Abstract
Background
Access to safe and effective surgery is limited in low and middle-income countries. Short-term surgical missions are a common platform to provide care, but the few published outcomes suggest unacceptable morbidity and mortality. We sought to study the safety and effectiveness of the ApriDec Medical Outreach Group (AMOG).
Methods
Data from the December 2017 and April 2018 outreaches were prospectively collected. Patient demographics, characteristics of surgery, complications of surgery, and patient quality of life were collected preoperatively and on postoperative days 15 and 30. Data were analyzed to determine complication rates and trends in quality of life.
Results
260/278 (93.5%) of patients completed a 30-day follow-up. Of these, surgical site infection was the most common complication (8.0%), followed by hematoma (4.1%). Rates of urinary tract infection were 1.2% while all other complications occurred in less than 1% of patients. There were no mortalities. With increasing time after surgery (0 to 15 days to 30 days), there was a significant improvement across each of the dimensions of quality of life (p < 0.001). All patients reported satisfaction with their procedure.
Conclusion
This study demonstrated that the care provided by AMOG group to the underserved populations of northern Ghana, yielded complication rates similar to others in low-resourced communities, leading to improved quality of life.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgical missions are among varied efforts to expand access to the estimated 5 billion people who lack timely access to safe, affordable surgical care [1]. Of the 313 million procedures undertaken worldwide each year, only 6% occur in the poorest countries, where one-third of the population lives. Even when access is available, patients in low-resource settings have limited ability to pay for care and appropriate follow-up. In fact, each year 81.3 million people suffer from catastrophic health expenditure secondary to the cost of surgery [2]. As surgical infrastructure, workforce, and financing efforts are escalated, humanitarian efforts strive to improve or provide access to fulfill unmet surgical needs. Different charitable platforms include disaster relief, short-term surgical trips, self-contained surgical platforms, and specialty surgical hospitals [3, 4]. The most common charitable platform is the short-term surgical mission.
Although surgical missions strive to provide charitable care to patients who experience barriers in accessing care, there exists considerable controversy regarding the efficacy, safety, cost-effectiveness, and sustainability of their efforts [3,4,5,6]. Nearly 95% of publications on surgical missions lack any data collection, making systematic review difficult [5]. However some analyses suggest morbidity and mortality that is 20 times greater than the same procedure in high-income countries [7]. Although not risk-adjusted, available data underlines poor quality care that is unacceptable to healthcare providers and patients, alike. Given the paucity of data, groups involved in charitable care should be encouraged to conduct their work in an ethically and responsible way, including the collection and sharing of patient experience and outcomes.
The ApriDec Medical Outreach Group (AMOG) is a Ghanaian-based non-governmental and non-profit organization that has been providing outreach surgical and medical services to under-resourced communities in northern Ghana since 2010. AMOG works closely with the Ghana Health Service and the Regional Director of Health Services to identify local needs and coordinate visits. Previous reports demonstrated the cost-effectiveness of AMOG [8].This study examines the safety and effectiveness of AMOG using prospectively collected outcomes data as well as patient surveys and quality of life metrics.
Material and methods
Setting
AMOG travels to the three northern regions in Ghana, usually twice a year to provide surgical care, on-site skills training, and continuous medical education. Since 2014 they have travelled to the Upper East Region and Upper West Regions on a yearly basis in April and December, respectively. AMOG volunteers work closely with local health care providers, regional health directorates, and community leaders to produce radio announcements and pamphlets to recruit patients needing surgical care. Patients are screened by local medical officers and prepared for surgery with the guidance of AMOG staff. During AMOG visits, the scope of practice was determined by AMOG staff in collaboration with local providers. Any condition that required advanced post-operative care were referred to regional tertiary centers. AMOG medical volunteers include surgeons of various specialties, surgical residents, nurse anesthetists, anesthesiologists, theater nurses, pharmacists, and other health professionals. All services were rendered with no cost to patients.
In addition to providing patient care, AMOG strives to build medical and surgical capacity through education with local providers. The group generally works with the same colleagues during each visit, leading to long-lasting collaboration and relationships.
Data collection
During the December 2017 outreach to the Upper East Region and April 2018 outreach to the Upper West Region, we performed a prospective assessment of surgical outcomes and patient quality of life metrics. All patients receiving surgical care were considered except patients unwilling to participate in the study who were excluded. Care rendered was not impacted by participation in the study. After consent, patients were interviewed by local or AMOG staff to obtain basic information on demographics along with perioperative information. Patient follow-up was arranged by a local operative nurse for postoperative day 15 and 30 days. Nurses were educated on how to recognize complications and encouraged to contact the local medical officer or AMOG staff for any uncertainty. Complications were managed by local operative nurses and medical offers and none required referrals for advanced care. Nurses and staff at each site were issued 200 GHS ($36) by AMOG to use at their discretion to facilitate patient follow-up, purchase supplies for wound care, and to compensate for their extra efforts.
Definitions
Complications were recorded as a binary yes or no, using the following outcomes: surgical site infection, hematoma, pneumonia, cardiac complication, urinary tract infection, venous thromboembolism, renal failure, unplanned return to the operating room, and death. Complications were defined according to the American College of Surgeons National Surgical Quality Improvement Program [9].
To measure quality of life, we used the validated EQ-5D-5L tool [10] after receiving permission from the EuroQol Research Foundation. This descriptive tool measures patient health across five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each health state is then divided into five levels of perceived problems:
Level one: indicating no problem
Level two: indicating slight problems
Level three: indicating moderate problems
Level four: indicating severe problems
Level five: indicating extreme problems
In addition, patients ranked their health on a scale of 0 to 100, where 0 means the worst health they could imagine and 100 meaning the best health imaginable. We asked patients to rate their overall level of health and across the five dimensions at three times: before surgery, postoperative day 15, and postoperative day 30.
Analysis
Analyses were conducted with Stata v14 (StataCorp, College Station, TX). Data were presented as mean ± standard deviation, as appropriate. Chi-square test was used to evaluate changes in patient responses regarding different dimensions of QoL.
Results
During the December 2017 and April 2018 outreaches, 278 operations were performed with all patients willing to participate and 260 (93.5%) patients completing 30 days of follow-up. Patients reported coming from homes with 8 or greater people (39.1%), while 24.6% and 27.0% reported living with 6–7 and 4–5 people, respectively (Table 1). Most patients reported a household yearly income of less than 2000 GHS ($360). Fifty-three percent had no formal education while 25.8% reported either starting or completing primary education. Cost of surgery was the most commonly reported barrier to necessary surgical care (63.8%).
Nine hospitals participated in the AMOG outreaches in 2018. Inguinal hernia repairs were the most common procedure (43.6%), followed by soft tissue excision biopsy (16.2%), other general surgery cases (10.7%), hysterectomy (8.1%), and obstetrics cases (7.3%) (Table 2).
Surgical site infection was the most common complication (8.0%), followed by hematoma (4.1%). Two patients (0.8%) had a cardiac complication (details not specified), three patients developed UTIs (1.2%), two patients had unplanned returns to the OR (0.8%), and one patient experienced both pneumonia and venous thromboembolism (Table 3). No deaths occurred. Of patients receiving surgery, 27 (11.6%) had at least one of the measured complications. The majority of wound complications occurred within the first 15 days, while other complications occurred throughout the 30-day period.
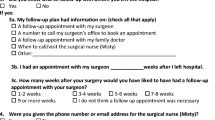
Figure 1 demonstrates patient-reported quality of life per EQ-5D-5L across five dimensions. With increasing time postoperative (0 to 15 days to 30 days), there was a significant shift towards improving quality of life across each of the dimensions of quality of life (p < 0.001).
The 100% stacked bar charts demonstrating the distribution of responses to the EQ-5D-5L by dimensions. With increasing time postoperative (0 to 15 days to 30 days), there was a significant shift towards improving quality of life across each of the dimensions of quality of life (p < 0.001). POD = post-operative day
On a scale of 0–100, patients rated their overall health as a median 70 out of 100 (interquartile range 60–100). On postoperative day 15 this had risen to 80 (IQR 70–100) and then to 90 (IQR 90–100) by postoperative day 30. All patients reported that they were glad to have received surgery on their postoperative visits.
Discussion
The role of surgical outreach groups in providing access to underserved areas is not well-characterized, with existing evidence suggesting poor outcomes [3,4,5,6,7]. We believe there is a role for thoughtful and ethical outreach to expand access as global surgical capacity increases. This study demonstrates that the AMOG group provided care to underserved populations in northern Ghana, with complication rates comparable to others in low-resourced areas, and improved quality of life for the care rendered.
AMOG’s mission is to improve access to quality specialized healthcare services in the most deprived communities in Ghana [11]. 61.2% of patients operated upon reported a household income of less than 2,000 GHS ($380) per year, which is below the poverty rate for an individual’s income defined by The World Bank [12]. Given that the majority of patients (63.7%) reported living with 6 or more people in their home, most families served by AMOG are well below the poverty rate. In these impoverished communities it is not surprising that the largest perceived barrier to receiving surgery was cost. It is notable that many patients in northern Ghana should be covered by the National Health Insurance Scheme (NHIS), which strives to cover necessary medical care without shared cost [13]. As the most commonly cited barrier to receiving necessary surgical care was cost, this goal has not been achieved in northern Ghana. Our patients’ perception that necessary surgical care comes at a cost is consistent with previous observations at Tamale Teaching Hospital [14]. Until care can be rendered without cost, the work of AMOG serves an important function in providing care to the deprived communities in northern Ghana.
Even when delivering free surgical care, clinicians should ensure safe and effective services. It is therefore essential that outreach groups monitor their outcomes to ensure acceptability. The most common complication experienced by AMOG was SSI (9.1%), followed by hematoma (4.7%). Although the majority of cases were considered clean, 50.5% were hernia repairs and hydrocelectomies. The groin may be particularly prone to infection with rates of SSI exceeding those from other clean cases, as demonstrated by an 8.7% SSI rate in high-risk environments [15], and rates higher than 10% in some high-risk settings [16, 17]. Previous surgical missions in Ghana reported an overall complication rate of 6.1%, with 4.4% of patients returning with hematoma and 1.7% with wound infections [18]. Mitura et al. reported a lower rate of wound infection, at 1% [19]. Most recently Yenli et al. reported a scrotal hematoma rate of 6.7% and surgical site infection rate of 2.9% [20]. However, these previous studies relied on patients calling to report postoperative complications [18, 19] or involved patient phone calls [20] to gather data, likely leading to an underestimation. To our knowledge, no previous groups in Ghana have assessed 15- and 30-day outcomes using in-person follow-up. Therefore we believe that a 9.1% rate of SSI is accurate and suggests an area for improvement. Rates of other complications were low. During two outreaches, we experienced no mortalities. To our knowledge, there have been no mortalities attributed directly to surgery since AMOG was established in 2010. Therefore it seems AMOG’s mortality is below previous estimates for elective and emergent cases in LMICS, 5.4 and 21% respectively [21].
While minimizing complications is critical, measures to ensure safe surgery are the ultimate goal of AMOG is to improve the lives of patients. The EQ-5D-5L is a widely used patient-reported outcome measure to assess patient QoL after surgery. There was a significant improvement across all dimensions of QoL at POD 30. It is interesting to note that patients experienced a non-significant worsening of pain and mobility on POD 15, compared to preoperatively. We believe this finding is secondary to normal incisional pain that subsequently resolved. A reported slight worsening of pain is also reassuring that patients were honest in their reporting of symptoms. Of course, these results can only hint at the true impact on QoL that essential surgical care can confer. It has been our experience that, for example, the repair of a large inguinoscrotal hernia or hysterectomy for debilitating fibroid pain are life-altering procedures that allow young men and women to return to work or care for their families.
Not captured in our study is the broader effect of the AMOG outreaches. AMOG provides surgical services but also strives to build local surgical capacity. Surgeons often train the local medical officers and other healthcare professionals, refreshing lessons learned during training or imparting new skills. For example, before AMOG visits, most local physicians were not trained in tension-free repairs of hernias using synthetic mesh. Local physicians have subsequently been trained and perform these procedures unassisted. AMOG operative nurses assist local staff with setting up the operating theatre, teach concepts of sterility, and provide lessons on operative assistance. In this way, the impact of AMOG’s efforts extend beyond the time of outreach. AMOG also brings other medical specialists, biomedical engineers, and public health clinicians to support local capacity. While this study strives to measure the impact of AMOG on patients, its effect on local surgical capacity is an important topic for future investigation.
Our QoL metrics relied on responses from patients. Although there was no way to verify their responses, we have no reason to believe that they would be hesitant to report unchanged or worsened symptoms after receiving treatment. Further, our rates of complications are not remarkably low, which would have suggested biased responses. We therefore believe that patients were honest in their responses. More accurate rates of SSI and hematoma could be improved by cell phone photography. The main limitation of our study is generalizability to other surgical outreach groups as there is great heterogenicity in this model of health care delivery. However we demonstrate that surgical outreaches can be performed responsibly by local national outreach from urban centers to rural settings. We encourage other short-term surgical missions to collaborate with local teams to integrate evaluation of postoperative outcomes into their processes. Post-surgical follow-up is necessary to ensure that surgical care to underserved communities in LMICs is safe and effective.
References
Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA et al (2015) Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386(9993):569–624
Shrime MG, Dare AJ, Alkire BC, O'Neill K, Meara JG (2015) Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob Health 3(Suppl 2):S38–S44
Shrime MG, Sleemi A, Ravilla TD (2015) Charitable platforms in global surgery: a systematic review of their effectiveness, cost-effectiveness, sustainability, and role training. World J Surg 39(1):10–20
Kynes JM, Zeigler L, McQueen K (2017) Surgical outreach for children by international humanitarian organizations: a review. Children 4(7):53
Sykes KJ (2014) Short-term medical service trips: a systematic review of the evidence. Am J Public Health 104(7):e38–e48
Zitzman E, Berkley H, Jindal RM (2018) Accountability in global surgery missions. BMJ Glob Health 3(6):e001025
Poilleux J, Lobry P (1991) Surgical humanitarian missions. An experience over 18 years. Chirurgie; memoires de l'Academie de chirurgie 117(8):602–606
Gyedu A, Gaskill C, Boakye G, Abantanga F (2017) Cost-effectiveness of a locally organized surgical outreach mission: making a case for strengthening local non-governmental organizations. World J Surg 41(12):3074–3082
American College of Surgeons National Surgical Quality Improvement Program (2016) User Guide for the 2015 ACS NSQIP Participant Use Data File (PUF)
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D et al (2011) Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Quality Life Res Int J Qual Life Asp Treat Care Rehabil 20(10):1727–1736
Cooke C, Hague S, McKay A (2016) The Ghana poverty and inequality report: Using the 6th Ghana living standards survey. Unicef, University of Sussex, Ashesi University College
The World Bank. Understanding Poverty. The World Bank; [updated 2019; cited 2018 August 5]. Available from: https://www.worldbank.org/en/topic/poverty/overview
Wang H, Otoo N, Dsane-Selby L (2017) Ghana national health insurance scheme: proving financial sustainability based on expenditure review. World Bank Group, Washington, DC
Tabiri S, Jalali A, Nelson RE, Damah MC, Abantanga FA, Price RR et al (2019) Barriers to timely presentation of patients with surgical conditions at Tamale Teaching Hospital in Northern Ghana. World J Surg 43(2):346–352
HerniaSurge G (2018) International guidelines for groin hernia management. Hernia J Hernias Abdom Wall Surg 22(1):1–165
Bailey IS, Karran SE, Toyn K, Brough P, Ranaboldo C, Karran SJ (1992) Community surveillance of complications after hernia surgery. BMJ 304(6825):469–471
Othman I (2011) Prospective randomized evaluation of prophylactic antibiotic usage in patients undergoing tension free inguinal hernioplasty. Hernia J Hernias Abdom Wall Surg 15(3):309–313
Shillcutt SD, Clarke MG, Kingsnorth AN (2010) Cost-effectiveness of groin hernia surgery in the Western Region of Ghana. Arch Surg 145(10):954–961
Mitura K, Koziel S, Pasierbek M (2015) Groin hernia surgery in northern Ghana–humanitarian mission of Polish surgeons in Tamale. Polski Przeglad Chirurgiczny 87(1):16–21
Yenli EMT, Abanga J, Tabiri S, Kpangkpari S, Tigwii A, Nsor A et al (2017) Our experience with the use of low cost mesh in tension-free inguinal hernioplasty in Northern Ghana. Ghana Med J 51(2):78–82
Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN (eds) (2015) Essential surgery: disease control priorities, vol 1, 3rd edn. World Bank, Washington, DC
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
MK, ST, RP, and FA designed the study and facilitated collection of data. AG performed statistical analysis. MK, ST, AG, RP and FA contributed to drafting the manuscript and provided critical revision for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study received approval by both the Ghana Health Service and University of Utah Institutional Review board committees.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Katz, M.G., Tabiri, S., Gyedu, A. et al. Patient Experience and Outcomes of the Locally Organized ApriDec Medical Outreach Group. World J Surg 44, 1039–1044 (2020). https://doi.org/10.1007/s00268-019-05288-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05288-1