Abstract
Background
There is a paucity of literature comparing laparoscopic to robotic inguinal hernia repair. We present a single surgeon’s transition from laparoscopic totally extraperitoneal (L-TEP) to robotic transabdominal preperitoneal (R-TAPP) inguinal hernia repair and compare outcomes from the two approaches.
Methods
This retrospective review and analysis of prospectively collected data compare outcomes during the transition from L-TEP to R-TAPP inguinal hernia repair by a single surgeon at one institution. Operating times and surgical outcomes and complications are analyzed. All consecutive L-TEP cases from November 2012 to August 2014 and all consecutive R-TAPP cases from March 2013 to October 2015 were included in the analysis.
Results
A total of 157 and 118 patients underwent L-TEP and R-TAPP inguinal hernia repair, respectively. The groups were similar regarding demographics and ASA class. A significantly higher number of complex cases were performed in the R-TAPP group compared to L-TEP group (n = 11 vs. n = 1, p = 0.0001). Mean surgical times were nearly identical (69.12 ± 35.13 min, R-TAPP; 69.05 ± 26.31, L-TEP) as were intraoperative and postoperative complication rates—despite the significantly higher number of complex cases in the R-TAPP group.
Conclusions
This is the largest study in the literature comparing a single surgeon’s experience transitioning from L-TEP to R-TAPP inguinal hernia repair. Results from the R-TAPP cases were similar to those achieved from laparoscopic cases. The robotic platform may have facilitated the execution of complex hernia cases during the proficiency phase.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia repair is one of the most common surgeries in the USA, with roughly 750,000 performed annually [1]. There has been a gradual evolution of inguinal hernia repair since the advent of laparoscopy in the mid-1990s. Unlike cholecystectomy, which is preferentially performed laparoscopically, inguinal hernia repair continues to be performed largely by the open approach. The first randomized prospective trial revealed recurrence rates of 10% after laparoscopic inguinal herniorrhaphy; this recurrence rate was significantly higher than that reported for open mesh repair [2]. However, the recurrence rates after procedures performed by the more experienced surgeons were similar to those after an open or laparoscopic repair [3].
Laparoscopic inguinal hernia repair, whether by the transabdominal preperitoneal (TAPP) or totally extraperitoneal (TEP) approaches, is associated with comparable recurrence rates and similar morbidity and mortality [1]. Many surgeons in the USA, however, prefer and continue to perform open inguinal hernia repairs, even for bilateral and recurrent inguinal hernia [4]. The long learning curve associated with the laparoscopic approach may be the reason for this preference. Developing proficiency with laparoscopic repair of inguinal hernias ranges from 100 to 240 operations [5–7].
Robotic surgery with the da Vinci® (Intuitive Surgical, Inc., Sunnyvale, CA) system offers three-dimensional vision through a computer interface, a stable platform, and increased dexterity with seven degrees of freedom at the articulating wrist. A study performed during the infancy of robotic surgery revealed that surgeons were significantly faster suturing and knot tying than they were at standard laparoscopy [8]. A later study revealed that novices in robotic surgery demonstrated consistently faster suturing using the robotic platform versus standard laparoscopy [9]. Similar to laparoscopic surgery, there is a learning curve to develop proficiency in the use of the robotic system [8, 10–12]. Use of the robot for repair of inguinal hernias has thus far provided promising outcomes, although the data are limited due to the novelty of the robotic approach for hernia repair [13].
We present a large retrospective case series that demonstrates a single surgeon’s learning curve transitioning from laparoscopic TEP inguinal hernia repair to TAPP inguinal hernia repair utilizing the da Vinci Si® Surgical System.
Materials and methods
Patient selection
The Good Samaritan Medical Center Institutional Review Board approved this retrospective review and analysis of prospectively collected data comparing L-TEP to R-TAPP inguinal hernia repair by a single surgeon (O.Y.K). The data in each group were collected over two time periods with some overlap, as the surgeon transitioned from laparoscopic surgery to robotic-assisted surgery. Data for the L-TEP group were collected from November 2012 to August 2014. Data from the R-TAPP group were collected from March 2013 to October 2015. All patients who underwent laparoscopic and robotic inguinal hernia repair by the surgeon over this time period were included.
Operative technique
We asked all patients to empty their bladders immediately before each operation (R-TAPP and L-TEP) and encouraged the anesthesiologist to restrict perioperative fluid to minimize postoperative urinary retention.
Robotic transabdominal preperitoneal inguinal hernia repair
The instrument table was set up in the same fashion for every case to provide workflow efficiency. Pneumoperitoneum was achieved via Veress needle placement in the left upper quadrant (Palmer’s). Three 8.5-mm trocars were introduced in a horizontal line 4 cm above the umbilicus; each lateral trocar was positioned in the mid-clavicular line, and the center trocar positioned just off the midline. All trocars were separated by at least 8 cm. The patient was then placed in the Trendelenburg position, and the robot was docked at the patient’s side at 30 degrees. All procedures were performed with a robotic bipolar grasper, needle driver, and monopolar scissors. The first assistant placed the laparoscopic needle driver and grasper through one of the 8.5-mm trocars to introduce the mesh and selected sutures. In cases involving intestinal adhesions, we avoided extensive adhesiolysis unless the adhesions obstructed the view. To avoid visceral injury in cases of sliding or irreducible hernias, neither adhesiolysis nor reduction was performed at the beginning of the case; rather, these procedural steps were taken during preperitoneal dissection and mobilization of the hernia content.
A peritoneal incision was made 4 cm above the inguinal canal from the anterior superior iliac spine to the median umbilical ligament, and the flap was developed with dissection in the preperitoneal space. The medial extent of dissection was carried out roughly 2 cm beyond the symphysis pubis to the contralateral side. The cranial extent of the dissection was carried out 4 cm above the transversalis arch. The lateral extent was the anterior superior iliac spine. The caudal extent was 4 cm below the iliopubic tract at the level of the psoas muscle and 2 cm below Cooper’s ligament. The peritoneal hernia sac and associated adipose tissue from the hernia (pre-, extra-, and retroperitoneal fat) were reduced toward the middle of the psoas muscle (parietalization), taking into consideration the importance of preserving the spermatic fascia and lumbar fascia to protect the vas deferens, nerves, and vessels.
Complete dissection of the pelvic floor ensured flat placement of the mesh, which covered the entire myopectineal orifice without folding. An assistant then introduced the ProGrip™ Laparoscopic Self-Fixating Mesh, Anatomical Design (Covidien, New Haven, CT USA) through one of the 8.5-mm trocar sites. Depending on the size of the hernia, we used either the 10 × 15 cm mesh or the 12 × 16 cm mesh. The mesh was placed in the peritoneal flap without using tacks or sutures. After adequate positioning of the mesh was ensured, the peritoneal flap was closed using a 3–0 absorbable, barbed suture. Local anesthetic (1% bupivacaine hydrochloride; Marcaine) was infiltrated at the trocar sites prior to skin closure.
We generally utilized three robotic instruments: bipolar non-crushing grasper, monopolar scissors, and needle driver.
Laparoscopic totally extraperitoneal inguinal hernia repair
A fascial incision was made into the anterior rectus sheath, and the rectus muscle was retracted laterally to gain entry to the preperitoneal space. A 12-mm blunt-tip trocar was then placed with an oval dissection balloon to help delineate the anatomy of the inguinal space and dissect within the preperitoneal space. Two 5-mm trocars were then placed in the same vertical line, taking care to prevent peritoneal entry. We ensured that dissection extended superiorly to the level of the umbilical area, inferiorly to the space of Retzius, inferolaterally to the psoas muscle and the space of Bogros until the anterior superior iliac spine was reached, and medially at least 2 cm beyond the midline.
In a similar fashion to the R-TAPP repair, complete exposure of the myopectineal orifice of Fruchaud was achieved, as it is considered critical to any minimally invasive inguinal hernia repair [1]. The hernia and any associated adipose tissue were reduced to the level of psoas muscle; complete parietalization of the vas deferens and the testicular vessels was achieved; and complete dissection of the pelvic floor was carried out to ensure flat placement of the mesh without folding or curling.
In challenging cases, such as large indirect or scrotal hernias, we identified the spermatic vessels first and began the dissection along the vessels toward the inguinal canal and to the top of the indirect sac to reduce risk of injury to the spermatic vessels. We often excised preperitoneal fat after retraction, because the fat may mimic a recurrent hernia in the future or become symptomatic. ProGrip™ Laparoscopic Self-Fixating Mesh, Anatomical Design (Covidien, New Haven, CT) was placed, using either the 10 × 15 cm mesh or the 12 × 16 cm mesh. No tacks were used to secure the mesh. The 12-mm balloon trocar incision was closed with a figure of eight zero absorbable braided suture. Skin closure was performed only at the 5-mm ports. Local anesthetic (1% bupivacaine hydrochloride; Marcaine) was infiltrated at the trocar sites. In cases of peritoneal entry, we attempted to close the peritoneum with a 5-mm metallic clip, and in cases where we failed to do so, we placed a left upper quadrant 5-mm port to decompress the peritoneal cavity, thus facilitating the completion of the L-TEP repair.
In the L-TEP group, we used 5-mm laparoscopic instruments and a 10-mm angled scope. Disposables in the L-TEP group were the 12-mm balloon dissector port, two 5-mm disposable ports, and occasionally a laparoscopic 5-mm clip applier to close peritoneum in cases involving peritoneal entry. We did not use a vessel sealer or ultrasonic dissectors. A laparoscopic suction irrigator was used only if needed. We used tacks during the first 16 cases of L-TEP; no tacks were used for the R-TAPP procedures.
Outcome measures and statistical analysis
Patient demographics were collected as were data on any prior open or laparoscopic inguinal hernia repairs on the operative side. Bilateral and unilateral surgical skin-to-skin (first incision to last closure) times were analyzed (Satterthwaite T test) and, for the robot, included docking and undocking of the console [14]. The surgeon’s routine patient follow-up for hernia surgery occurred in office at 2 weeks, 3 months, 1 and 3 years. Performance of complex cases (the presence of an incarcerated non-reducible or scrotal hernia), conversion to laparotomy, and postoperative complications through 3 months were also analyzed (Fisher’s exact test). Characteristics of the inguinal hernias in the R-TAPP versus L-TEP group, including bilateral versus unilateral repair, were compared (Chi-square), as were emergent cases in each group (Fisher’s exact test). Postoperative complications through 3 months, i.e., re-admission, urinary retention, symptomatic seroma requiring intervention, and inguinodynia, were also compared (Fisher’s exact test). Recurrence and inguinodynia were analyzed at the 1-year follow-up (Fisher’s exact test). Statistical significance was set at a p < 0.05. Analyses were performed with SAS v9.4 (SAS Institute Inc., Cary, NC, USA).
Results
One hundred eighteen patients underwent R-TAPP inguinal hernia repair, and 157 patients underwent L-TEP inguinal hernia repair at a single institution from March 2013 through December 2015. One surgeon (O.Y.K.) performed all cases. One patient was lost to follow-up at 3 months in the R-TAPP group, and 16 R-TAPP patients had not yet completed their 1-year postoperative visit at the time of this writing. Patient characteristics at baseline were significantly different between the two cohorts, with the exception of their ASA classifications (Table 1). The robotic group was characterized by significantly older patients with significantly higher body mass indices and significantly higher proportion of females. The percentage of patients undergoing recurrent hernia repair was lower in the robotic group than in the laparoscopic group, although the difference was not statistically significant.
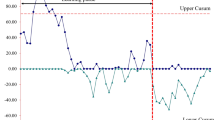
Almost all cases were elective, with 3 and 1 cases performed emergently for R-TAPP and L-TEP, respectively (p = 0.3172) (Table 2). Emergent cases comprised acutely incarcerated and painful inguinal hernia that presented to the emergency department; they were not reducible and required surgical intervention within 24 h. A significantly higher proportion of complex cases were performed in the robotic group. Complex cases were any of four types: (1) recurrent cases from a previous TEP or TAPP procedure, (2) cases with previous prostatectomy, (3) cases that involved an incarcerated non-reducible inguinal hernia even after induction of anesthesia, and (4) cases of scrotal inguinal hernia. There were no significant differences between total surgical times, with all cases in both groups averaging approximately 69 min (p = 0.9843) (Table 2). Statistically similar times also characterized the two cohorts, based on unilateral and bilateral cases. Not surprising, unilateral surgical repair time was significantly shorter than bilateral hernia surgical repair time adjusted for cohort (R-TAPP vs. L-TEP): p = 0.0001. Comparison of surgical times for consecutive R-TAPP and L-TEP cases reveals decreasing operative times with the completion of more cases (Fig. 1). The mean surgical time for the initial six R-TAPP procedures was 128.5 ± 22.97 min and decreased to 63.3 ± 13.38 min R-TAPP cases 115–118. We saw similar decreases in time after completion of more cases in the L-TEP group from an initial time of 102.5 ± 9.28 min for the first 6 cases to 57.2 ± 6.20 min for cases 115–120.
Only one intraoperative complication occurred (subcutaneous emphysema), which was in the L-TEP group. There also was one conversion to laparotomy during the one complex L-TEP case due to the surgeon’s inability to reduce the hernia contents laparoscopically.
All L-TEP patients were discharged the same day as their surgeries, with the exception of an 87-year-old patient who stayed overnight due to lack of transportation. The R-TAPP patients also were discharged the same day as their surgeries with the exception of the following five patients. Two patients with urinary retention—an 83-year-old male and a 65-year-old male—each stayed overnight. A 78-year-old female, who underwent combined Nissen fundoplication and inguinal hernia repair, also stayed overnight. An 81-year-old female, who was an emergent case, had no help at home and therefore was placed in a rehabilitation center. She stayed two nights in the hospital before she could be transferred to the rehabilitation center. Last, a homeless 61-year-old male presented to the emergency room. The patient stayed overnight so that the social worker could plan his safe discharge.
There was no significant difference between cohorts regarding postoperative complications through the 3-month follow-up (R-TAPP, n = 8; L-TEP, n = 8; p = 0.6084). There were three re-admissions within 30 days in L-TEP group (syncope, n = 1; constipation and urinary retention, n = 1; hematoma, n = 1). Similar to R-TAPP, there were no episodes of surgical site infection, testicular atrophy, hydrocele, or orchitis.
Four re-admissions occurred within 30 days in the robotic group: atrial fibrillation (n = 2), Crohn’s flare (n = 1), and pneumonia (n = 1). Three re-admissions occurred within 30 days in the L-TEP group: hematoma (patient on warfarin) (n = 1), urinary retention and constipation (n = 1), and syncope (n = 1).
At the 3-month follow-up, the following complications were reported in the R-TAPP group: symptomatic seroma requiring drainage at the office (n = 2) and urinary retention requiring catheterization (n = 2). One patient had inguinodynia at 6 weeks (n = 1) but was lost to follow-up. In the L-TEP group, urinary retention requiring catheterization (n = 1), inguinodynia (n = 1), and symptomatic seroma requiring drainage (n = 2) were observed at 3-month follow-up.
At 1 year follow-up, there were no episodes of recurrence, surgical site infection, testicular atrophy, hydrocele, or orchitis in the robotic cohort. At the same follow-up, there was one recurrence in a L-TEP patient, who subsequently underwent successful R-TAPP repair. The patient with inguinodynia at 3 months had resolution of his symptoms by 7 months post-procedure and intervention was not required. One patient, who underwent L-TEP of a unilateral symptomatic inguinal hernia, required contralateral L-TEP repair of the other side within 1 year.
Discussion
This single-center, single-surgeon retrospective study compares results from 157 consecutive L-TEP inguinal hernia repairs and from 118 consecutive R-TAPP inguinal hernia repairs. Mean surgical times were almost identical between cohorts. Intraoperative and postoperative outcomes at 3 months and at 1 year also were similar with no significant differences in inguinodynia, seroma, or hernia recurrence. The low rate of recurrence in both groups at 1 year agrees with prior studies of laparoscopic and robotic inguinal hernia repair [13, 15].
A significantly greater number of complex cases were in the R-TAPP group (n = 11) than in the L-TEP group (n = 1). Six of the first twelve cases performed with R-TAPP were complex hernias, and these may have contributed to the long initial operative times and the initial learning curve associated with R-TAPP. All complex robotic cases were completed successfully without conversion, whereas the only complex laparoscopic case performed was converted to open due to the inability to reduce the hernia contents laparoscopically.
It is crucial to understand the robotic technology including the console, patient cart, and troubleshooting. Surgeons must spend adequate time learning the proper port placements, positioning the patient cart, and understanding the geometry behind the distance between robotic arms and reach for target anatomy. Proficiency with L-TEP, and perhaps with advanced laparoscopy in general, may facilitate the transition to robotic-assisted preperitoneal repair. For surgeons who are looking for a minimally invasive option to perform inguinal hernia repair, R-TAPP may be considered, especially for complex cases.
The principal limitation of the study was its single-center, single-surgeon retrospective design. Operative times and complications might vary significantly depending on the experience of multiple surgeons. The surgeon in this study gained experience performing L-TEP repair prior to beginning the R-TAPP approach. Thus, the challenges that one might experience learning the robotic-assisted preperitoneal approach without ever having gained proficiency with L-TEP may be underestimated. The study was also limited by the lack of any validated pain measurement and by the 1-year duration of follow-up, especially in terms of recurrence. Last, a detailed economic evaluation of the two approaches would require a longitudinal cost-of-care analysis, from procedure through postoperative follow-up, to fully explore and understand the impact that L-TEP and R-TAPP have on patient outcomes. Such an analysis would be elucidating, but it was beyond the scope of the study and of the available resources.
The robotic platform offers advanced ergonomics for the surgeon, superior imaging, and arms with 7 degrees of freedom permitting difficult cases to be performed while still maintaining a low complication rate and no significant increase in surgical time. For these reasons, R-TAPP may have a role in complex inguinal hernia repair, and this warrants further study. Surgeons, who are not willing to offer laparoscopy for certain complex hernias, may be able to offer patients a minimally invasive repair with a robotic approach.
Conclusion
This is the largest reported single-surgeon, single-site study comparing R-TAPP to L-TEP inguinal hernia repair. The results from R-TAPP consecutive cases, which included learning curve cases, were similar to those of matured laparoscopic cases for the same surgeon. The robotic platform may have facilitated the execution of complex hernia cases during the proficiency phase.
References
Bittner R, Montgomery MA, Arregui E, Bansal V et al (2015) Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society). Surg Endosc 29(2):289–321. doi:10.1007/s00464-014-3917-8
Neumayer L, Giobbie-Hurder A, Jonasson O et al (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350(18):1819–1827. doi:10.1056/NEJMoa040093
McCormack K, Scott NW, Go PM et al (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev 1:CD001785. doi:10.1002/14651858.CD001785
Trevisonno M, Kaneva P, Watanabe Y et al (2015) A survey of general surgeons regarding laparoscopic inguinal hernia repair: practice patterns, barriers, and educational needs. Hernia 19(5):719–724. doi:10.1007/s10029-014-1287-8
Haidenberg J, Kendrick ML, Meile T et al (2003) Totally extraperitoneal (TEP) approach for inguinal hernia: the favorable learning curve for trainees. Curr Surg 60(1):65–68. doi:10.1016/S0149-7944(02)00657-8
Schouten N, Simmermacher RK, van Dalen T et al (2013) Is there an end of the “learning curve” of endoscopic totally extraperitoneal (TEP) hernia repair? Surg Endosc 27(3):789–794. doi:10.1007/s00464-012-2512-0
McCormack K, Wake B, Perez J et al (2005) Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technol Assess 9(14):1–203
Yohannes P, Rotariu P, Pinto P et al (2002) Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Urology 60(1):39–45 discussion 45
Chandra V, Nehra D, Parent R et al (2010) A comparison of laparoscopic and robotic assisted suturing performance by experts and novices. Surgery 147(6):830–839. doi:10.1016/j.surg.2009.11.002
Schreuder HW, Wolswijk R, Zweemer RP et al (2012) Training and learning robotic surgery, time for a more structured approach: a systematic review. BJOG 119(2):137–149. doi:10.1111/j.1471-0528.2011.03139.x
Catchpole K, Perkins C, Bresee C et al (2015) Safety, efficiency and learning curves in robotic surgery: a human factors analysis. Surg Endosc. doi:10.1007/s00464-015-4671-2
Choi YY, Kim Z, Hur KY (2012) Learning curve for laparoscopic totally extraperitoneal repair of inguinal hernia. Can J Surg 55(1):33–36. doi:10.1503/cjs.019610
Escobar Dominguez JE, Ramos MG, Seetharamaiah R et al (2015) Feasibility of robotic inguinal hernia repair, a single-institution experience. Surg Endosc. doi:10.1007/s00464-015-4717-5
Satterthwaite FE (1946) An approximate distribution of estimates of variance components. Biom Bull 2:110–114
Cavazzola LT, Rosen MJ (2013) Laparoscopic versus open inguinal hernia repair. Surg Clin North Am 93(5):1269–1279. doi:10.1016/j.suc.2013.06.013
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Kudsi is a proctor and consultant for Intuitive Surgical and a consultant for Bard and Medtronic. Drs. McCarty, Paluvoi, and Mabardy have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Kudsi, O.Y., McCarty, J.C., Paluvoi, N. et al. Transition from Laparoscopic Totally Extraperitoneal Inguinal Hernia Repair to Robotic Transabdominal Preperitoneal Inguinal Hernia Repair: A Retrospective Review of a Single Surgeon’s Experience. World J Surg 41, 2251–2257 (2017). https://doi.org/10.1007/s00268-017-3998-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-3998-3