Abstract
Background
The recurrence patterns and therapeutic outcomes of patients with recurrent esophageal cancer after curative esophagectomy are not fully understood.
Methods
Data on recurrence patterns and sites of recurrence in patients with recurrent esophageal cancer after curative esophagectomy from 2005 to 2015 were retrospectively analyzed. Time to recurrence after curative esophagectomy and survival after recurrence were compared among groups stratified by recurrence pattern and site. Multivariate analysis was performed to identify clinicopathological parameters influencing survival after recurrence.
Results
Of the 290 patients identified, a single pattern of recurrence occurred in 224 patients (77.2%) and a multiple pattern of recurrence occurred in 66 patients (22.8%). The most frequent recurrence pattern was lymph node in 173 patients (59.7%), followed by distant organ in 133 patients (45.9%). Median time to recurrence and median survival after recurrence of all patients were 228 and 327 days, respectively. Among patients with lymph node or lung recurrence, there were 5-year survivors after recurrence who underwent multimodal therapy. Multivariate analysis revealed that longer disease-free interval [hazard ratio (HR) 0.70, 95% confidence interval (95% CI) 0.52–0.93], single pattern of recurrence (HR 0.54, 95% CI 0.39–0.74), and curative treatment for recurrence (HR 0.17, 95% CI 0.10–0.28) were significantly associated with favorable prognosis.
Conclusions
Although the prognosis of recurrent esophageal cancer remains unfavorable, if multimodal treatment that includes local therapy was curative, prognosis could improve, especially in patients with lymph node or lung recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal cancer is the sixth deadliest cancer worldwide [1]. Although esophagectomy remains the standard treatment for esophageal cancer, recurrence after curative esophagectomy is frequently observed [2, 3]. As lymph node metastasis occurs more frequently and extensively in esophageal cancer than in other gastrointestinal tract cancers, three-field lymphadenectomy, i.e., cervico-thoraco-abdominal lymph node dissection, has become the standard operative procedure in Japan [4, 5]. Meanwhile, two randomized phase III studies recently demonstrated a survival benefit associated with neoadjuvant treatment for esophageal cancer [6, 7]. However, even when esophagectomy with extended lymphadenectomy was performed after neoadjuvant treatment, the 5-year survival rate remained approximately 40% [6,7,8].
Several retrospective studies have revealed that lymph node recurrence is the most common pattern of recurrence after curative esophagectomy, followed by distant organ recurrence [3, 9, 10]. These studies have also demonstrated that distant organ recurrence had a poorer prognosis than loco-regional recurrence. However, details about recurrence patterns and sites, as well as the prognosis of patients with recurrent esophageal cancer, are not yet fully understood. Few studies have investigated the patterns and sites of recurrence after curative esophagectomy as well as the prognosis of patients in the era of neoadjuvant treatment. Therefore, the aim of this study was to clarify current recurrence patterns and therapeutic outcomes of patients with recurrent esophageal cancer after curative esophagectomy.
Materials and methods
Background and patient data
We reviewed data retrieved from a prospective database about esophagectomies performed by our department. A total of 1030 patients underwent esophagectomy for esophageal cancer between January 2005 and December 2015, of whom 971 patients underwent curative resection. Among them, disease recurrence occurred in 299 patients. Nine patients with no survival information were excluded, leaving 290 consecutive patients with recurrent esophageal cancer after curative esophagectomy. We investigated the recurrence patterns of esophageal cancer after curative esophagectomy and compared the time to recurrence after curative surgery and survival after recurrence between patients with different recurrence patterns and sites. In addition, we analyzed the associations between clinicopathological parameters and overall survival after recurrence. The original study protocol was approved by the institutional review board of our institution.
Recurrence patterns
Patients were divided into four groups by pattern of recurrence: lymph node, local, distant organ, and disseminated. Disseminated included both abdominal and pleural dissemination. In addition, a single pattern of recurrence was defined as simple recurrence and a combination of two or more patterns was defined as complex recurrence. Furthermore, recurrence in a distant organ was classified into five groups: bone, lung, liver, other, and multiple. “Other” represented recurrence in a distant organ other than bone, lung, or liver.
Treatment for recurrent disease
In general, patients diagnosed with a complex pattern of recurrence, disseminated, or multiple distant recurrences were treated with chemotherapy that included 5-fluorouracil, cisplatin, docetaxel, and paclitaxel. Patients with recurrence in a solitary lymph node or solid organ usually underwent chemoradiotherapy. We performed resection for recurrent esophageal cancer only when the recurrent tumor was solitary, localized, and considered to be completely resectable. Diagnostic resection was sometimes performed when a solitary lung or liver tumor was detected. After resection of the recurrent tumor, adjuvant chemotherapy or prophylactic radiotherapy was performed depending on the pathological findings.
Statistical analysis
Cumulative survival was estimated using the Kaplan-Meier method. The two groups were compared using a two-sided log-rank test. Multivariate Cox regression was performed. All variables with P < 0.1 in the univariate analyses were included in multivariable models. P < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 23 (IBM Corp., Armonk, NY).
Other materials and methods
Details of the other materials and methods are described in the Supplementary file.
Results
Recurrence patterns
Recurrence patterns and sites are summarized in Table 1. Among all 290 patients, the most common site of recurrence was lymph node in 173 patients (59.7%), followed by distant organ in 133 patients (45.9%), local recurrence in 29 patients (10.0%), and disseminated in 26 patients (9.0%). The pattern of recurrence was simple in 224 patients (77.2%) and complex in 66 patients (22.8%). With a simple recurrence pattern, the most common site was lymph node in 117 patients (52.2%), followed by distant organ in 79 (35.3%), local recurrence in 15 (6.7%), and dissemination in 13 (5.8%). Among patients who experienced simple lymph node recurrence, metastases limited to regional lymph nodes were observed in 78 patients while metastases to distant lymph nodes alone were seen in 33 patients, and metastases to both occurred in 6 patients. Distant organ recurrence involved the lung in 26 patients (11.6%), liver in 26 patients (11.6%), multiple organs in 12 patients (5.4%), bone in 6 patients (2.7%), and other organs in 9 patients (4.0%). Sites of recurrence classified as “other” included the brain (n = 2), skin (n = 2), kidney (n = 1), spleen (n = 1), adrenal gland (n = 1), bronchus (n = 1), and spinal cord (n = 1).
Relationship between patient characteristics or perioperative parameters and recurrent pattern
The clinicopathological characteristics of all 290 patients with recurrence are shown in Table 2. There were 249 men (85.9%) and 41 women (14.1%), with a median age of 64 years. The histological tumor type was squamous cell carcinoma in 243 patients (83.8%), adenocarcinoma in 32 patients (11.0%), and other in 15 patients (5.2%). Regarding preoperative treatment, chemotherapy was performed in 116 patients (40.0%) and chemoradiotherapy or radiotherapy was performed in 21 patients (7.2%); 153 patients (52.8%) did not undergo preoperative treatment. The pattern of recurrence did not differ largely by any patient background characteristic, including age, gender, American Association of Anesthesiologists physical status, histological diagnosis, preoperative treatment, type of esophagectomy, lymph node dissection type, cStage, and pStage.
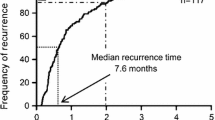
Time to recurrence after a curative esophagectomy
The median time to recurrence was 228 (15–2296) days after curative surgery. Recurrence was diagnosed within 1 year after esophagectomy in 199 patients (68.6%) and within 2 years in 256 patients (88.6%). Patients with a complex pattern of recurrence had a significantly shorter time to recurrence than those with a simple pattern (median time to recurrence, 190 vs. 255 days, P = 0.003). Among patients with a simple pattern of recurrence, patients with distant organ recurrence had the shortest interval to recurrence after a curative esophagectomy (median 179 days; range 15–2296 days), followed by lymph node recurrence (257 days; 34–1791 days), disseminated recurrence (334 days; 112–1071 days), and local recurrence (404 days; 151–1695 days). Furthermore, among patients with distant organ recurrence, patients with liver recurrence had the shortest time to recurrence (135 days; 64–2296 days), followed by multiple organ (141 days; 68–803 days), distant organ other than lung, liver, or bone (243 days; 93–1034 days), lung (314 days; 15–1745 days), and bone (453 days; 148–1533 days).
Treatment and overall survival after recurrence
The distribution of therapeutic modalities initially selected for primary recurrence after a curative esophagectomy was as follows: chemotherapy in 103 patients (35.5%), radiotherapy in 59 patients (20.3%), chemoradiotherapy in 41 patients (14.1%), surgical resection in 26 patients (9.0%), best supportive care in 52 patients (17.9%), and unknown in 9 patients (3.1%). As part of treatment for recurrence, 32 patients underwent surgical resection for a recurrent tumor. The median survival time after recurrence of all patients was 327 (1–3156) days. Patients with a complex pattern of recurrence had significantly poorer prognosis than patients with a simple pattern of recurrence (median survival after recurrence, 167 vs. 364 days, P < 0.001; Fig. 1a, d). Among patients with a simple pattern of recurrence, patients with disseminated recurrence had the shortest median survival (229 days; 5–393 days; Fig. 1b, d), followed by distant organ (327 days; 5–2925 days), local (410 days; 4–1518 days), and lymph node (478 days; 1–3156 days). Among patients with distant organ recurrence, patients with bone recurrence had the most unfavorable prognosis (48 days; 5–1117 days; Fig. 1c, d), followed by multiple organ (185 days; 7–459 days), liver (242 days; 39–893 days), lung (450 days; 89–2925 days), and distant organ other than the lung, liver, or bone (996 days; 212–1700 days). Among patients with lymph node or lung recurrence, there were patients who underwent multimodal therapy after recurrence who are 5-year survivors.
Overall survival after recurrence. a Overall survival after recurrence classified by simple or complex recurrence pattern; b overall survival after recurrence among patients with a simple recurrence stratified by site of recurrence; c overall survival after recurrence among patients stratified by distant organ of metastasis; d median time to recurrence after curative esophagectomy and median survival after recurrence among patients classified by recurrence pattern and site
Of the 290 patients, 46 patients underwent curative treatment, including 24 patients who underwent curative resection and 22 patients with complete response. Of 24 patients who achieved curative resection, the most frequent recurrent pattern was lymph node in 8 patients, followed by lung recurrence in 7 patients, other organ in 4 patients, liver recurrence in 3 patients, and local recurrence in 2 patients. Of 22 patients who achieved complete response, the most frequent pattern of recurrence was lymph node in 18 patients, followed by local recurrence in 2 patients, and lung and bronchus recurrence each in 1 patient. The therapeutic modalities selected were chemoradiotherapy, radiotherapy, and chemotherapy in 17, 4, and 1 patient, respectively.
Risk factors related to survival after recurrence
In the univariate analysis of survival after recurrence, longer time to recurrence after esophagectomy (≥228 days), simple recurrence pattern, and curative resection or complete response to a recurrent tumor were significantly associated with favorable prognosis, along with cStage and pStage (Table 3). Multivariate analysis revealed that longer time to recurrence after an esophagectomy [hazard ratio (HR) 0.67, 95% confidence interval (95% CI) 0.50–0.89, P = 0.006], simple recurrence pattern (HR 0.55, 95% CI 0.40–0.75, P < 0.001), and curative resection or complete response to recurrence (HR 0.16, 95% CI 0.09–0.27, P < 0.001) were independent prognostic factors for survival after recurrence.
Figure 2a demonstrates the effect of time to recurrence on survival after recurrence. When patients were divided into two groups by median survival of 228 days as the cutoff value, patients with a longer time to recurrence had significantly better survival than those with a shorter time to recurrence (median survival after recurrence, 250 vs. 389 days, P < 0.001). Figure 2b demonstrates the impact of curative resection or complete response to recurrent disease on survival after recurrence. Survival after recurrence was significantly better in patients who underwent curative resection or achieved complete response to recurrent disease than those who did not (median survival after recurrence, 250 vs. 1776 days, P < 0.001). The effect of curative resection or complete response to recurrence was observed in patients with lymph node recurrence as the first recurrence pattern (Fig. 2c; 5-year survival rate, 5.9 vs. 70.2%, P < 0.001) as well as in those with distant organ metastasis as the first recurrence pattern (Fig. 2d; median survival after recurrence, 277 vs. 1415 days, P < 0.001).
Overall survival after recurrence. a Overall survival after recurrence by time to recurrence after curative esophagectomy; b overall survival after recurrence by complete local control status; c overall survival of patients with lymph node metastasis; d overall survival of patients with distant organ metastasis. CR complete response
Among patients with curative resection or complete response, the median survival after recurrence was 2186 days in patients with lung recurrence (n = 8), 1415 days with other organ recurrence (n = 5), and 437 days with liver recurrence (n = 3). The 5-year survival rate after recurrence was 71.4 and 53.3% in patients with curative resection or complete response for mediastinal lymph node recurrence (n = 15) and cervical lymph node recurrence (n = 9), respectively.
Discussion
We analyzed data from 290 patients with recurrence after curative esophagectomy for esophageal cancer. We revealed that patients with a complex pattern of recurrence, disseminated, or distant organ recurrence had a relatively unfavorable prognosis. Within distant organ recurrence, bone, liver, or multiple metastases tended to be associated with poor prognosis. On the other hand, among patients with lymph node or lung recurrence, there were 5-year survivors after recurrence who underwent multimodal therapy. Multivariate analysis demonstrated that longer time to recurrence after esophagectomy, simple pattern of recurrence, and curative resection or complete response to recurrent tumors were significantly correlated with favorable prognosis.
Previous studies have demonstrated that about 80% of recurrences happen within 2 years of curative esophagectomy [10,11,12]. Lymph node, distant organ, and local recurrence were observed in 22–67, 31–55, and 3–8% of patients, respectively [3, 9, 10, 12,13,14,15]. In the present study, we also found that 88.6% of recurrences happen within 2 years of curative esophagectomy. The most common site of recurrence was lymph node (59.7%), followed by distant organ (45.9%), local (10.0%), and disseminated (9.0%). This result was consistent with previous reports. We also found that the distribution of recurrent sites was comparable between simple and complex recurrences. In addition, the recurrence pattern did not differ between patients who did or did not undergo preoperative treatment.
Another finding of this study was that patient prognosis differed according to metastatic organ, although recurrent esophageal cancer could be considered as systemic disease. In particular, some of patients with lymph node or lung recurrence could survive over 5 years after recurrence. We also showed that patients who had complex, liver, or bone recurrence had unfavorable prognosis, as in previous studies [10, 14, 16].
A previous study of 174 patients with esophageal adenocarcinoma after curative esophagectomy reported that survival after recurrence was significantly correlated with time to recurrence after curative surgery [11]. Miyata et al. [16] also showed that recurrence within 1 year of curative esophagectomy was significantly correlated with unfavorable prognosis after recurrence in patients with esophageal squamous cell carcinoma. In the present study, we also revealed that shorter time to recurrence after curative surgery was significantly correlated with unfavorable prognosis. This may be biologically plausible because high-grade cancers, which are more resistant to treatment, recur earlier and result in poorer survival. Duration to recurrence and site of metastasis could be surrogate markers of tumor biology.
Previous studies have suggested that multimodal treatment for recurrent esophageal tumors may prolong survival [10, 11, 14, 16, 17]. However, whether aggressive local treatment to control recurrent tumors improves survival or not remains unclear. Therefore, we evaluated the influence of local tumor control on survival after recurrence in this study. We demonstrated that complete surgical resection or complete response to treatment was an independent favorable prognostic factor. Although the therapeutic strategy for recurrent esophageal cancer has not yet been established, we showed that patients with lymph node or lung recurrence have the potential to be cured by local tumor control, which leads to a favorable prognosis.
Recently, several retrospective studies have demonstrated that resection of recurrent esophageal cancer, in particular lymph node or lung recurrence, prolongs prognosis [13, 17,18,19,20,21,22]. If a recurrent tumor is solitary or localized, resection could potentially be curative and may prolong survival. Although there was no consensus about the indications for surgical resection of a recurrent lymph node or pulmonary lesion, a longer disease-free interval from esophagectomy to recurrence was reported to be significantly associated with favorable prognosis after pulmonary resection [18, 22]. In the present study, we showed that both lymph node and lung recurrence was associated with a relatively long interval to recurrence after surgery, with long survival observed after such recurrences. These results indicate that lymph node or lung recurrence tends to grow slowly and locally, which might make them suitable for surgical treatment.
Several limitations of this study should be acknowledged. This was a retrospective study conducted in a single institution with a limited number of patients. In addition, during the present study period, surgical procedures, perioperative adjuvant therapies, and therapeutic strategies for recurrent esophageal cancer improved with each passing year. Therefore, the results of this study might not apply to all esophageal cancer patients who are going to receive treatment. A larger-scale, prospective study is necessary to validate the clinical significance of our findings.
In conclusion, this study revealed that longer time to recurrence, simple pattern of recurrence, and curative resection or complete response for disease recurrence could contribute to prolonged survival of patients with recurrent esophageal cancer. Although prognosis remains unfavorable, if multimodal treatment that includes local therapy was curative, prognosis could improve, especially in patients with lymph node or lung recurrence.
References
Zhang Y (2013) Epidemiology of esophageal cancer. World J Gastroenterol 19:5598–5606
Morita M, Kuwano H, Ohno S et al (1994) Characteristics and sequence of the recurrent patterns after curative esophagectomy for squamous cell carcinoma. Surgery 116:1–7
Doki Y, Ishikawa O, Takachi K et al (2005) Association of the primary tumor location with the site of tumor recurrence after curative resection of thoracic esophageal carcinoma. World J Surg 29:700–707. doi:10.1007/s00268-005-7596-4
Sannohe Y, Hiratsuka R, Doki K (1981) Lymph node metastases in cancer of the thoracic esophagus. Am J Surg 141:216–218
Fujita H (2015) History of lymphadenectomy for esophageal cancer and the future prospects for esophageal cancer surgery. Surg Today 45:140–149
Oppedijk V, van der Gaast A, van Lanschot JJ et al (2014) Patterns of recurrence after surgery alone versus preoperative chemoradiotherapy and surgery in the CROSS trials. J Clin Oncol 32:385–391
Ando N, Kato H, Igaki H et al (2012) A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol 19:68–74
Medical Research Council Oesophageal Cancer Working Group (2002) Surgical resection with or without preoperative chemotherapy in oesophageal cancer: a randomised controlled trial. Lancet 359:1727–1733
Natsugoe S, Okumura H, Matsumoto M et al (2006) The role of salvage surgery for recurrence of esophageal squamous cell cancer. Eur J Surg Oncol 32:544–547
Sugiyama M, Morita M, Yoshida R et al (2012) Patterns and time of recurrence after complete resection of esophageal cancer. Surg Today 42:752–758
Abate E, DeMeester SR, Zehetner J et al (2010) Recurrence after esophagectomy for adenocarcinoma: defining optimal follow-up intervals and testing. J Am Coll Surg 210:428–435
Lou F, Sima CS, Adusumilli PS et al (2013) Esophageal cancer recurrence patterns and implications for surveillance. J Thorac Oncol 8:1558–1562
Motoyama S, Kitamura M, Saito R et al (2006) Outcome and treatment strategy for mid- and lower-thoracic esophageal cancer recurring locally in the lymph nodes of the neck. World J Surg 30:191–198. doi:10.1007/s00268-005-0092-z
Kato H, Fukuchi M, Miyazaki T et al (2005) Classification of recurrent esophageal cancer after radical esophagectomy with two- or three-field lymphadenectomy. Anticancer Res 25:3461–3467
Ninomiya I, Okamoto K, Tsukada T et al (2016) Recurrence patterns and risk factors following thoracoscopic esophagectomy with radical lymph node dissection for thoracic esophageal squamous cell carcinoma. Mol Clin Oncol 4:278–284
Miyata H, Yamasaki M, Kurokawa Y et al (2011) Survival factors in patients with recurrence after curative resection of esophageal squamous cell carcinomas. Ann Surg Oncol 18:3353–3361
Hiyoshi Y, Morita M, Kawano H et al (2015) Clinical significance of surgical resection for the recurrence of esophageal cancer after radical esophagectomy. Ann Surg Oncol 22:240–246
Kanamori J, Aokage K, Hishida T et al (2016) The role of pulmonary resection in tumors metastatic from esophageal carcinoma. Jpn J Clin Oncol 47:25–31
Ichida H, Imamura H, Yoshimoto J et al (2013) Pattern of postoperative recurrence and hepatic and/or pulmonary resection for liver and/or lung metastases from esophageal carcinoma. World J Surg 37:398–407. doi:10.1007/s00268-012-1830-7
Yano M, Takachi K, Doki Y et al (2006) Prognosis of patients who develop cervical lymph node recurrence following curative resection for thoracic esophageal cancer. Dis Esophagus 19:73–77
Nakamura T, Ota M, Narumiya K et al (2008) Multimodal treatment for lymph node recurrence of esophageal carcinoma after curative resection. Ann Surg Oncol 15:2451–2457
Ichikawa H, Kosugi S, Nakagawa S et al (2011) Operative treatment for metachronous pulmonary metastasis from esophageal carcinoma. Surgery 149:164–170
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There are no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yamashita, K., Watanabe, M., Mine, S. et al. Patterns and Outcomes of Recurrent Esophageal Cancer After Curative Esophagectomy. World J Surg 41, 2337–2344 (2017). https://doi.org/10.1007/s00268-017-4024-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4024-5