Abstract
Background
For patients with acute cholecystitis managed with percutaneous cholecystostomy (PC), the optimal duration of post-procedural antibiotic therapy is unknown. Our objective was to compare short versus long courses of antibiotics with the hypothesis that patients with persistent signs of systemic inflammation 72 h following PC would receive prolonged antibiotic therapy and that antibiotic duration would not affect outcomes.
Methods
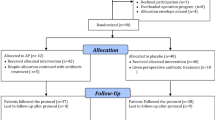
We performed a retrospective cohort analysis of 81 patients who underwent PC for acute cholecystitis at two hospitals during a 41-month period ending November 2014. Patients who received short (≤7 day) courses of post-procedural antibiotics were compared to patients who received long (>7 day) courses. Treatment response to PC was evaluated by systemic inflammatory response syndrome (SIRS) criteria. Logistic and linear regressions were used to evaluate associations between antibiotic duration and outcomes.
Results
Patients who received short (n = 30) and long courses (n = 51) of antibiotics had similar age, comorbidities, severity of cholecystitis, pre-procedural vital signs, treatment response, and culture results. There were no differences in recurrent cholecystitis (13 vs. 12%), requirement for open/converted to open cholecystectomy (23 vs. 22%), or 1-year mortality (20 vs. 18%). On logistic and linear regressions, antibiotic duration as a continuous variable was not predictive of any salient outcomes.
Conclusions
Patients who received short and long courses of post-PC antibiotics had similar baseline characteristics and outcomes. Antibiotic duration did not predict recurrent cholecystitis, interval open cholecystectomy, or mortality. These findings suggest that antibiotics may be safely discontinued within one week of uncomplicated PC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
When acute cholecystitis is managed with cholecystectomy and complete source control is obtained, prolonged postoperative antibiotic therapy is not warranted [1–3]. When patients with acute cholecystitis are too ill to tolerate surgery, they may be managed by decompressing the biliary tree with a percutaneous cholecystostomy (PC) tube. However, the optimal duration of antibiotic therapy following PC is unknown [4]. Ongoing gallbladder wall inflammation may not be mitigated by PC, especially in the context of gangrenous cholecystitis [5]. Even with a PC tube in place, the patient remains at risk for recurrent cholecystitis, particularly in the presence of calculi [6]. Faced with these challenges and a lack of evidence-based recommendations, patients may be subjected to unnecessarily prolonged antibiotic regimens. Previous work has shown that excessive antibiotic administration propagates multi-drug-resistant organisms [7–9], increases Clostridium difficile infection rates [10], and increases health care costs [11, 12]. Therefore, prudent antibiotic management following percutaneous cholecystectomy has the potential to make a significant impact.
The purpose of this study was to compare short (≤7 day) courses of antibiotics to long (>7 day) courses of antibiotics for patients managed with PC for acute cholecystitis. We hypothesized that patients with persistent systemic toxicity 72 h following PC would be more likely to receive prolonged antibiotic therapy and that antibiotic duration would not affect rates of recurrent cholecystitis, subsequent operative management strategies, or mortality.
Methods
We conducted a retrospective analysis of 81 patients who underwent PC for acute cholecystitis at two hospitals (a tertiary academic center and Veterans Affairs hospital) from June 1, 2011 to November 1, 2014. PC was performed by the transhepatic or transperitoneal route and was guided by computed tomography or ultrasound imaging. Patients age ≥18 and meeting the TG13 Tokyo definition of acute cholecystitis (right upper quadrant mass, pain, or tenderness along with fever, leukocytosis, elevated C-reactive protein, or imaging findings characteristic of acute cholecystitis) [13] were included. Patients transferred from outside institutions after endoscopic, radiographic, or surgical interventions on the biliary tree and those with concomitant cholangitis or gallstone pancreatitis were excluded. Patients were also excluded if PC was not technically successful, defined as cannulation of the gallbladder with aspiration of bile and/or purulence within three attempts [14]. Patients who died while on antibiotic therapy were excluded in order to ensure that antibiotic duration would not be confounded by early deaths. At both hospitals, cholecystostomy was offered as an alternative to cholecystectomy for high-risk surgical candidates with acute cholecystitis. The decision to perform cholecystostomy was reached through a shared decision-making process involving the patient and the treating physicians and was made on a case-by-case basis.
Data were retrospectively collected from the electronic medical record. Severity of acute cholecystitis was defined by the TG13 Tokyo guidelines (Grade I: mild, Grade I: moderate, Grade III: severe) [13]. Systemic inflammatory response syndrome (SIRS) criteria were defined as described by Davies and Hagen [15]. Clinical improvement was defined as resolution of the SIRS response, discontinuation of vasopressors, or discharge home within 72 h of PC. Clinical decline was defined as development of a new SIRS response or a new vasopressor requirement within 72 h of PC. The 72-hour time point to measure SIRS criteria was based on methods and results from previous studies [16–19]. Microbiologic culture data were recorded for each patient. Recurrent acute cholecystitis was defined as a new episode of acute cholecystitis occurring after a 48-h period in which the patient was off antibiotics and did not meet SIRS criteria. Decisions regarding duration of antibiotic therapy were at the discretion of the attending surgeon. Antibiotic therapy for ≤7 days was defined as a short course; antibiotic therapy for >7 days was defined as a long course. The 7-day cutoff allowed for comparison of more evenly sized groups (short course: n = 30; long course: n = 51). Differences in group sizes hindered analysis of a 5-day cutoff (short course: n = 20; long course: n = 61) or 3-day cutoff (short course: n = 12; long course: n = 79).
Statistical analysis was performed using SPSS (version 23, IBM, Armonk, NY). Normally distributed continuous variables were compared by one-way analysis of variance (reported as mean ± standard deviation), non-normally distributed continuous variables were compared by the Kruskal–Wallis test (reported as median [interquartile range]), and discrete variables were compared by Fisher’s exact test [reported as n (%)]. Correlations between antibiotic duration and salient outcomes were assessed by Pearson’s r. The ability of antibiotic duration to predict discrete and continuous outcome variables was determined with logistic and linear regressions as appropriate. Significance was set at α = 0.05, and confidence intervals for regression variables were set at 95%.
Results
There were no significant differences in the baseline characteristics of patients who received ≤7 days of antibiotic therapy and those that received >7 days of antibiotic therapy (Table 1). The two groups had similar age (65 vs. 70 years), Charlson comorbidity index (4.0 vs. 4.4), severity of acute cholecystitis (1.9 vs. 1.8), and clinical response to PC. Compared to the university hospital, patients managed at the Veterans Affairs hospital were older (73 vs. 65 years, p = 0.019), more likely to be male (93 vs. 53%, p < 0.001), and had higher Charlson comorbidity index scores (5.1 vs. 3.8, p = 0.015). VA and university hospital patients had similar rates of acalculous cholecystitis (17 vs. 20%, p > 0.999) and TG13 cholecystitis severity grade (1.8 vs. 1.8, p = 0.953). Acute cholecystitis was the admitting diagnosis in 73% of all patients. Patients who received ≤7 days of antibiotics were more likely to meet SIRS criteria at the time of PC (77 vs. 53%), though rates of SIRS were equal between groups 72 h after PC (13 vs. 14%). Of the four patients in the short-course group (13%) who had SIRS 72 h after PC, three patients (10%) still had SIRS at five days, and two patients (6%) had SIRS at 7 days. Of the seven patients (14%, p = 0.931) in the long-course group who had SIRS 72 after PC, three patients (6%, p = 0.665) still had SIRS at 5 days, and one (2%, p = 0.552) had SIRS at seven days. Of the three patients in the entire study population who had SIRS seven days following PC, two patients died within 30 days.
There were no differences in microbiologic findings between groups (Table 2). Seventy-seven out of 81patients (95%) had a bile culture performed, and 53 (69%) of these specimens contained bacteria (Table 2). There was a higher incidence of positive bile cultures in the prolonged antibiotic group, though the difference was not statistically significant (73 vs. 53%, p = 0.094). The most commonly isolated organisms were Escherichia coli, Klebsiella species, and Enterococcus faecalis. Thirty-seven percent of all specimens were polymicrobial. Compared to patients with a positive bile culture, patients with a negative bile culture had similar rates of SIRS at the time of PC (64 vs. 62%, p > 0.999) and SIRS 72 h after PC (28 vs. 16%, p = 0.308). Twelve patients (15%) had a bloodstream infection. In ten of these twelve patients (83%), the same organism was isolated in blood and bile cultures. There were no cases in which culture results required escalation or broadening of antibiotic therapy.
There was no significant difference in the proportion of patients with a non-biliary infection between the short-course and long-course groups (30 vs. 29%, p > 0.999). The proportion of patients who had two or more non-biliary infections was also similar between groups (7 vs. 4%, p = 0.624). Therefore, it seems unlikely that non-biliary infectious had a significant influence on the observed duration of antibiotic therapy between groups. There were no significant differences in the percentage of patients who had a stool culture to detect Clostridium difficile between short-course and long-course groups (23 vs. 14%, p = 0.363). There was one positive Clostridium difficile stool culture, which occurred in a patient in the long-course group (0 vs. 2%, p > 0999). There were no significant differences in the frequency of multi-drug-resistant infections for short-course and long-course groups (20 vs. 20%, p > 0.999). None of these infections occurred more than one calendar day after PC, and 75% of these cases involved a multi-drug-resistant organism in the bile culture.
Seventy-five patients (93%) had at least one follow-up clinic visit or subsequent hospital admission. The incidence of recurrent cholecystitis was similar between patients who received ≤7 days of antibiotic therapy (13%) and those that received >7 days of antibiotic therapy (12%). The two groups also had similar initial hospital length of stay, and rates of drain removal, interval cholecystectomy, requirement for open/converted to open cholecystectomy, and mortality at 30 days and one year (Table 3). A greater proportion of patients managed at the university hospital underwent interval cholecystectomy, though the difference was not statistically significant (49 vs. 27%, p = 0.062). Duration of antibiotic therapy did not have any significant associations with relevant outcomes by Pearson’s correlation, logistic regression, or linear regression (Table 4).
To address the possibility that outcomes were affected by disproportionate allocation of patients with a favorable clinical trajectory to the group that received a short-course of antibiotics, we performed a sensitivity analysis by excluding all patients who had SIRS at the time of PC, remained in the hospital 72 h after PC, and did not have SIRS at 72 h. This analysis excluded 15 patients in the short-course group and 16 patients in the long-course group. All parameters in Table 3 were assessed in the sensitivity analysis; there were no significant differences between groups. Short-course and long-course groups had similar hospital length of stay [6 (3–25) vs. 6 (3–10) days, p = 0.537], and similar rates of recurrent cholecystitis (7 vs. 11%, p > 0.999), drain removal (87 vs. 77%, p = 0.702), and cholecystectomy (47 vs. 46%, p > 0.999).
Discussion
Our data indicate that decisions regarding antibiotic therapy following PC for acute cholecystitis were arbitrary and that prolonged courses of antibiotics provided no benefit. We hypothesized that sicker patients would receive more than one week of antibiotics, and this was not the case. In fact, the group of patients who received ≤7 days of antibiotics had higher initial rates of SIRS, but improved over time such that the two groups had evenly matched SIRS criteria 72 h following PC. Microbiology data demonstrated that the groups had similar biliary and non-biliary infections, though there was a trend toward increased incidence of positive bile cultures in the prolonged antibiotic group, which may have affected decisions regarding antibiotic therapy [20–22]. There was a high degree of fidelity between organisms isolated from the blood and bile in patients with bloodstream infection. As expected, hospital length of stay and long-term outcomes were unaffected by antibiotic duration.
Rates of recurrent acute cholecystitis in this study were on the low end of the 10–41% range reported in the literature [6, 23–27]. This may be due to a combination of two factors: 7% of patients in this study had no documented follow-up in our system, and 19% had acalculous cholecystitis and were therefore at low risk of recurrent cholecystitis [28–31]. Cases of acalculous cholecystitis were included because ultrasound is only 84% sensitive (95% CI 76–92) in detecting cholelithiasis, and so many patients diagnosed with acalculous cholecystitis may actually have gallstones [32]. Also, inclusion of cases of presumed acalculous cholecystitis increased the sample size and allows our findings to be generalized to a broader population of all patients with acute cholecystitis.
The major limitations of this study are its retrospective design, small sample size. A larger study would reduce the likelihood of type II errors and allow for an adequately powered analysis of an even shorter duration of antibiotic therapy, e.g., 1–3 days. Unfortunately, there was no precedent for duration of antibiotic therapy following cholecystostomy tube placement in the literature prior to this study, and so the 7-day cutoff was based on our own practice patterns. Duration of antibiotic therapy was also analyzed as a continuous variable to decrease the likelihood that the 7 day cutoff concealed a true difference in outcomes for short versus long antibiotic therapy. Although immediate discontinuation of antibiotics following PC has not been studied, a short course of post-PC antibiotics seems prudent on the grounds that acute cholecystitis primarily involves inflammation of the gallbladder wall rather than its contents, and so decompression of the biliary tree may not address all aspects of the underlying pathophysiology [33]. In particular, a gangrenous necrotic gallbladder wall may be a source of ongoing inflammation and infection following PC [5]. Patients with this condition may be best managed by early cholecystectomy rather than extended antibiotic therapy [34]. Future studies should focus on appropriate selection of patients for PC and seek to determine whether even shorter courses of antibiotics are equally safe and effective.
Patients who received short (≤7 day) versus long (>7 day) courses of antibiotics following PC for acute cholecystitis had similar baseline characteristics, clinical response to PC, short-term outcomes, and long-term outcomes. Antibiotic duration was not predictive of recurrent cholecystitis, interval open cholecystectomy, or mortality. These findings suggest that antibiotics may be safely discontinued within one week of PC. Future studies should determine the efficacy of even shorter antibiotic courses (e.g., 1–3 days).
References
Lau WY, Yuen WK, Chu KW et al (1990) Systemic antibiotic regimens for acute cholecystitis treated by early cholecystectomy. Aust N Z J Surg 60(7):539–543
Regimbeau JM, Fuks D, Pautrat K et al (2014) Effect of postoperative antibiotic administration on postoperative infection following cholecystectomy for acute calculous cholecystitis: a randomized clinical trial. JAMA 312(2):145–154
Solomkin JS, Mazuski JE, Bradley JS et al (2010) Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis 50(2):133–164
Venara A, Carretier V, Lebigot J et al (2014) Technique and indications of percutaneous cholecystostomy in the management of cholecystitis in 2014. J Visc Surg 151(6):435–439
Merriam LT, Kanaan SA, Dawes LG et al (1999) Gangrenous cholecystitis: analysis of risk factors and experience with laparoscopic cholecystectomy. Surgery 126(4):680–685 discussion 685–686
Winbladh A, Gullstrand P, Svanvik J et al (2009) Systematic review of cholecystostomy as a treatment option in acute cholecystitis. HPB (Oxford) 11(3):183–193
Mcgowan JE (1983) Antimicrobial resistance in hospital organisms and its relation to antibiotic use. Rev Infect Dis 5(6):1033–1048
Arnold HM, Micek ST, Skrupky LP et al (2011) Antibiotic stewardship in the intensive care unit. Semin Respir Crit Care Med 32(2):215–227
de Man P, Verhoeven BA, Verbrugh HA et al (2000) An antibiotic policy to prevent emergence of resistant bacilli. Lancet 355(9208):973–978
Feazel LM, Malhotra A, Perencevich EN et al (2014) Effect of antibiotic stewardship programmes on Clostridium difficile incidence: a systematic review and meta-analysis. J Antimicrob Chemother 69(7):1748–1754
Dik JW, Vemer P, Friedrich AW et al (2015) Financial evaluations of antibiotic stewardship programs-a systematic review. Front Microbiol 6:317
Geissler A, Gerbeaux P, Granier I et al (2003) Rational use of antibiotics in the intensive care unit: impact on microbial resistance and costs. Intensive Care Med 29(1):49–54
Yokoe M, Takada T, Strasberg SM et al (2012) New diagnostic criteria and severity assessment of acute cholecystitis in revised Tokyo Guidelines. J Hepatobiliary Pancreat Sci 19(5):578–585
Saad WE, Wallace MJ, Wojak JC et al (2010) Quality improvement guidelines for percutaneous transhepatic cholangiography, biliary drainage, and percutaneous cholecystostomy. J Vasc Interv Radiol 21(6):789–795
Davies MG, Hagen PO (1997) Systemic inflammatory response syndrome. Br J Surg 84(7):920–935
Welschbillig-Meunier K, Pessaux P, Lebigot J et al (2005) Percutaneous cholecystostomy for high-risk patients with acute cholecystitis. Surg Endosc 19(9):1256–1259
Spira RM, Nissan A, Zamir O et al (2002) Percutaneous transhepatic cholecystostomy and delayed laparoscopic cholecystectomy in critically ill patients with acute calculus cholecystitis. Am J Surg 183(1):62–66
Chopra S, Dodd GD 3rd, Mumbower AL et al (2001) Treatment of acute cholecystitis in non-critically ill patients at high surgical risk: comparison of clinical outcomes after gallbladder aspiration and after percutaneous cholecystostomy. AJR Am J Roentgenol 176(4):1025–1031
Berber E, Engle KL, String A et al (2000) Selective use of tube cholecystostomy with interval laparoscopic cholecystectomy in acute cholecystitis. Arch Surg 135(3):341–346
Darkahi B, Sandblom G, Liljeholm H et al (2014) Biliary microflora in patients undergoing cholecystectomy. Surg Infect (Larchmt) 15(3):262–265
Galili O, Eldar S Jr, Matter I et al (2008) The effect of bactibilia on the course and outcome of laparoscopic cholecystectomy. Eur J Clin Microbiol Infect Dis 27(9):797–803
Thompson JE Jr, Bennion RS, Doty JE et al (1990) Predictive factors for bactibilia in acute cholecystitis. Arch Surg 125(2):261–264
Skillings JC, Kumai C, Hinshaw JR (1980) Cholecystostomy: A place in modern biliary surgery? Am J Surg 139(6):865–869
McKay A, Abulfaraj M, Lipschitz J (2012) Short- and long-term outcomes following percutaneous cholecystostomy for acute cholecystitis in high-risk patients. Surg Endosc 26(5):1343–1351
Jang WS, Lim JU, Joo KR et al (2015) Outcome of conservative percutaneous cholecystostomy in high-risk patients with acute cholecystitis and risk factors leading to surgery. Surg Endosc 29(8):2359–2364
Chang YR, Ahn YJ, Jang JY et al (2014) Percutaneous cholecystostomy for acute cholecystitis in patients with high comorbidity and re-evaluation of treatment efficacy. Surgery 155(4):615–622
Granlund A, Karlson BM, Elvin A et al (2001) Ultrasound-guided percutaneous cholecystostomy in high-risk surgical patients. Langenbecks Arch Surg 386(3):212–217
Eggermont AM, Lameris JS, Jeekel J (1985) Ultrasound-guided percutaneous transhepatic cholecystostomy for acute acalculous cholecystitis. Arch Surg 120(12):1354–1356
Berger H, Pratschke E, Arbogast H et al (1989) Percutaneous cholecystostomy in acute acalculous cholecystitis. Hepatogastroenterology 36(5):346–348
Shirai Y, Tsukada K, Kawaguchi H et al (1993) Percutaneous transhepatic cholecystostomy for acute acalculous cholecystitis. Br J Surg 80(11):1440–1442
Kirkegard J, Horn T, Christensen SD et al (2015) Percutaneous cholecystostomy is an effective definitive treatment option for acute acalculous cholecystitis. Scand J Surg 104(4):238–243
Shea JA, Berlin JA, Escarce JJ et al (1994) Revised estimates of diagnostic test sensitivity and specificity in suspected biliary tract disease. Arch Intern Med 154(22):2573–2581
Ambe PC, Zirngibl H (2015) The fate of patients managed with percutaneous cholecystostomy for acute cholecystitis. Surgery 159(5):1479–1480
Akyurek N, Salman B, Yuksel O et al (2005) Management of acute calculous cholecystitis in high-risk patients: percutaneous cholecystotomy followed by early laparoscopic cholecystectomy. Surg Laparosc Endosc Percutaneous Tech 15(6):315–320
Acknowledgements
This manuscript has not been submitted or published elsewhere, and the authors have nothing to disclose. The authors acknowledge Drs. Loretta Coady-Fariborzian, MD and Elisha Collins, MD for their assistance in obtaining IRB approval. This work was supported in part by R01 GM113945-01 (PAE), R01 GM105893-01A1 (AMM), P50 GM111152–01 (SCB, FAM, PAE, AMM) awarded by the National Institute of General Medical Sciences (NIGMS). TJL was supported by a post-graduate training Grant (T32 GM-08721) in burns, trauma and perioperative injury by NIGMS. Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR001427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Loftus, T.J., Brakenridge, S.C., Dessaigne, C.G. et al. Antibiotics May be Safely Discontinued Within One Week of Percutaneous Cholecystostomy. World J Surg 41, 1239–1245 (2017). https://doi.org/10.1007/s00268-016-3861-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3861-y