Abstract
Background
Colectomy is one of the most common major abdominal procedures performed in the USA. A better understanding of risk factors and the effect of operative approach on adverse postoperative outcomes may significantly improve quality of care.
Methods
Adult patients with a primary diagnosis of colon cancer undergoing colectomy were selected from the National Surgical Quality Improvement Program 2013–2015 targeted colectomy database. Patients were stratified into five groups based on specific operative approach. Univariate and multivariate analyses were used to compare the five groups and identify risk factors for 30-day anastomotic leak, readmission, and mortality.
Results
In total, 25,097 patients were included in the study, with a 3.32% anastomotic leak rate, 1.20% mortality rate, and 9.57% readmission rate. After adjusting for other factors, open surgery and conversion to open significantly increased the odds for leak, mortality, and readmission compared to laparoscopy. Additionally, smoking and chemotherapy increased the risk for leak and readmission, while total resection was associated with increased mortality and leak.
Conclusions
Operative approach and several other potentially modifiable perioperative factors have a significant impact on risk for adverse postoperative outcomes following colectomy. To improve quality of care for these patients, efforts should be made to identify and minimize the influence of such risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colectomy is not only the mainstay of treatment for most colon cancers, but also constitutes an invaluable therapeutic option in the management of several non-neoplastic diseases, making it one of the most commonly performed abdominal operations in the USA. The last two decades have witnessed widespread adoption of minimally invasive techniques for many surgical procedures. Randomized trials have justified this trend, providing evidence for several benefits of minimally invasive surgery over the traditional open approach. Specifically, in patients undergoing colectomy, significant advantages in terms of shorter hospital length of stay (LOS), less pain, and earlier recovery of bowel function have been extensively reported [1, 2]. Nevertheless, laparoscopy remains underutilized for colectomy, showing a remarkably lower adoption rate over time than that observed for other procedures, such as cholecystectomy and Nissen fundoplication [3]. Furthermore, in recent years, newer techniques such as robotic surgery have entered the landscape of colorectal surgery, and there are data suggesting that this approach might deliver even additional benefits over conventional laparoscopy [4].
With the recent development of the targeted colectomy participant use file (PUF), the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database is a powerful tool to study current trends and outcomes surrounding colectomy. In addition to the robust preoperative data available for risk stratification, this database now uniquely contains details of the specific operative approach utilized as well as the ability to identify unplanned conversion from a minimally invasive to an open approach. This database provides adequate sample size to generate the statistical power to detect differences in less common complications between various operative approaches. Furthermore, a specific outcome measure for anastomotic leak was recently introduced, providing the opportunity to study this complication on a national scale using a standardized definition for the first time.
Therefore, the primary purpose of this study was to compare postoperative outcomes between various operative approaches for colectomy in patients with colon cancer. Secondarily, we aimed to identify other patient- and disease-related risk factors for mortality, anastomotic leak, and readmission following colon resection.
Materials and methods
Data source
This study is a retrospective analysis of the ACS-NSQIP-targeted colectomy database. Although this database was first introduced in 2011, detailed information regarding operative approach was not reported until 2013, and therefore this analysis was restricted to 2013–2015. The PUF contains 22 colectomy-specific variables collected from 154 participating sites [5]. Patients’ demographics, preoperative comorbidities, intraoperative variables, and 30-day postoperative morbidity and mortality outcomes were obtained by merging the aforementioned colectomy PUF with the main ACS-NSQIP database using the unique case identification variable.
Briefly, both the procedure-targeted and main ACS-NSQIP PUFs are validated databases that contain data regarding surgical patient comorbidities and 30-day outcomes. The data are abstracted from clinical records, rather than from administrative sources, by trained surgical clinical reviewers. Additional details of ACS-NSQIP are described elsewhere [6, 7]. This study was approved by the Institutional Review Board of the Johns Hopkins School of Medicine.
Study population
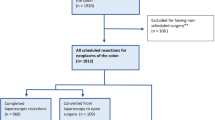
This study included patients with a primary diagnosis of colon cancer aged 18 years or older who underwent colectomy with or without proximal diverting ostomy (Current Procedural Terminology (CPT) codes of 44204, 44140, 44207, 44145, 44150, 44210, 44147, 44143, 44146, 44206, or 44208, 44205, or 44160) between January 1, 2013 and December 31, 2015. Patients undergoing emergency surgery were excluded. We restricted our cohort to colon cancer patients in order to achieve a more homogenous population. For the purpose of this study, five categories of operative approach were defined for comparison as detailed in Table 1. Patients who underwent single-incision laparoscopic surgery (SILS) and other less commonly performed procedures were excluded. Further exclusion criteria included diagnosis of disseminated cancer.
An additional small proportion of patients were excluded specifically from the readmission analysis alone. Readmission is defined by NSQIP as at least one readmission (to the same or other hospital), for any reason, within 30 days of surgery. Therefore, patients who remain in the hospital longer during their initial hospitalization have fewer days of follow-up time, introducing an immortal time bias. To address this concern, patients with LOS greater than 16 days (2.92% of the overall population) were excluded in order to allow a minimum of 2-week post-discharge follow-up. Additionally, patients not at risk of readmission due to predischarge in-hospital mortality and discharge to a separate acute care hospital were excluded from the readmission analysis as well.
Demographic and clinical characteristics
Demographic and clinical characteristics considered to be potentially associated with anastomotic leak, mortality, and hospital readmission were assessed. Demographic characteristics included age, gender, and race. Clinical characteristics included American Society of Anesthesiologists (ASA) classification of physical condition, functional status, body mass index (BMI), and preoperative comorbidities. Current smoking is defined as smoking within 1 year before surgery; weight loss is defined as >10% weight loss within 6 months prior to surgery; chemotherapy identifies patients receiving treatment within 90 days prior to surgery. Age and BMI were categorized as follows: <50, 50–59, 60–69, 70–79 and ≥80 years old, and <18.5 kg/m2 (underweight), 18.5–24.9 kg/m2 (normal), 25–29.9 kg/m2 (overweight), and ≥30 (obese), respectively. Other variables included in analysis were type of resection (partial vs. total), and proximal diversion.
Outcomes
Intraoperative and postoperative outcomes were compared between the five operative approaches. The three primary outcomes were anastomotic leak, mortality, and hospital readmission within 30-days of surgery. Secondary outcomes included LOS (days from operation to discharge), operative time, non-home discharge destination (transfer to rehabilitation facility, separate acute care, or skilled care), prolonged postoperative ileus, and individual complications reported in the NSQIP database. Additional secondary composite endpoints were based on groupings of similar complications. These included wound complications (any of superficial surgical site infection (SSI), deep incisional SSI, or wound dehiscence); cardiac complications (cardiac arrest requiring cardiopulmonary resuscitation and myocardial infarction); renal complications (postoperative acute renal failure or progressive renal insufficiency); and thrombotic complications (deep vein thrombosis/thrombophlebitis and pulmonary embolism). Serious morbidity was defined as occurrence of one of the following complications: cardiac complication, sepsis/shock, unplanned intubation, on ventilator for more than 48 h, organ space SSI, or reoperation.
Statistical analysis
Baseline patient demographics and comorbidities were compared using Pearson’s Chi-square tests for categorical variables and analysis of variance (ANOVA) for continuous variables. Initial exploratory data analyses were performed using univariate logistic regression to compare the odds of anastomotic leak, mortality, and readmission across the five operative approach groups. Odds ratios (OR) and 95% confidence intervals (CI) are reported. Multivariable logistic regression analyses were then performed to compare outcomes between operative approaches while controlling for baseline differences between the groups. Initially, each multivariable model included all covariates with associations in the exploratory analysis at the p < 0.25 significance level, as recommended by Hosmer and Lemeshow [8]. These models were then refined based on the clinical importance of covariates and their impact on the overall model, as determined by likelihood ratio tests. The final models were evaluated using the Hosmer–Lemeshow goodness-of-fit test [8]. Statistical significance was defined as p < 0.05 for all statistical tests. All statistical analysis was conducted using Stata/MP version 14 (StataCorp LP, College Station, TX, USA).
Results
Study population
A total of 25,097 patients underwent partial or total colectomy and met inclusion criteria for the study. The mean [SD] age and BMI of the overall study population were 66.2 [13.5] years and 28.5 [6.6], respectively. Laparoscopy, open, and hand assisted procedures were the most common (30.51, 26.74, and 30.51%, respectively). Significant differences between the five operative approaches were observed with regards to patient demographics and clinical characteristics. Not surprisingly, older patients with higher ASA classification and multiple comorbidities more frequently underwent an open procedure (Table 2). Open surgery was the most commonly utilized operative approach for total colectomy (43.79% of total resections). Patients requiring conversion to open were more likely to be obese (43.06%) compared to those completed via the planned minimally invasive approach.
Outcomes
Unadjusted analysis
The overall rates for anastomotic leak, mortality, and readmission were 3.32% (n = 834), 1.20% (n = 300), and 9.57% (n = 2286), respectively. Anastomotic leak and readmission rates were highest in the open and conversion to open groups (4.37 and 4.49, 12.11 and 12.14%, respectively) and lowest in the lap group (2.30, 7.57%, respectively) (Table 3). Mortality rate was highest in the open group (2.21%) and lowest in the robotic group (0.19%). Aside from operative approach, factors associated with increased risk of anastomotic leak included, male gender, chemotherapy and smoking (Table 4). Higher mortality was associated with older age and multiple comorbidities and factors associated with readmission included proximal diversion, age ≥80, ASA class, chemotherapy and renal disease.
Adjusted analysis
Even when controlling for underlying differences between the five groups, patients undergoing open, conversion to open, and hand assisted procedures had worse outcomes compared to laparoscopy (Table 5). Specifically, patients who underwent an open or conversion to open procedures were nearly twice as likely to suffer from anastomotic leak, and over twice more likely to die. Open and conversion to open procedures also had about 1.5-fold increase in readmission. In addition, although the hand-assisted approach had increased odds of leak (OR 1.30, 95% CI 1.06–1.59, p = 0.010) and readmission (OR 1.17, 95% CI 1.03–1.31, p = 0.012), those odds were substantially lower than the odds of leak in the open (OR 1.72, 95% CI 1.42–2.10, p < 0.001) and conversion to open (OR 1.81, 95% CI 1.39–2.36, p < 0.001) approaches and readmission in the open (OR 1.44, 95% CI 1.28–1.62, p < 0.001) and conversion to open (OR 1.52, 95% CI 1.28–1.80, p < 0.001) approaches. Smoking carried increased odds of both anastomotic leak (OR 1.37; 95% CI 1.13–1.64, p < 0.001) and readmission (OR 1.19, 95% CI 1.04–1.36, p = 0.009). Additional independent predictors of both mortality and readmission included ASA class, partially/totally dependent status, and history of CHF, while chemotherapy was associated with both anastomotic leak and readmission. Finally, proximal diversion was associated with significantly increased odds of readmission (OR 1.51, 95% CI 1.29–1.78, p < 0.001).
Discussion
In this study, we have identified several factors, including both patient characteristics and chosen operative approach that increase the risk for anastomotic leak, mortality, and readmission after colon resection.
Anastomotic leak is one of the most feared complications of colectomy, having a direct influence on other important outcome measures such as need for reoperation and mortality [9]. Prior to the development of the NSQIP-targeted colectomy PUF, the ability to reliably measure the risk of anastomotic leak using large multi-institutional datasets has been limited. The absence of a standardized outcome variable has previously required investigators to rely on surrogate measures such as “organ space SSI,” which grossly underestimates true leak rates [10]. In the present study, we were able to identify several risk factors for anastomotic leak. We found that sicker patients, with higher ASA classification, had higher risk for leak.
Other independent predictors for anastomotic leak identified in this study included male gender and smoking. Higher risk of leak in male patients has been reported previously and is generally attributed to increased difficulty operating in the narrower male pelvis [11]. Smoking has also been identified as an important risk factor for leak in prior studies. Sørensen et al. proposed an underlying etiology of anastomotic malperfusion secondary to nicotine-induced vasoconstriction and microthromboses due to increased platelet aggregation [12]. The influence of smoking behavior on anastomotic integrity is a factor worth stressing, as it not only increases the risk of leak, but also represents one of the few truly modifiable variables.
Both open surgery and conversion to open were associated with significantly worse outcomes by all measures. The effect of conversion on postoperative outcomes is likely related in part to the reason for conversion itself. For example, factors such as unusual anatomy, occurrence of unexpected intraoperative complications, or staging errors may both dictate the decision to convert and also lead to a suboptimal postoperative course, thereby confounding the relationship between conversion and outcomes. This represents a controversial topic in the literature, with some authors reporting higher morbidity and mortality in converted patients, while others describe outcomes comparable to laparoscopy [13–15]. The NSQIP-targeted colectomy database makes a particularly meaningful contribution to the literature on this topic, benefiting from a very large, high-quality sample and detailed information regarding operative approach.
Patients undergoing open colectomy were older and had more comorbid conditions at baseline compared to those undergoing minimally invasive approaches, and it is therefore unsurprising that unadjusted analysis revealed worse outcomes in this group. Nonetheless, these differences remained significant in the adjusted analysis, suggesting that there are true benefits to minimally invasive colon resection. These findings are in contrast to two highly cited previous randomized, multi-center studies comparing laparoscopic versus open surgery for colon cancer. In both the COST [16] and COLOR [17] trials, overall complications, readmissions, and mortality were equivalent in both the open and laparoscopic group. However, in both studies, approximately 20% of patients with either an open or a converted to open approach were analyzed in the laparoscopic group given the intention to treat analysis. A recent analysis of the Nationwide Inpatient Sample (NIS) database described higher mortality and complication rates for patients undergoing open colectomy, even after applying propensity matching [18]. Furthermore, open colectomy is economically disadvantageous, leading to significantly higher healthcare costs and utilization in the short- and long-term [19]. In light of this evidence, one must wonder why minimally invasive colon resection has not achieved the same reach as other abdominal operations, such as laparoscopic cholecystectomy. Although some possible reasons for the empiric selection of an open approach, such as prior history of complex abdominal surgery or intraabdominal infection, are not traceable through NSQIP, such explanations likely do not fully account for why over one-third of patients continue to undergo open surgery. Barriers to wider adoption must be identified and addressed in order to deliver the highest quality of care to all patients.
Robotic approach did not differ significantly from laparoscopic colectomy in terms of mortality, readmission rates, and risk of anastomotic leak. Hand-assisted techniques, which accounted for nearly 30% of all cases, may serve as an important bridge to a totally minimally invasive approach and, importantly, appear to offer some of the benefits granted by pure minimally invasive techniques. Cima and colleagues [20] found hand-assisted colectomy to have comparable 30-day outcomes to laparoscopy. These findings were associated with the added benefit of shortened operative times, resulting in meaningful economical savings. Unfortunately, they did not investigate the effect of the hand-assisted approach on anastomotic leak or readmission, nor have any other published studies to date. As robotic surgery is also significantly more costly than laparoscopy [18], the equivalence in outcomes becomes an important factor in assessing value. While features of the surgical robot (magnified tridimensional visualization, excellent range of motion, tremor filtration) have the theoretical potential to improve outcomes over other techniques, this potential has gone largely unrealized in practice [4, 21].
The last main outcome we evaluated was readmission, which represents an increasingly important quality indicator for surgery and has been estimated to cost about $300 million annually for colorectal surgery alone in the USA [22]. Several of the risk factors we identified for readmission, such as proximal diversion and open surgery, have been previously reported [23, 24] and are to some extent at the discretion of the operating surgeon. Most of the independent predictors of readmission, however, such as renal disease, recent chemotherapy and history of CHF, are poorly modifiable patient characteristics. This is an important finding in the era of pay-for-performance and financial penalties tied to hospital readmission.
While the novel NSQIP-targeted colectomy database has many strengths which have been leveraged for this study, there are also inherent limitations. For example, we were unable to assess functional and oncologic outcomes, both of which are clearly important when comparing surgical techniques. In addition, NSQIP is limited to 30-day outcomes and therefore fails to detect deaths and readmissions occurring after that time period. While we made every attempt to control for differences between groups, there are certainly remaining unmeasured differences, such as previous surgical history and patient preferences, which may play an important role when comparing operative techniques. Specifically, our analysis assumes that all patients were candidates for any of the potential operative approaches, which is almost certainly untrue. Ideally, we would have been able to exclude patients who underwent an open procedure because it was the only available option. Given this inherent limitation of a retrospective database study, we undertook a comprehensive multivariate analysis to adjust for confounding baseline differences between the five groups. Finally, hospital participation in NSQIP is voluntary and self-funded, so it is unknown whether the data reported by this small subset of hospitals, usually high volume centers, can accurately be extrapolated to all hospitals. Despite these limitations, we believe that the use of a surgically oriented database and the large sample size in this study have allowed us to evaluate the comparative effectiveness of various operative approaches to colectomy.
We found that minimally invasive techniques are associated with improved short-term outcomes following colectomy. While there is clearly significant selection bias in terms of operative approach, our adjusted analysis suggests that there are likely real differences in outcomes between patients undergoing minimally invasive and open procedures. We have also identified several potentially modifiable perioperative factors that are associated with increased risk of anastomotic leak, mortality, and readmission. These results are important for risk stratification, patient counseling, and quality improvement efforts in this patient population.
References
Veldkamp R, Kuhry E, Hop WC et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484
Lacy AM, Garcia-Valdecasas JC, Delgado S et al (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359(9325):2224–2229
Robinson CN, Chen GJ, Balentine CJ et al (2011) Minimally invasive surgery is underutilized for colon cancer. Ann Surg Oncol 18(5):1412–1418
Chang YS, Wang JX, Chang DW (2015) A meta-analysis of robotic versus laparoscopic colectomy. J Surg Res 195(2):465–474
ACS-NSQIP. ACS-NSQIP participant use data file [Internet]. Available from: https://www.facs.org/quality-programs/acs-nsqip/program-specifics/participant-use. Accessed 8 Dec 2015
Henderson WG, Daley J (2009) Design and statistical methodology of the national surgical quality improvement program: Why is it what it is? Am J Surg 198(5 Suppl):S19–S27
American College of Surgeons. ACS-NSQIP data collection, analysis, and reporting [Internet]. Available from: http://site.acsnsqip.org/program-specifics/data-collection-analysis-and-reporting/. Accessed 8 Dec 2015
Hosmer DW, Lemeshow S (2000) Applied logistic regression, 2nd edn. Wiley, New York
Bakker IS, Grossmann I, Henneman D, Havenga K, Wiggers T (2014) Risk factors for anastomotic leakage and leak-related mortality after colonic cancer surgery in a nationwide audit. Br J Surg 101(4):424–432 discussion 32
Rickles AS, Iannuzzi JC, Kelly KN et al (2013) Anastomotic leak or organ space surgical site infection: What are we missing in our quality improvement programs? Surgery 154(4):680–687 discussion 7–9
Krarup PM, Jorgensen LN, Andreasen AH, Harling H (2012) A nationwide study on anastomotic leakage after colonic cancer surgery. Colorectal Dis 14(10):e661–e667
Sorensen LT, Jorgensen T, Kirkeby LT, Skovdal J, Vennits B, Wille-Jorgensen P (1999) Smoking and alcohol abuse are major risk factors for anastomotic leakage in colorectal surgery. Br J Surg 86(7):927–931
Scheidbach H, Garlipp B, Oberlander H, Adolf D, Kockerling F, Lippert H (2011) Conversion in laparoscopic colorectal cancer surgery: impact on short- and long-term outcome. J Laparoendosc Adv Surg Tech A 21(10):923–927
Franko J, Fassler SA, Rezvani M et al (2008) Conversion of laparoscopic colon resection does not affect survival in colon cancer. Surg Endosc 22(12):2631–2634
Allaix ME, Degiuli M, Arezzo A, Arolfo S, Morino M (2013) Does conversion affect short-term and oncologic outcomes after laparoscopy for colorectal cancer? Surg Endosc 27(12):4596–4607
The Clinical Outcomes of Surgical Therapy (COST) Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
The COlon cancer Laparoscopic or Open Resection Study Group (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomized trial. Lancet Oncol 6:477–484
Juo YY, Hyder O, Haider AH, Camp M, Lidor A, Ahuja N (2014) Is minimally invasive colon resection better than traditional approaches?: First comprehensive national examination with propensity score matching. Jama Surg 149(2):177–184
Crawshaw BP, Chien HL, Augestad KM, Delaney CP (2015) Effect of laparoscopic surgery on health care utilization and costs in patients who undergo colectomy. Jama Surg 150(5):410–415
Cima RR, Pendlimari R, Holubar SD et al (2011) Utility and short-term outcomes of hand-assisted laparoscopic colorectal surgery: a single-institution experience in 1103 patients. Dis Colon Rectum 54(9):1076–1081
Davis BR, Yoo AC, Moore M, Gunnarsson C (2014) Robotic-assisted versus laparoscopic colectomy: cost and clinical outcomes. Jsls. 18(2):211–224
Wick EC, Shore AD, Hirose K et al (2011) Readmission rates and cost following colorectal surgery. Dis Colon Rectum 54(12):1475–1479
Kulaylat AN, Dillon PW, Hollenbeak CS, Stewart DB (2015) Determinants of 30-d readmission after colectomy. J Surg Res 193(2):528–535
Damle RN, Cherng NB, Flahive JM et al (2014) Clinical and financial impact of hospital readmissions after colorectal resection: predictors, outcomes, and costs. Dis Colon Rectum 57(12):1421–1429
Acknowledgements
This study was supported by the Johns Hopkins University Department of Surgery Research Fund from Mr. Edwin Lewis.
Author contribution
All authors contributed substantially to the design, analysis, and writing and/or revising of this manuscript. All authors provided final approval of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Mungo, B., Papageorge, C.M., Stem, M. et al. The Impact of Operative Approach on Postoperative Complications Following Colectomy for Colon Caner. World J Surg 41, 2143–2152 (2017). https://doi.org/10.1007/s00268-017-4001-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4001-z