Abstract
Background
Pheochromocytoma with synchronous ipsilateral adrenal cortical adenoma (PSCA) may present with mixed clinical, biochemical, and radiological features characteristic to each neoplasm subtype.
Methods
All patients with a pathological diagnosis of pheochromocytoma were evaluated for an ipsilateral cortical adenoma from 1994 through 2015. Retrospectively extracted data included indications for adrenalectomy, diagnostic workup (biochemical and radiographic), operative characteristics, pathological findings, and postoperative complications.
Results
Sixteen of 413 patients (4%) undergoing adrenalectomy for pheochromocytoma had a PSCA. Median patient age was 57.7 years (IQR 50.1, 63.1); 50% were male. On imaging, 75% of the adrenal neoplasms were found incidentally and only 50% were reported to have a synchronous ipsilateral neoplasm based on imaging findings. Clinically important cortical hormone secretion was diagnosed in 38% of these patients; 25% had glucocorticoid secretory autonomy; and 13% had primary aldosteronism.
Conclusion
Physicians should be aware that adrenal neoplasms with mixed diagnostic findings may represent PSCA. Evaluation should be performed on this co-occurrence to prevent perioperative complications from resection of an unexpected secretory cortical neoplasm.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The majority of adrenal masses are discovered incidentally through imaging for reasons unrelated to adrenal diseases [1, 2]. These incidentalomas may be adrenal cortical adenomas, pheochromocytomas, or potentially both neoplasm types presenting synchronously. When an adrenal gland presents with both cortical and medullary neoplasms, diagnostic workup and perioperative care can be challenging due to the combined characteristics specific to each tumor subtype. For example, resection of an unexpected glucocorticoid-secreting cortical neoplasm, even when subclinical, during adrenalectomy for pheochromocytoma can lead to postoperative adrenal insufficiency if not diagnosed and treated appropriately. Conversely, patients undergoing evaluation for primary aldosteronism may precipitate a hypertensive crisis during adrenal venous sampling if catecholamine excess was not diagnosed prior to the procedure. Given the clinical significance of this co-occurrence, it is imperative that the incidence and characteristics of the concomitant entity be accurately reported. However, the simultaneous occurrence of pheochromocytoma and adrenal cortical adenoma has been previously reported only via isolated case reports [3,4,5,6,7,8,9,10,11,12]. Heterogeneity in this published data makes it difficult to decipher useful and generalizable information to be applied in clinical practice. We aimed to review our experience at a large tertiary referral center to better understand the clinical and perioperative characteristics of this clinical entity. We report a case series of 16 patients with pheochromocytoma and synchronous cortical adenoma (PSCA). Our study aims to describe the incidence, clinical characteristics, diagnostic evaluation, and surgical management of this co-occurrence.
Materials and methods
The study was reviewed and approved by the Mayo Foundation Institutional Review Board. All patients ≥18 years of age with a pathological diagnosis of pheochromocytoma from January 1, 1994, through June 30, 2015, were identified using an institutional surgical pathology specimen database. The final pathology report of each patient with a pheochromocytoma was reviewed for the presence of a synchronous ipsilateral adrenal cortical adenoma. The medical record of each patient with PSCA was reviewed. Retrospectively collected data included indications for adrenalectomy, diagnostic workup (biochemical and radiographic), operative characteristics, pathological findings with immunohistochemical studies, and postoperative management and complications. Patients with mixed corticomedullary tumors, cortical hyperplasia without glandular features, cortical adenoma size less than 3 mm, contralateral tumors without ipsilateral synchronization, and patients diagnosed with each entity (pheochromocytoma and cortical adenoma) at separate times were excluded. Figure 1 summarizes the patient search strategy.
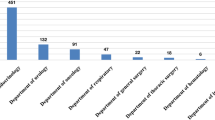
Results
In total, we identified 16 cases of PSCA among 413 patients (4%) who underwent adrenalectomy for pheochromocytoma. Patient characteristics are summarized in Table 1. Mean patient age at diagnosis and surgery was 57 years (SD 29–78); 50% were male. Median BMI was 28.5 kg/m2 (IQR 26.8, 30.8). The preoperative presumptive diagnosis included nine pheochromocytomas (56%), four cortical adenomas (25%), and three PSCA (19%).
Patient presentation
The clinical presentation was variable (Table 1), with paroxysmal clinical symptoms of a pheochromocytoma documented in 13 (81%) patients. At the time of clinical evaluation, six patients (38%) presented with headache, seven (44%) with sweating, eight (50%) with palpitations, and five (31%) with tachycardia. Paroxysmal hypertension was diagnosed in ten patients (63%), whereas sustained hypertension was diagnosed in nine patients (56%). Two patients (13%) had diabetes mellitus and six (38%) had dyslipidemia. Two patients (13%) had hypokalemia. Significant weight loss (defined as loss of 5% or more of usual body weight over 6 months) was seen in three patients (19%), whereas one (7%) had weight gain (defined as gain of 5% or more of usual body weight over 6 months). No patient presented with clinical stigmata of Cushing syndrome or androgen excess. Median time from diagnosis to surgery was 1.0 months (range 0.2–30.8). One patient had a family history of pheochromocytoma, and none had a family history of cortical adenoma. Genetic testing was positive in three of five total patients tested. Diagnoses included multiple endocrine neoplasia (MEN) type 1, MEN-2A, and neurofibromatosis type 1 (NF1).
Imaging characteristics
In 12 cases (75%), the initial primary neoplasm was found incidentally on imaging for an unrelated issue (nephrolithiasis, diverticulitis, acute abdomen, etc.). Only eight cases (50%) were reported on imaging to have a synchronous ipsilateral neoplasm. Three cases (19%) had an additional contralateral neoplasm. The most common method of detection for PSCA was an incidental finding on computed tomography (CT) scan (75%), followed by intentional CT attempting to identify adrenal neoplasms (19%) and incidental finding on ultrasound (7%). Other modalities of imaging included magnetic resonance imaging (MRI, 44%) and 123-I-metaiodobenzylguanidine scintigraphy (MIBG scan, 38%). Adrenal mass radio densities were above 20 Hounsfield units (HU) in eight patients with unenhanced CT scans (73%) and below 10 HU in two patients (18%). Mean increase in size per year during monitoring was 0.8 cm (min 0.01, max 3.0).
Biochemical evidence
Biochemical results for patients with PSCA are summarized in Table 2. Four patients (25%) were diagnosed preoperatively with clinically relevant autonomous cortisol overproduction. Two patients (13%) were diagnosed preoperatively with primary aldosteronism and both underwent adrenal venous sampling (AVS). Both of these patients developed a hypertensive crisis during AVS.
Perioperative management and outcomes
The initial surgical approaches were laparoscopic (81%), open (13%), and retroperitoneoscopic (6%). All but two patients (88%) had alpha-adrenergic blockade prior to surgery, six patients (38%) had beta-adrenergic blockade, and two (13%) had calcium channel blockade. Of the four patients diagnosed preoperatively with only cortical adenomas, only two (50%) had alpha-adrenergic blockade before surgery due to borderline catecholamine levels and mixed imaging findings. Median hospital stay was 2.5 days (range 2–6). Intraoperative blood pressures included a median maximum systolic pressure of 173 mmHg (range 138–289 mmHg), median minimum systolic pressure of 83 mmHg (range 52–140 mmHg), median maximum diastolic pressure of 94 mmHg (range 70–155 mmHg), and median minimum diastolic pressure of 47 mmHg (range 28–80 mmHg). The median maximum intraoperative heart rate was 106 bpm (range 70–151 bpm) and the median minimum was 49 bpm (range 20–81 bpm). One laparoscopic operation was converted to open due to intraoperative hemorrhage. No patient required blood transfusion, postoperative vasopressor support, an intensive care unit stay, reoperation, or readmission within 30 days. There was no other major morbidity and no mortality within 1 year found in the available medical record. Postoperative management included beta-adrenergic blockers in five patients (31%), alpha-adrenergic blockers in two (13%), and a calcium channel blocker in one (7%). Five patients (31%) were placed on steroid tapers postoperatively. One patient known to be RET oncogene positive returned with a recurrent pheochromocytoma on the contralateral side within 5 years.
Pathological characteristics
Gross pathological evaluation revealed mean pheochromocytoma size was 2.7 cm (range 0.8–4.8) and mean cortical adenoma size was 1.8 cm (range 0.3–4.4). Eleven (69%) of the masses were found on the patient’s right side. Gross specimens were typically characterized by two distinct lesions (Fig. 2): one in the adrenal medulla that was reddish brown and soft (pheochromocytoma) and the other in the adrenal cortex that was yellow and firm (cortical adenoma). Histologically, all tumors had microscopic characteristics within the expected pathological range for both cortical adenomas and pheochromocytomas.
Gross specimen of pheochromocytoma and synchronous cortical adenoma. The gross image discloses a 9.5 g, 5.2 × 3.0 × 1.6 cm adrenal gland with a 2.5 × 1.8 × 1.5 cm reddish brown pheochromocytoma located in the medulla, and a 4.4 × 2.3 × 1.3 cm yellow cortical adenoma. Both masses are confined to the adrenal gland
Discussion
Pheochromocytoma with synchronous cortical adenoma (PSCA) is a rare clinical entity characterized by simultaneous tumors in the adrenal medulla and cortex. This entity is seldom considered in the preoperative differential diagnosis of an adrenal mass. Among ten case reports in the literature, only 60% of the patients were diagnosed with PSCA preoperatively based on mixed biochemical and/or imaging findings [3,4,5,6,7,8,9,10,11,12]. Current guidelines from the American Association of Clinical Endocrinologist and American Association of Endocrine Surgeons published in 2009 recommend biochemical and imaging workup of all adrenal incidentalomas. Any patient found to have an incidental adrenal mass should undergo a full biochemical workup to exclude autonomous glucocorticoid production, catecholamine excess, and primary aldosteronism. Imaging is aimed at determining whether the neoplasm has features suggestive of malignancy. However, if there are mixed findings on clinical evaluation, biochemical analysis, or imaging, PSCA should be suspected and fully evaluated.
The most common clinical presentation of PSCA in our cohort involved characteristics related to pheochromocytoma (81%) including paroxysmal hypertension, palpitations, headaches, and generalized sweating. As expected with this surgical cohort, a diagnosis of pheochromocytoma was the presumptive preoperative diagnosis in the majority of patients. No patients presented with signs or symptoms that would have been suggestive of Cushing syndrome despite 25% of patients displaying autonomous glucocorticoid production on biochemical analysis. Five patients (31%) presented with medically recalcitrant hypertension and/or hypokalemia requiring potassium supplementation with 13% of patients ultimately diagnosed with primary aldosteronism. Although the hormonal activity of cortical adenomas in this study was higher (38%) than reported in previous studies on incidentalomas (7–10.8%), the hormonal activity in our cases was ascertained after pathological confirmation as opposed to evaluating for hormonal activity after finding an incidentaloma on imaging [13, 14]. Symptoms and signs of adrenal cortical hormone excess should be carefully elucidated during the initial workup of a suspected pheochromocytoma.
Even in the absence of clinical findings suggesting cortical hormone overproduction, full biochemical workup should ensue in patients with an adrenal incidentaloma. Initial biochemical evaluation for a hormonally active adrenal mass may include PAC/PRA ratio, plasma free metanephrines and normetanephrines, and overnight 1-mg dexamethasone suppression test. At our institution, we commonly include 24-h urine catecholamines, metanephrines, plasma free metanephrines, and 24-h urine cortisol levels. The 1-mg overnight dexamethasone suppression test can be used in patients suspected to have pheochromocytoma [15]. Another way to screen for surgically relevant subclinical cortisol excess in non-cushingoid adrenal adenoma patients is to obtain an ACTH level, which will be suppressed in cortisol overproduction. Any patient with significant hypertension may be worked up for primary aldosteronism with plasma aldosterone and plasma renin levels. Although none of our patients had suppressed plasma renin activity (PRA), the diagnosis of primary aldosteronism was made in 13% of our patients from both elevated plasma aldosterone concentrations (PAC) (above 15 ng/dL) and elevated PAC/PRA ratios (above 30 ng/dL). It should be noted that in patients with mixed biochemical and/or imaging findings, adrenal venous sampling should only be conducted after biochemical workup for pheochromocytoma has been excluded to avoid hypertensive crisis during the procedure, as was seen in both of our cases. Given that many of these cases (19%) had positive genetic testing for the presence of germline mutations associated with both types of adrenal tumors, this may have clued the clinician to suspect a broader presentation than a pure pheochromocytoma. Thus, the prevalence of PSCA in otherwise sporadic-appearing, uncomplicated pheochromocytoma patients may be less than what is reported here (4%). Regardless, any patients with mixed symptoms, biochemical, and/or imaging findings while pursuing workup for either a pheochromocytoma or adrenal adenoma should have a complete biochemical workup for PSCA.
In addition to full biochemical evaluation, imaging may suggest a synchronous adrenal neoplasm. A triple-phase dedicated adrenal CT scan can best detect subtleties within the adrenal gland. Non-dedicated CT scans done for other reasons can easily miss mixed features unless imaging and biochemical analysis clearly suggest pheochromocytoma in which case adrenalectomy will be performed regardless the results of dedicated adrenal CT (in this scenario, biochemical analysis will exclude Cushing’s or primary hyperaldosteronism). The dedicated adrenal CT will include thin cuts through the adrenal glands. Phases include non-contrast-enhanced images, venous phase images, and delayed phase images. Imaging should be reviewed to ascertain whether there are mixed features. Pheochromocytoma will typically be hyper-attenuating on non-contrast-enhanced images compared to cortical adenomas. Furthermore, pheochromocytoma will display with delayed washout of contrast. Diagnosis of PSCA can be difficult on imaging alone as the hypo-attenuating cortical adenoma can be in close association with the pheochromocytoma and be easily mistaken as heterogeneity of the pheochromocytoma. Characteristics of adrenal masses on non-contrast CT, specifically their radiodensity, can help guide clinicians toward a definitive diagnosis and assist in differentiating adrenal adenomas from non-adenomas [16]. Previously, researchers found that the mean pre-contrast HU value for adrenal adenomas and hyperplasia was 16.2 HU, compared to 38.6 HU for a pheochromocytoma [16]. Although these values are different, when these masses are in close proximity (as in the case of a PSCA) differentiation via CT may be more difficult. This may explain why only 50% of our cases were identified as having synchronous neoplasms on the initial scan. Conventional MRI can also distinguish between a pheochromocytoma and a cortical adenoma. This was the main modality used to detect PSCA in 44% of our patients when imaging characteristics on CT scan were mixed or indeterminate. Although 38% of our patients underwent nuclear imaging with 123-I-MIBG, this was mainly utilized to confirm whether the patient had a pheochromocytoma on an indeterminate scan after radiological diagnosis of adrenal adenoma.
Following a complete clinical, radiographic, and biochemical evaluation, patients with PSCA should undergo alpha-adrenergic blockade followed by beta-adrenergic blockade. Surgical resection may be recommended for appropriately selected surgical candidates due to significant cardiovascular complications from untreated catecholamine release from the pheochromocytoma in addition to the possibility of malignancy [17]. Previous studies detailing the optimal surgical approach for PSCA are lacking, but in our experience, this entity can be technically resected in a similar approach as other similarly sized adrenal masses. Multiple surgical approaches (open, laparoscopic transperitoneal, retroperitoneoscopic, robotic) have been described. Laparoscopic adrenalectomies can be performed via an anterior (transperitoneal) or posterior approach (retroperitoneal), both of which have equivalent operative duration, blood loss, time to ambulation and oral intake, and complication rates when performed by skilled surgeons [18]. Intraoperative challenges unique to PSCA include those similar to adrenalectomy for pheochromocytoma. Our approach to prevent hemodynamic lability was detailed in the Endocrine Society’s 2014 Clinical Practice Guidelines and includes preoperative pharmacologic preparation with combined alpha- and beta-adrenergic blockade, calcium channel blockers, and/or metyrosine [19].
Postoperative management of patients after resection of PSCA presents a few unique significant issues—particularly if the synchronous cortical adenoma was not expected and not fully biochemically evaluated preoperatively to exclude glucocorticoid autonomy. Following resection of pheochromocytoma, patients may become hypotensive secondary to either bleeding, lingering alpha-adrenergic blockade with vasoplegia, or a combination of both. In addition, if the synchronous cortical adenoma had some level of glucocorticoid autonomy, the hypothalamic–pituitary–adrenal axis may be suppressed resulting in secondary adrenal insufficiency. While no patients in our cohort who did not receive prophylactic steroid taper experienced this complication, this remains a relevant theoretical concern.
The natural history of a PSCA is poorly understood, but likely recapitulates that of their separate counterparts (pheochromocytoma and cortical adenoma). It is interesting to note that 18% of our cohort had a genetic predisposition to pheochromocytoma which is well within the range of what would be expected in patients with pheochromocytoma. However, only 5 of the 16 total patients underwent genetic testing and, therefore, the rate of a germline mutation may be much higher than our series suggests. Several genetic disorders that are associated with pheochromocytoma, including von Hippel–Lindau (VHL) syndrome, MEN2, and NF1, have not been reported to be associated with cortical adenomas. Rather, the pathophysiology underlying this co-occurrence may be related to hormonal signaling.
We do not know whether cortical adenomas developed in our patients because of a substance produced by the pheochromocytoma or vice versa. Catecholamine excess from pheochromocytoma can stimulate β − 1 adrenergic receptors in the juxtaglomerular apparatus to increase the release of renin into the circulation [20]. This has been shown to result in angiotensin release and subsequent adrenocortical stimulation, leading to cortical hyperplasia and the autonomous production of aldosterone [21]. Among the stimulating hormones that directly affect adrenocortical hormone release, only ACTH has been shown to be produced occasionally by pheochromocytomas [22]. Adrenocorticotropic hormone was not measured in our patients with PSCA, so we cannot say with certainty that this is the definitive mechanism which results in cortical growth. Previous studies have suggested that chromaffin cells within the adrenal medulla exert paracrine control on the adrenal cortex, resulting in stimulation of steroid synthesis [23]. In contrast, exogenous glucocorticoid has been shown to provoke pheochromocytoma crisis, possibly due to increased catecholamine secretion [24]. Taken together, these corticomedullary interactions may have contributed to the existence of PSCA in our patients. We have not encountered a case of a true mixed corticomedullary tumor at our institution and suspect that this entity is likely the misinterpretation of a collision event of two tumors from separate cortical and medullary backgrounds. Further research to elucidate the pathophysiology of this co-occurrence is warranted.
There are several limitations to our study. First, this was primarily a descriptive study without a control group for comparison. Additionally, all abstracted data from medical records were collected retrospectively and non-systematically as part of routine care, resulting in some aspects of diagnostic, therapeutic, and side effect outcomes that may have not been detected. Also, this was a single institutional experience with a limited sample size. Nonetheless, we report the largest experience with a rare clinical entity that has not been previously well described in the literature.
Conclusion
We describe the single largest series of PSCA, a rare but important clinical condition. In our cohort, nearly 4% of patients undergoing adrenalectomy for pheochromocytoma at our institution were found to have a synchronous cortical lesion. Of patients with PSCA, 25% had autonomous glucocorticoid overproduction and 13% had primary aldosteronism. Physicians should include PSCA in the differential diagnosis for any patient being evaluated for pheochromocytoma with mixed biochemical and/or imaging findings. In patients with mixed findings, it is imperative to rule out glucocorticoid excess, even if subclinical, as resection of a cortical adenoma that is autonomously producing glucocorticoids may result in postoperative adrenal insufficiency if not expected and treated appropriately. Conversely, patients being evaluated for primary aldosteronism in the setting of an identified adrenal neoplasm with mixed findings can be biochemically evaluated for catecholamine excess if clinical suspicion is high. Missing a biochemically functional pheochromocytoma, while unlikely, can potentially result in hypertensive crisis during AVS or laparoscopic adrenalectomy. Further multi-institutional studies are indicated to better define this unique clinical entity.
References
Herrera MF, Grant CS, van Heerden JA, Sheedy PF, Ilstrup DM (1991) Incidentally discovered adrenal tumors: an institutional perspective. Surgery 110(6):1014–1021
Young WF Jr (2007) Clinical practice. The incidentally discovered adrenal mass. N Engl J Med 356(6):601–610. doi:10.1056/NEJMcp065470
Bernini GP, Moretti A, Mannelli M, Ercolino T, Bardini M, Caramella D et al (2005) Unique association of non-functioning pheochromocytoma, ganglioneuroma, adrenal cortical adenoma, hepatic and vertebral hemangiomas in a patient with a new intronic variant in the VHL gene. J Endocrinol Invest 28(11):1032–1037
Cope O, Labbe JP, Raker JW, Bland EF (1952) Pheochromocytoma and adrenal cortical adenoma; report of a case with both tumors and discussion of their relation. J Clin Endocrinol Metab 12(7):875–880
Hwang WR, Ma WY, Tso AL, Pan CC, Chang YH, Lin HD (2007) Pheochromocytoma and adrenocortical adenoma in the same gland. J Chin Med Assoc JCMA 70(7):289–293
Inoue J, Oishi S, Naomi S, Umeda T, Sato T (1986) Pheochromocytoma associated with adrenocortical adenoma: case report and literature review. Endocrinol Jpn 33(1):67–74
Miyazawa K, Kigoshi T, Nakano S, Kobayashi Y, Suzuki K, Tsugawa R et al (1998) Hypertension due to coexisting pheochromocytoma and aldosterone-producing adrenal cortical adenoma. Am J Nephrol 18(6):547–550
Sakamoto N, Tojo K, Saito T, Fujimoto K, Isaka T, Tajima N et al (2009) Coexistence of aldosterone-producing adrenocortical adenoma and pheochromocytoma in an ipsilateral adrenal gland. Endocr J 56(2):213–219
Sato H, Igarashi H, Kishimoto Y, Yamaguchi K, Saito T, Ishida H et al (2002) Combined tumor consisting of non-functioning adrenocortical adenoma and pheochromocytoma in the same gland. Int J Urol 9(7):398–401
Sparagana M, Feldman JM, Molnar Z (1987) An unusual pheochromocytoma associated with an androgen secreting adrenocortical adenoma. Evaluation of its polypeptide hormone, catecholamine, and enzyme characteristics. Cancer 60(2):223–231
Yotsuyanagi S, Fuse H, Koshida K, Uchibayashi T, Namiki M (2001) A case of adrenal pheochromocytoma with contralateral adrenocortical adenoma. Hinyokika Kiyo 47(2):89–93
Aiba M, Hirayama A, Ito Y, Fujimoto Y, Nakagami Y, Demura H et al (1988) A compound adrenal medullary tumor (pheochromocytoma and ganglioneuroma) and a cortical adenoma in the ipsilateral adrenal gland. A case report with enzyme histochemical and immunohistochemical studies. Am J Surg Pathol 12(7):559–566
Mantero F, Terzolo M, Arnaldi G, Osella G, Masini AM, Ali A et al (2000) A survey on adrenal incidentaloma in Italy. Study Group on Adrenal Tumors of the Italian society of endocrinology. J Clin Endocrinol Metab 85(2):637–644. doi:10.1210/jcem.85.2.6372
Cawood TJ, Hunt PJ, O’Shea D, Cole D, Soule S (2009) Recommended evaluation of adrenal incidentalomas is costly, has high false-positive rates and confers a risk of fatal cancer that is similar to the risk of the adrenal lesion becoming malignant; time for a rethink? Eur J Endocrinol 161(4):513–527
Barrett C, van Uum SHM, Lenders JWM (2015) Risk of catecholaminergic crisis following glucocorticoid administration in patients with an adrenal mass: a literature review. Clin Endocrinol (Oxf) 83(5):622–628
Hamrahian AH, Ioachimescu AG, Remer EM, Motta-Ramirez G, Bogabathina H, Levin HS et al (2005) Clinical utility of noncontrast computed tomography attenuation value (hounsfield units) to differentiate adrenal adenomas/hyperplasias from nonadenomas: cleveland clinic experience. J Clin Endocrinol Metab 90(2):871–877. doi:10.1210/jc.2004-1627
Kassim TA, Clarke DD, Mai VQ, Clyde PW, Mohamed Shakir KM (2008) Catecholamine-induced cardiomyopathy. Endocr Pract 14(9):1137–1149. doi:10.4158/EP.14.9.1137
Constantinides VA, Christakis I, Touska P, Palazzo FF (2012) Systematic review and meta-analysis of retroperitoneoscopic versus laparoscopic adrenalectomy. Br J Surg 99(12):1639–1648
Lenders JWM, Duh Q-Y, Eisenhofer G, Gimenez-Roqueplo A-P, Grebe SKG, Murad MH et al (2014) Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 99(6):1915–1942
Reid IA, Schrier RW, Earley LE (1972) An effect of extrarenal beta adrenergic stimulation on the release of renin. J Clin Invest 51(7):1861–1869
Hsieh BS, Chen FW, Hsu HC, Chang CC, Chen WY (1979) Hyperaldosteronism with coexistence of adrenal cortical adenoma and pheochromocytoma. Taiwan Yi Xue Hui Za Zhi 78(5):445–451
Sakuma I, Higuchi S, Fujimoto M, Takiguchi T, Nakayama A, Tamura A et al (2016) Cushing syndrome due to ACTH-Secreting pheochromocytoma, aggravated by glucocorticoid-driven positive-feedback loop. J Clin Endocrinol Metab 101(3):841–846
Neri G, Andreis PG, Prayer-Galetti T, Rossi GP, Malendowicz LK, Nussdorfer GG (1996) Pituitary adenylate-cyclase activating peptide enhances aldosterone secretion of human adrenal gland: evidence for an indirect mechanism, probably involving the local release of catecholamines. J Clin Endocrinol Metab 81(1):169–173
Rosas AL, Kasperlik-Zaluska AA, Papierska L, Bass BL, Pacak K, Eisenhofer G (2008) Pheochromocytoma crisis induced by glucocorticoids: a report of four cases and review of the literature. Eur J Endocrinol 158(3):423–429
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hasassri, M.E., Pandian, T.K., Bobr, A.A. et al. Pheochromocytoma with Synchronous Ipsilateral Adrenal Cortical Adenoma. World J Surg 41, 3147–3153 (2017). https://doi.org/10.1007/s00268-017-4110-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4110-8