p = 0.854) (Fig. 3). On the other hand, when the 8th UICC/AJCC staging system was applied, significant differences in the RFS and OS were found between N0 and N1 (RFS, p < 0.001; OS, p < 0.001), but not between N1 and M1 (RFS, p = 0.055; OS, p = 0.071) and N2 and M1 (RFS, p = 0.890; OS, p = 0.963) (Fig. 3). As for N1 and N2, significant differences in the OS were found (p = 0.040), but not found in the RFS (p = 0.069) (Fig. 4). A multivariate analysis for RFS using the Cox proportional hazards analysis adjusted for pancreatic invasion, duodenal invasion, lymphatic invasion, venous invasion, and 3 or more LNMs identified that the presence of 3 or more LNMs was the only independent prognostic factor associated with RFS (HR, 3.22 [1.47–7.06, p = 0.004]) (Table 3).
Prognostic stratification according to the number of the lymph node metastasis, based on our proposal classification. a The RFS curves of the no lymph node metastasis group, metastasis in 1 or 2 regional lymph nodes group, metastasis in 3 or more regional lymph nodes group, and para-aortic lymph node metastasis group. b The OS curves of the no lymph node metastasis group, metastasis in 1 or 2 regional lymph nodes group, metastasis in 3 or more regional lymph nodes group, and para-aortic lymph node metastasis group
Prognostic stratification according to the number of the lymph node metastasis, based on the 8th UICC/AJCC classification. a The RFS curves of the no lymph node metastasis group, metastasis in 1–3 regional lymph nodes group, metastasis in 4 or more regional lymph nodes group, and para-aortic lymph node metastasis group. b The OS curves of the no lymph node metastasis group, metastasis in 1–3 regional lymph nodes group, metastasis in 4 or more regional lymph nodes group, and para-aortic lymph node metastasis group
A comparison of the prognosis according to the location of lymph node metastasis
The patients were classified into four groups with respect to the location of LNM, i.e., N0 group (node negative, n = 66), Np group (n = 35), Nd group (n = 8), and M1 group (n = 5). When this proposed classification was applied, significant differences in the RFS and OS were found between N0 and Np (RFS, p < 0.001; OS, p = 0.002), and Np and Nd (RFS, p = 0.004; OS, p = 0.004), but not between Nd and M1 (RFS, p = 0.883; OS, p = 0.826). As for Np and M1, significant differences in the RFS were found (p = 0.033), but not found in the OS (p = 0.0568) (Fig. 5). A multivariate analysis for RFS using the Cox proportional hazards analysis adjusted for pancreatic invasion, duodenal invasion, lymphatic invasion, venous invasion, and LNM except for PHLN identified that LNM except for PHLN was the only independent prognostic factor associated with RFS (HR, 4.27 [1.92–9.48, p < 0.001]) (Table 4).
Prognostic stratification according to the location of the lymph node metastasis. a The RFS curves of the no lymph node metastasis group, Np group (metastasis along posterior and anterior pancreaticoduodenal vessels), Nd group (metastasis in other regional areas), and para-aortic lymph node metastasis group. b The OS curves of the no lymph node metastasis group, Np group (metastasis along the posterior and anterior pancreaticoduodenal vessels), Nd group (metastasis in other regional areas), and para-aortic lymph node metastasis group
Discussion
The purpose of this study was to propose an optimal classification of LNM according to the number of LNM and to define RLN of AC based on clinical relevance. The results of this study could propose an alternative classification of N-status into N0 (none), N1 (1–2 LNMs), and N2 (3 or more LNMs). The prognosis of patients with 3 or more LNMs was comparable with that of patients with distant metastasis. Moreover, all of the patients with LNM had PHLN metastasis, while there were only 8 cases (7.0%) in the Nd group. The prognostic outcome in patients in the Nd group was significantly worse than that of Np group and comparable to that of the patients with M1.
For AC, as well as other digestive system tumors [19,20,21,22], the number of LNM has been regarded as a prognostic factor [8,9,10, 23]. However, the cutoff value varied among studies [8,9,10]. Lee et al. [24] noted the factor of 3 or more LNMs had the independent power in predicting a poor outcome in patients with AC after resection. Meanwhile, Sierzega et al. [25] reported that 4 or more LNMs was the independent prognostic factor in patients with AC. In this study, the presence of 3 or more LNMs was identified as a best cutoff value, and the prognostic stratification of our classification was better than that of UICC/AJCC classification; however, an absolute LNM cutoff value is still contentious. Larger sample sizes are needed to prove the optimal cutoff value of LNM.
There is no consensus on the extent of lymphadenectomy for AC. Therefore, the number of nodes retrieved is different between institutions. AJCC recommends 12 or more lymph nodes evaluated for accurate nodal staging. In this study, the median number of lymph nodes examined was 23. Therefore, staging in this study might be qualifiable. The different number and different extent of examined lymph nodes potentially caused stage migration and resulted in the different cutoff value among studies. Therefore, unification of the definition of RLN for AC is a priority issue.
The prognostic significance of the location of LNM has also widely accepted in AC [12,13,14]. In this study, only 7.0% of the patients had Nd LNM and the prognosis with Nd LNM was comparable with distant metastasis. The findings might suggest that the dissection of Nd LNM may provide little clinical benefit of upfront surgery. In fact, it has been reported that the involvement of the superior mesenteric nodes indicates a poor outcome after resection [13]. Lymphatic invasion of AC is considered toward superior mesenteric artery along the posterior pancreaticoduodenal vessels because ampulla of Vater is derived embryologically from ventral pancreas [26]. Therefore, the invasion may be unlikely to be toward the gastric duodenal artery, common hepatic artery, and pyloric, infrapyloric, and subpyloric vessels [26]. In this series, five patients had para-aortic LNM at the time of PD, and three of them died of the disease within a year after resection. De Castro et al. also reported similar results [27]. These results suggest that only PHLNs were defined as RLN and the other nodes might be suitable to be excluded from RLN for AC.
There is also no consensus on the best chemotherapy for patients with advanced AC because of the rarity of this disease. In our institution, adjuvant therapy was not performed in any patients regardless of the staging of the AC, except for clinical trials, because of the lack of data from randomized trials proving a survival advantage. A meta-analysis of 14 studies found no associated survival benefit for adjuvant therapy in the treatment of periampullary cancer [28]. In the systematic review, a total of 1671 patients (904 in the control group and 767 who received adjuvant therapy) were included. The median 5-year OS rate was 37.5% in the control group, while it was 40.0% in the adjuvant group (HR, 1.08 [0.91–1.28, p = 0.067]) [28]. Based on the results from the ABC-02 trial, it is considered that the combination of gemcitabine and cisplatin is a reasonable approach [29]. Similarly, there is no consensus regarding the optimal management of patients after curative resection. However, some studies show that adjuvant chemotherapy was associated with improved survival in patients with resected AC, especially with advanced stage disease [2, 30,31,32]. The patients will likely be treated with a fluorouracil- or gemcitabine-based regimen as extrapolated using data from other cases of periampullary cancers [2, 30, 31]. Because the prognosis of the patients with 3 or more LNM and/or Nd LNM was comparable with that of the patients with distant metastasis after curative resection, systemic chemotherapy is preferable for the patients that are preoperatively suspected of having 3 or more LNM and/or Nd LNM.
This study is associated with some limitations, including its retrospective nature, short follow-up period, and the fact that it was conducted in a single center. In particular, N2, Nd, and M1 patients were only 11 (9.6%), 8 (7.0%), and 5 (4.4%), respectively. From the viewpoint of LNM, the population in each subgroup is biased and relatively small in some subgroups, potentially leading to a statistical type II error. Therefore, larger sample sizes are needed in order to prove that the stratification of the prognosis in the 8th edition is insufficient. Further prospective studies are required to precisely evaluate the clinical significance of LNM in the treatment of AC.
Reconsidering the N category based on the prognostic impact, it can be reasonable that only PHLN would be defined as RLN, and the optimum cutoff value was 3 or more. Surgical indications may be carefully determined in patients with suspected Nd LNM or 3 or more LNMs based on the preoperative images. After surgery, for the patients with Nd LNM or 3 or more LNMs confirmed by pathologic examination, addition of chemotherapy may need to be considered to improve survival.
References
Jemal A, Siegel R, Ward E et al (2008) Cancer statistics, 2008. CA Cancer J Clin 58:71–96
Kim K, Chie EK, Jang JY et al (2009) Role of adjuvant chemoradiotherapy for ampulla of Vater cancer. Int J Radiat Oncol Biol Phys 75:436–441
Narang AK, Miller RC, Hsu CC et al (2011) Evaluation of adjuvant chemoradiation therapy for ampullary adenocarcinoma: the Johns Hopkins Hospital-Mayo Clinic collaborative study. Radiat Oncol 6:126
Williams JA, Cubilla A, Maclean BJ et al (1979) Twenty-two year experience with periampullary carcinoma at Memorial Sloan-Kettering Cancer Center. Am J Surg 138:662–665
Chen SC, Shyr YM, Chou SC et al (2015) The role of lymph nodes in predicting the prognosis of ampullary carcinoma after curative resection. World J Surg Oncol 13:224
Balci S, Basturk O, Saka B et al (2015) Substaging Nodal Status in Ampullary Carcinomas has Significant Prognostic Value: proposed Revised Staging Based on an Analysis of 313 Well-Characterized Cases. Ann Surg Oncol 22:4392–4401
Roland CL, Katz MH, Gonzalez GM et al (2012) A high positive lymph node ratio is associated with distant recurrence after surgical resection of ampullary carcinoma. J Gastrointest Surg 16:2056–2063
Choi SB, Kim WB, Song TJ et al (2011) Surgical outcomes and prognostic factors for ampulla of Vater cancer. Scand J Surg 100:92–98
Sommerville CA, Limongelli P, Pai M et al (2009) Survival analysis after pancreatic resection for ampullary and pancreatic head carcinoma: an analysis of clinicopathological factors. J Surg Oncol 100:651–656
Sakata J, Shirai Y, Wakai T et al (2007) Number of positive lymph nodes independently affects long-term survival after resection in patients with ampullary carcinoma. Eur J Surg Oncol 33:346–351
Kang HJ, Eo SH, Kim SC et al (2014) Increased number of metastatic lymph nodes in adenocarcinoma of the ampulla of Vater as a prognostic factor: a proposal of new nodal classification. Surgery 155:74–84
Roder JD, Schneider PM, Stein HJ et al (1995) Number of lymph node metastases is significantly associated with survival in patients with radically resected carcinoma of the ampulla of Vater. Br J Surg 82:1693–1696
Shirai Y, Tsukada K, Ohtani T et al (1996) Carcinoma of the ampulla of Vater: is radical lymphadenectomy beneficial to patients with nodal disease? J Surg Oncol 61:190–194
Kayahara M, Nagakawa T, Ohta T et al (1997) Surgical strategy for carcinoma of the papilla of Vater on the basis of lymphatic spread and mode of recurrence. Surgery 121:611–617
Miyazaki M, Ohtsuka M, Miyakawa S, et al (2015) Classification of biliary tract cancers established by the Japanese Society of Hepato-Biliary-Pancreatic Surgery: 3(rd) English edition. J Hepatobiliary Pancreat Sci 22:181-196
Network NCC NCCN Guidelines, 2019
Kohga A, Yamamoto Y, Sano S et al (2017) Surgical Strategy for T1 Duodenal or Ampullary Carcinoma According to the Depth of Tumor Invasion. Anticancer Res 37:5277–5283
Mazumdar M, Glassman JR (2000) Categorizing a prognostic variable: review of methods, code for easy implementation and applications to decision-making about cancer treatments. Stat Med 19:113–132
Ichikura T, Tomimatsu S, Okusa Y et al (1993) Comparison of the prognostic significance between the number of metastatic lymph nodes and nodal stage based on their location in patients with gastric cancer. J Clin Oncol 11:1894–1900
Kodera Y, Yamamura Y, Shimizu Y et al (1998) The number of metastatic lymph nodes: a promising prognostic determinant for gastric carcinoma in the latest edition of the TNM classification. J Am Coll Surg 187:597–603
Cohen AM, Tremiterra S, Candela F et al (1991) Prognosis of node-positive colon cancer. Cancer 67:1859–1861
Tang R, Wang JY, Chen JS et al (1995) Survival impact of lymph node metastasis in TNM stage III carcinoma of the colon and rectum. J Am Coll Surg 180:705–712
Imamura T, Yamamoto Y, Sugiura T et al (2019) The Prognostic Relevance of the New 8th Edition of the Union for International Cancer Control Classification of TNM Staging for Ampulla of Vater Carcinoma. Ann Surg Oncol 26:1639–1648
Lee JH, Lee KG, Ha TK et al (2011) Pattern analysis of lymph node metastasis and the prognostic importance of number of metastatic nodes in ampullary adenocarcinoma. Am Surg 77:322–329
Sierzega M, Nowak K, Kulig J et al (2009) Lymph node involvement in ampullary cancer: the importance of the number, ratio, and location of metastatic nodes. J Surg Oncol 100:19–24
Kawabata Y, Tanaka T, Nishi T et al (2012) Appraisal of a total meso-pancreatoduodenum excision with pancreaticoduodenectomy for pancreatic head carcinoma. Eur J Surg Oncol 38:574–579
de Castro SM, van Heek NT, Kuhlmann KF et al (2004) Surgical management of neoplasms of the ampulla of Vater: local resection or pancreatoduodenectomy and prognostic factors for survival. Surgery 136:994–1002
Acharya A, Markar SR, Sodergren MH et al (2017) Meta-analysis of Adjuvant Therapy Following Curative Surgery for Periampullary Adenocarcinoma. Br J Surg 104(7):814–822
Valle J, Wasan H, Palmer DH et al (2010) Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med 362:1273–1281
Jin Z, Hartgers ML, Sanhueza CT et al (2018) Prognostic factors and benefits of adjuvant therapy after pancreatoduodenectomy for ampullary adenocarcinoma: mayo Clinic experience. Eur J Surg Oncol 44:677–683
Nassour I, Hynan LS, Christie A et al (2018) Association of adjuvant therapy with improved survival in ampullary cancer: a national cohort study. J Gastrointest Surg 22:695–702
Lee JH, Whittington R, Williams NN et al (2000) Outcome of pancreaticoduodenectomy and impact of adjuvant therapy for ampullary carcinomas. Int J Radiat Oncol Biol Phys 47:945–953
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
No.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
:The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all participants included in the study.
Statement of human rights
The study was approved by the institutional review board (J2019-130-2019-1), and each study subject provided their written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Matsui, S., Yamamoto, Y., Sugiura, T. et al. The Prognostic Relevance of the Number and Location of Positive Lymph Nodes for Ampulla of Vater Carcinoma. World J Surg 45, 270–278 (2021). https://doi.org/10.1007/s00268-020-05770-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05770-1