Abstract
Background
There is limited knowledge about the epidemiology of the major histological subtypes of appendiceal malignancy: adenocarcinoma and neuroendocrine neoplasm of the appendix (A-NEN). The aims of this national cohort study were to assess the prevalence, incidence and trends of appendiceal malignancies in Sweden.
Method
All individuals who underwent appendicectomy and all diagnosed with appendiceal malignancy from 1970 to 2012 were identified from the National Patient Register and the Swedish Cancer Registry. Demographic data of the background population were obtained from Statistics Sweden. The incidence rate (IR) and the prevalence of appendiceal malignancy per performed appendicectomy were calculated.
Results
We identified 3774 patients with appendiceal malignancy. IR of A-NEN was 5.8/106 person-years with a peak of 8.4/106 at age 20–30 years, whereafter it plateaued at a somewhat lower level. IR for adenocarcinoma was 3.7/106 person-years, starting at a very low level among the youngest and increasing to 15.4/106 at age 80–89 years. The IR of adenocarcinoma increased from 2.6/106 in 1970–1979 to 5.4/106 in 2010–2012. The IR of A-NEN was stable during the study period. The prevalence per appendicectomy was low for both types of malignancies among the young but increased with age, most dramatically for adenocarcinoma. There was a trend during the study period towards more extensive surgery.
Conclusion
Adenocarcinoma is most common and increasing in the elderly, whereas A-NEN affects all ages with a peak in young age. This peak probably reflects removal of occult A-NEN due to the higher appendicectomy frequency in the young.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignancies of the vermiform appendix are rare and heterogeneous. The two predominant histopathological subtypes are appendiceal neuroendocrine neoplasms (A-NEN) and adenocarcinoma, both with distinct biological behaviour [1, 2].
Current knowledge about the epidemiology of these malignancies is scarce. The estimated incidence of primary appendiceal malignancies varies enormously between 0.02 and 9.7 per million person-years in reports from USA, Iceland and the Netherlands [3,4,5,6,7,8,9]. There are indications that the incidence of both A-NEN and adenocarcinoma of the appendix has increased over the last decades [4, 5, 9, 10].
The majority of patients with appendiceal malignancies present with acute abdomen and many of them with a clinical presentation similar to acute appendicitis [1]. Routine histology of all appendix specimen is recommended as many cases are not discovered pre- and intraoperatively [11]. This may however lead to the diagnosis of incidental A-NEN with no clinical importance [3].
Appendiceal malignancies are rare, and most surgeons will have very limited experience of this disease. Appendiceal malignancy should be considered when selecting management strategy for patients with suspected appendicitis, especially since studies of conservative treatment with antibiotics for appendicitis have shown a high number of malignancies in these patients [4]. Knowledge of a patients risk for appendiceal malignancy augments the on-call surgeons capability of making sound clinical choices when managing patients with suspected appendicitis.
As some appendiceal malignancies may be of an incidental character, we hypothesize that the high incidence of appendectomies in children and young adults would have an impact on the incidence rate of those malignancies. The aims of this study were to assess the incidence and temporal trends of appendiceal malignancies in Sweden. We also analysed the age-specific prevalence of malignancy at appendicectomy in Sweden.
Methods
Study population
The Swedish National Board of Health and Welfare maintains the National Patient Register (NPR) and the Swedish Cancer Registry (SCR). These registers contain data on diagnoses and interventions for all hospital admissions and specialist outpatient visits as well as localization and histopathological characteristics of all malignancies diagnosed in Sweden. These registries can be linked using the national identification number that uniquely identifies all Swedish residents.
The SCR uses histology codes WHO/HS/CANC/24.1. Using the ICD-7 code 153.4 for the localization of the malignancy together with histology codes for neuroendocrine neoplasms (e086) and adenocarcinoma (e096) from the SCR, we identified a cohort of all patients in Sweden with a diagnosis of appendiceal neuroendocrine neoplasms (A-NEN) and appendiceal adenocarcinoma from 1970 to 2012. Adenocarcinoma (e096) includes adenocarcinomas regardless of growth pattern, including the rarer mucinous malignancies and Goblet cell adenocarcinomas (previously called Goblet cell carcinoid) [5]. A-NEN include mainly well-differentiated neuroendocrine tumours (A-NET), but also the rarer poorly differentiated neuroendocrine carcinomas (A-NEC) and mixed neuroendocrine–non-neuroendocrine neoplasms (MiNENs). These subgroups can be found using ICD-O3 codes, which were introduced in the SCR from 2005 and onwards.
All hospital admissions are recorded in the NPR with details on diagnoses, performed procedures and admission dates. Open and laparoscopic operations were defined using ICD-9 and ICD-10 codes as appendectomy (JEA00, JEA10, JEA01, 4510, 4511, 0058), ileocecal resection (JFB20, JFB21, 4642) and right hemicolectomy (JFB30, JFB31, 4641). Primary surgery was defined as the first registered operation in association with the cancer diagnosis. Secondary surgery was defined as completion of ileocecal resection or right hemicolectomy within 90 days after the primary operation.
Background and reference populations
Data on the composition of the Swedish population were obtained from the public database provided by Statistics Sweden [12]. Unless otherwise stated, all reported incidence rates are directly standardized for sex and age in 10-year intervals to the Swedish population during the study period. In addition, we estimated incidence rates with standardization to the US 2000 Standard Million population to allow comparisons with previous studies [13]. Incidence was illustrated graphically in 5-year intervals to give a more detailed picture.
For the estimation of the prevalence of appendiceal malignancies per appendicectomy, all patients in the NPR with an appendicectomy (procedural codes 4510, 4511, 4517, JEA00, JEA01, JEA10) from 1980 to 2012 were identified. As complete nationwide coverage of this register was reached only from 1987, only malignancies diagnosed in patients from areas that were fully covered by the register before 1987 were included in these estimates.
Statistical analysis
The incidence rates (IRs) of A-NEN and adenocarcinoma were estimated and adjusted for age, sex and year of diagnosis using direct standardization. Incidence-rate ratios (IRRs) were estimated using Poisson regression. The association of cancer stage with age was analysed by stratifying the patients in terciles of age. The correlation between cancer stage and age was tested using Fisher’s exact test and Kendall’s rank correlation test. Change in operative management over time was assessed with the Chi-square test. Statistical tests were two-sided, and a p value of less than 0.05 was considered to indicate statistical significance.
Stata 15.1 (StataCorp, College Station, TX, USA) was used for all statistical analysis.
Results
A total of 3774 patients with appendiceal malignancy diagnosed between 1970 and 2012 were identified from the registries. After exclusion of 236 patients with histology codes other than e096 or e086, the study included 2171 patients with A-NEN and 1367 with adenocarcinoma. Using ICD-O3 codes, we identified 15 Goblet cell adenocarcinomas (3.6% of adenocarcinomas) as well as 16 MiNENs (3.4% A-NEN) diagnosed from 2005 and onwards.
This corresponds to IR 5.8 for A-NEN and 3.7 for adenocarcinoma per million person-years, respectively, for the whole study period (Table 1). The overall IR standardized to the US 2000 Million Standard population was 5.7 and 3.1 per million person-years, respectively. The incidence of A-NEN was unchanged during the study period, whereas IR of adenocarcinoma increased from 2.6/106 to 5.4/106 (p < 0.001) (Table 1).
Age- and sex-specific incidence rate
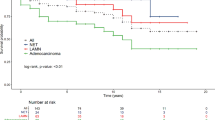
A-NEN was more common in women (IR 7.5/106) than in men (IR 4.2/106; p < 0.001), while the incidence of adenocarcinoma did not differ between men and women (IR 3.6/106 and 3.7/106, respectively; p = 0.482) (Table 1). Two distinctly different patterns of age-specific IR were observed between the malignancy types (Fig. 1). A-NEN occurred in all ages with a peak incidence at age 20–29 years (8.4/106). By contrast, adenocarcinoma was non-existent in childhood whereafter the incidence increased steadily with age reaching its top level at age 80–89 years (15.4/106).
Prevalence per appendicectomy
Appendicectomy was performed in 381,858 patients between 1980 and 2012. Appendiceal malignancy was diagnosed in 2937 (0.8%) patients, equalling a prevalence of one malignancy per 130 appendicectomies. The age-specific prevalence of A-NEN per appendicectomy increased slowly starting already at the lowest ages (Fig. 2). Adenocarcinoma was an uncommon finding per appendicectomy among patients under 30 years at which point the prevalence started to increase more rapidly. Both subtypes have its highest prevalence in the age interval 85–89 years.
Cancer stage by age
Cancer stage was recorded consistently from 2005 and onwards. Full TNM classification was available from 180 patients with A-NEN and 362 patients with adenocarcinoma. Advanced malignancies (stages III and IV) were more common in adenocarcinoma than in A-NEN (p < 0.001). For A-NEN, there was a significant trend towards higher stage at diagnosis with increasing age. For the youngest tercile, 71.4% of the malignancies were stage I, and 28.6% were stage II or higher. The corresponding figures for the oldest quantile were 45.5% and 54.5%, respectively (Kendall's tau-b = 0.214, p < 0.001). For adenocarcinoma, the distribution did not differ between the quantiles of age (Kendall's tau-b = -0.032, p = 0.883) (Table 2).
Trends in operative management
Appendectomy was the most common primary operation for A-NEN during the whole study period (88.0% of all primary operations) with ileocecal resection (5.8%) and right hemicolectomy (6.3%) being less common (Table 3). Most patients with appendiceal adenocarcinoma also underwent appendectomy initially (58.6% of all primary operations), but ileocecal resection (18.3%) and right hemicolectomy (23.1%) were relatively more common than for A-NEN. Most patients with either A-NEN (91.1%) or adenocarcinoma (76.4%) did not undergo further surgery beyond the first operation. The proportion of patients that had ileocecal resection as primary surgery decreased, while the proportion that had right hemicolectomy increased over time for both A-NEN (p = 0.003) and adenocarcinoma (p = 0.041). A similar temporal trend was observed for secondary operations for both A-NEN (p < 0.001) and adenocarcinoma (p < 0.001).
Discussion
This study, spanning over 5 decades, is one of few national population-based studies of the epidemiology of appendiceal malignancies [3, 8, 10]. The results indicate a slightly higher incidence of both A-NEN and adenocarcinoma in Sweden compared to other countries [5, 9, 10]. In keeping with other studies, we noted a rising incidence rate of adenocarcinoma during the study period [4, 5]. Unlike previous reports, the incidence of A-NEN remained unchanged [5, 9, 10]. An increased use of colonoscopy and diagnostic imaging as well as routine histopathological examination after appendicectomy could contribute to an increasing incidence rate due to a higher detection rate [4, 5, 14]. Since appendectomy eliminates the risk of future appendiceal malignancy, a lower incidence of appendectomy could contribute to an increasing incidence of appendiceal malignancy. The frequency of appendectomy in Sweden was around 240 cases/100.000 person-years from the 1920s till the 1980s [15, 16], but has since steadily decreased mainly in children and young adults, reaching 120 cases/100.000 in recent years [17]. As a consequence, the population at risk is larger in recent decades which may have contributed to an increasing incidence rate. This effect should be limited in view of the small proportion of the population that undergoes appendectomy. Another possible reason for bias is the proportion of appendectomies that undergo histopathological examination, which may have changed during the long study period. Unfortunately, we do not have any information on that factor.
There was a striking difference in age distribution between the two types of malignancy. Adenocarcinoma of the appendix follows the pattern of most other gastrointestinal cancers and is virtually non-existent among children and young adults but becomes increasingly common from 30 years of age. The prevalence of adenocarcinoma per excised appendices follows the same pattern as the incidence rate, steadily increasing with age. By contrast, the incidence rate of A-NEN reaches its highest level in young adults. However, the prevalence of A-NEN per excised appendices is low in children and young adults but increases with age to reach its highest level at age 85. These seemingly contradicting findings between the incidence rate and the prevalence are explained by the age distribution of appendicectomy which has a peak in children and young adults and the fact that A-NEN commonly is an incidental finding in younger patients [1, 16]. The high incidence rate of A-NEN in young persons may thus be mainly explained by the higher sampling frequency. This hypothesis is further corroborated by the finding that a majority of A-NEN in young patients were stage I or II.
Appendiceal malignancy is uncommon in the general population but considering only patients undergoing appendicectomy the prevalence rises sharply from age 40 to reach high levels in octogenarians. In this group, one adenocarcinoma is diagnosed in every 20 appendicectomies. The current recommendation is to send all appendectomy specimens for histopathological examination for safety reasons [11]. Deviations from this recommendation are however common, mainly due to the scarcity of histopathological service. Different frequencies of histopathological examination may explain the great variation of incidence rates in the literature. In our study, 71% of patients with A-NEN who were younger than 29 years had a stage 1 malignancy. According to guidelines, these malignancies have little to no clinical impact since most of these cases require no further treatment or follow-up [18]. When assessing the utility of routine histopathology for appendectomy specimen, this needs to be taken into account. The results of the present study may be used in cost-utility analysis to develop more practical guidelines.
The surgical management has become more aggressive over time with more extensive surgery both at the primary and the secondary operation, especially in patients with adenocarcinoma. Compared to A-NEN, adenocarcinomas are more commonly advanced upon presentation which could necessitate more extensive primary surgery. Right hemicolectomy is considered standard treatment for adenocarcinomas. As the diagnosis can be unclear at the primary operation, secondary operations may be needed after the histopathological diagnosis is established [19]. It should be noted that the survival benefit from right hemicolectomy has been questioned for patients with A-NEN, and benefit has only been shown in adenocarcinomas and only when 12 or more lymph nodes are retrieved [20].
Strengths and weaknesses
Strengths of this study include the high quality and coverage of the national registries, resulting in an almost complete population-based study with a long inclusion period and a large cohort. However, as with any registry study, clinical details of each patient were unavailable. A few developments have occurred in the classification of appendiceal tumours during the study period. Goblet cell adenocarcinomas and mucinous adenocarcinomas cannot be reliably separated from each other in the SCR before the introduction of ICD-O3 codes in 2005 and are therefore included in the adenocarcinoma cohort throughout the study period. For the same reason, occasional MiNENs are included in the A-NEN cohort. Due to their rarity, this probably makes little difference to the interpretation of the study overall. A further limitation was the restricted data on TNM stage. Unless all removed appendices are sent for histopathology, there will always be some uncertainty regarding the “true” incidence of malignancy. There are currently no available records showing the rate of histopathological examination for appendicectomy specimen in Sweden.
Conclusion
Adenocarcinoma of the appendix has steadily become more frequent since the 1970s. The incidence of adenocarcinoma increases with age, whereas A-NEN primarily affect younger patients. This is probably a consequence of the incidental detection of occult A-NEN due to the higher appendicectomy frequency in the young. The surgical management has become more aggressive over time with more extensive surgery both at the primary and the secondary operation, especially in patients with adenocarcinoma.
References
Tang LH (2010) Epithelial neoplasms of the appendix. Arch Pathol Lab Med 134:1612–1620
Misdraji J (2010) Appendiceal mucinous neoplasms: controversial issues. Arch Pathol Lab Med 134:864–870
McCusker ME, Coté TR, Clegg LX et al (2002) Primary malignant neoplasms of the appendix: a population-based study from the surveillance, epidemiology and end-results program, 1973–1998. Cancer 94:3307–3312
Turaga KK, Pappas SG, Gamblin T (2012) Importance of histologic subtype in the staging of appendiceal tumors. Ann Surg Oncol 19:1379–1385
Marmor S, Portschy PR, Tuttle TM et al (2015) The rise in appendiceal cancer incidence: 2000–2009. J Gastrointest Surg 19:743–750
Mullen JT, Savarese DM (2011) Carcinoid tumors of the appendix: a population-based study. J Surg Oncol 104:41–44
Nielsen GP, Isaksson HJ, Finnbogason H et al (1991) Adenocarcinoma of the vermiform appendix. A population study. APMIS 99:653–656
Smeenk RM, van Velthuysen ML, Verwaal VJ et al (2008) Appendiceal neoplasms and pseudomyxoma peritonei: a population based study. Eur J Surg Oncol 34:196–201
Dasari A, Shen C, Halperin D et al (2017) Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol 3:1335–1342
Ellis L, Shale MJ, Coleman MP (2010) Carcinoid tumors of the gastrointestinal tract: trends in incidence in England since 1971. Am J Gastroenterol 105:2563–3569
Swank HA, Eshuis EJ, Ubbink DT et al (2011) Is routine histopathological examination of appendectomy specimens useful? A systematic review of the literature. Colorectal Dis 13:1214–1221
Statistics CBo (2017) Statistikdatabasen. https://www.statistikdatabasen.scb.se/pxweb/sv/ssd/START__BE__BE0101__BE0101A/BefolkningR1860/?rxid=6fe9e41d-f130-44da-928b-43eb297669b3. Accessed 21 Aug 2018
Surveillance E, End Results program. Standard populations—19 age groups. https://seer.cancer.gov/stdpopulations/stdpop.19ages.html. Accessed 21 Aug 2018
van den Heuvel MG, Lemmens VE, Verhoeven RH et al (2013) The incidence of mucinous appendiceal malignancies: a population-based study. Int J Colorectal Dis 28:1307–1310
Nyström G (1932) Wachsende appendicitismortalität. Acta Chir Scand 72:236–260
Andersson R, Hugander A, Thulin A et al (1994) Indications for operation in suspected appendicitis and incidence of perforation. BMJ 308:107–110
The Swedish National Board of Health and Welfare. National Patient Register. Cited 07 July 2020
Pape UF et al (2016) ENETS consensus guidelines for neuroendocrine neoplasms of the appendix (Excluding goblet cell carcinomas). Neuroendocrinology 2016(103):144–152
Hatch QM, Gilbert EW (2018) Appendiceal neoplasms. Clin Colon Rectal Surg 31:278–287
Fleischmann I et al (2017) Improved survival after retrieval of 12 or more regional lymph nodes in appendiceal cancer. Eur J Surg Oncol 43:1876–1885
Funding
This study was supported by Futurum, Academy for Health and Care, Region Jönköping County, Sweden.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
The study was approved by the Regional Ethical Review Board at Linköping University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Johansson, J., Andersson, R.E., Landerholm, K. et al. Incidence of Appendiceal Malignancies in Sweden Between 1970 and 2012. World J Surg 44, 4086–4092 (2020). https://doi.org/10.1007/s00268-020-05758-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05758-x