Abstract
Introduction
Enhanced recovery after surgery (ERAS) programs have been developed to improve patient outcomes, accelerate recovery after surgery, and reduce healthcare costs. ERAS programs are a multimodal approach, with interventions during all stages of care. This meta-analysis examines the impact of ERAS programs on patient outcomes and recovery.
Methods
A comprehensive search of all published randomized control trials (RCTs) assessing the use of ERAS programs in surgical patients was conducted. Outcomes analyzed were length of stay (LOS), overall mortality, 30-day readmission rates, total costs, total complications, time to first flatus, and time to first bowel movement.
Results
Forty-two RCTs involving 5241 patients were analyzed. ERAS programs significantly reduced LOS, total complications, and total costs across all types of surgeries (p < 0.001). Return of gastrointestinal (GI) function was also significantly improved, as measured by earlier time to first flatus and time to first bowel movement, p < 0.001. There was no overall difference in mortality or 30-day readmission rates; however, 30-day readmission rates after upper GI surgeries nearly doubled with the use of ERAS programs (RR = 1.922; p = 0.019).
Conclusions
ERAS programs are associated with a significant reduction in LOS, total complications, total costs, as well as earlier return of GI function. Overall mortality and readmission rates remained similar, but there was a significant increase in 30-day readmission rates after upper GI surgeries. ERAS programs are effective and a valuable part in improving patient outcomes and accelerating recovery after surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 321 million surgical procedures are performed annually worldwide, and the number is expected to rise with advances in technology and improvements in healthcare [1]. Persistent pain, gut dysfunction, and immobility often impede postoperative recovery and prolong hospitalization. Actions to support return to baseline function, however, can be taken without compromising patient safety and often even reduce complications. A compilation of these elements have been shown to be more beneficial than any single element alone [2]. These “enhanced recovery after surgery” (ERAS) programs have been developed and increasingly studied over the last few decades in an effort to improve patient outcomes and accelerate surgical recovery [3, 4].
ERAS programs consist of multidisciplinary and multifaceted approaches with interventions in all three phases of surgical patient care: preoperative, intraoperative, and postoperative [4]. Insulin resistance, prevention of postoperative infectious and respiratory complications, pain management, return of gastrointestinal (GI) function, and return to normal daily routine for the patient are all examples of outcomes that are targeted and assessed. Preoperative ERAS components aim to optimize the patient prior to surgery and include preadmission counseling, avoiding prolonged fasting, carbohydrate loading, selective use of bowel preparation, and antibiotic prophylaxis and thromboprophylaxis when necessary. Intraoperative ERAS components involving operative and anesthesia techniques include regional and local anesthetic blocks, avoidance of fluid overload, selective use of drains, and maintenance of normothermia, which minimizes disruption to the normal physiology. Postoperative ERAS components aim to enhance patient rehabilitation and recovery and include the avoidance of nasogastric tubes, early removal of catheters, drains, and chest tubes, prevention of postoperative nausea and vomiting, early oral nutrition, use of non-opioid oral analgesia, and early mobilization [4].
The first meta-analysis was published by Varadhan et al. in 2010 and included only six studies. This report demonstrated a significant reduction in length of stay (LOS) with the use of ERAS programs in elective open colorectal surgeries, but no difference in readmission or mortality rates [5]. More recently, Nicholson et al. [6] conducted a meta-analysis including 38 studies and demonstrated a significant overall reduction in LOS [standardized difference of means (SMD) = −1.15; 95% confidence interval (CI) −1.45 to −0.85; p < 0.05] and total complications [relative risk (RR) = 0.71; p < 0.05], with no significant difference in 30-day readmission or overall mortality with the use of ERAS programs. Limited subgroup analyses were conducted, and outcomes such as total hospital costs and return of GI function were not analyzed. Given that most studies involve colorectal surgeries, generalizations to other types of surgeries are difficult to make, and data into whether or not there are significant differences in the effectiveness of ERAS programs between different types of surgeries are lacking.
This current meta-analysis provides an updated comprehensive perspective on the impact of ERAS programs on various measures of patient outcome. Furthermore, this study aims to highlight the disparities within the published data and identify differences in the efficacy of these programs between different types of surgeries to guide future research.
Materials and methods
Study selection
A comprehensive search of all published RCTs evaluating the use of ERAS programs was conducted using PubMed, Cochrane Central Registry of Controlled Trials, and Google Scholar (1966–2016). The last search was conducted on February 11, 2016. Keywords used included combinations of “enhanced recovery after surgery,” “enhanced recovery after thoracic surgery,” “enhanced recovery program,” “fast track,” “ERAS,” and “ERATS.” RCTs comparing the use of an ERAS program with conventional standard of care, with ≥4 components of the ERAS program, were included.
Data extraction
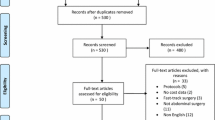
Articles retrieved were assessed for eligibility (Fig. 1). Primary clinical outcomes included hospital LOS, 30-day readmission rates, overall mortality within 30 days of surgery, and total costs. Total complications, time to first flatus, and time to first bowel movement were also analyzed. Cost analysis was conducted in US dollars (USD), with currency conversion rates on July 27, 2015 (1 RMB = 0.160974 USD, 1 Euro = 1.10629 USD, and 1 NZD = 0.660284 USD).
Statistical analysis
RR and 95% CI for categorical data and difference in means (MD) and 95% CI for continuous data were calculated. Meta-analysis of the pooled data was performed using Comprehensive Meta-Analysis software Version 3 (Biostat, Englewood, NJ, USA). A continuity correction factor of 0.5 was applied to studies with zero incidence to calculate the RR and variance. Both the fixed-effect model and random-effect model were considered, depending on the heterogeneity of the included studies. Heterogeneity between studies was assessed using both Cochrane’s Q statistic and I 2 statistic and considered statistically significant when p < 0.05 or I 2 > 50. If heterogeneity was observed, data were analyzed using a random-effect model, whereas a fixed-effect model was utilized in the absence of heterogeneity. Sensitivity analyses were conducted to determine the influence of each study on the overall relative risk estimates by removing each study in succession. Publication bias regarding the primary outcome (LOS) was visually evaluated by a funnel plot and quantitatively evaluated using Egger’s and Begg’s tests. A two-tailed p < 0.05 was considered statistically significant.
Results
Forty-two RCTs were identified, involving 5241 patients (2595 ERAS and 2646 standard of care) (Tables 1 and 2, and Supplementary Material).
Effects of ERAS programs on length of stay
Meta-analysis demonstrated a significant reduction in LOS by 2.35 days with the use of the ERAS program compared to standard of care (MD = −2.349 days; 95% CI −2.740 to −1.958; p < 0.001; Fig. 2).
Subgroup analysis identified a significant reduction in LOS among GI surgeries (MD = −2.39; 95% CI −2.801 to −1.975; p < 0.001), with similar reductions among both upper GI (MD = −2.360; 95% CI −3.172 to −1.547; p < 0.001) and colorectal (MD = −2.259; 95% CI −2.932 to −1.585; p < 0.001) surgeries. Significant reductions were also observed among genitourinary (MD = −1.835; 95% CI −3.556 to −0.115; p = 0.037) and orthopedic surgeries (MD = −2.998; 95% CI −5.457 to −0.539; p = 0.017) but not among the two studies involving thoracic surgery or the single study involving vascular surgery. No significant between group heterogeneity was observed (p = 0.921).
There were significantly greater reductions in LOS among studies in European countries (RR = −3.300; p < 0.001) compared to Asian countries (RR = −1.704; p < 0.001), p < 0.001. Similar variations were seen among all types of surgeries.
Effects of ERAS programs on readmission within 30 days
Meta-analysis showed no significant difference in 30-day readmission rates between the ERAS and control groups (RR = 1.151; p = 0.412; Fig. 3). There was no significant change in 30-day readmission rates among GI surgeries (RR = 1.138; p = 0.457).
There was a significant increase in 30-day readmission rates among upper GI surgery (RR = 1.922; 95% CI 1.111–3.324; p = 0.019), but no significant difference in 30-day readmission rates among colorectal or genitourinary surgeries. The single study involving vascular surgery reported zero readmissions in both groups.
Effects of ERAS program on total cost of hospital stay
Meta-analysis showed a significant reduction in the total cost of hospital stay between the ERAS and control groups (MD = −$639.064; 95% CI −933.850 to −344.278; p < 0.001; Fig. 4).
Subgroup analysis identified a significant reduction in total costs among upper GI (MD = −$591.609; 95% CI −$904.987 to −$278.232; p < 0.001) and colorectal surgeries (MD = −$1003.790; 95% CI −$1872.567 to −$135.012; p = 0.024). Cost data were not reported from any of the thoracic, vascular, or orthopedic surgery studies.
Effects of ERAS programs on postoperative complications
Meta-analysis showed a significant 38.0% reduction in the risk of postoperative complications between the ERAS and control groups (RR = 0.620; 95% CI 0.545–0.704; p < 0.001; Fig. 5). Similarly, a 27.2% reduction was seen among GI surgeries.
Subgroup analysis identified a significant reduction in the risk of postoperative complications following upper GI (RR = 0.606; 95% CI 0.473–0.778; p < 0.001), colorectal (RR = 0.634; 95% CI 0.542–0.741; p < 0.001), and genitourinary surgeries (RR = 0.429; 95% CI 0.197–0.934; p = 0.033). No significant reduction in the risk of complications in the one thoracic surgery study was observed.
There were significant reductions in the risk of pulmonary complications by 57.3% (RR = 0.427; 95% CI 0.307–0.594; p < 0.001), cardiac complications by 52.7% (RR = 0.473; 95% CI 0.291–0.767; p = 0.002), and surgical site infections by 27.2% (RR = 0.728; 95% CI 0.560–0.948; p = 0.018) with the use of ERAS programs. No significant reduction in anastomotic leaks was observed (RR = 0.806; p = 0.308). Reductions in all types of complications following each type of surgery were observed.
Effects of ERAS programs on return of gastrointestinal function
Meta-analysis showed a significant reduction in time to first flatus between the ERAS and control groups (MD = −13.119 h; 95% CI −17.980 to −8.257; p < 0.001; Fig. 6). Subgroup analysis identified earlier time to first flatus after both upper GI (MD = −9.323; 95% CI −14.760 to −3.886; p = 0.001) and colorectal surgeries (MD = −28.247; 95% CI −39.101 to −17.392; p < 0.001).
Meta-analysis showed a significant reduction in time to first bowel movement between the ERAS group and control groups (MD = −33.860 h; 95% CI −43.276 to −24.444; p < 0.001; Fig. 7). Subgroup analysis identified earlier time to first bowel movement after both upper GI (MD = −33.765; 95% CI –50.836 to −16.695; p < 0.001) and colorectal surgeries (MD = −33.901; 95% CI −45.190 to −22.612; p < 0.001).
Effects of ERAS programs on mortality
Meta-analysis showed no significant reduction in the risk of mortality (RR = 0.708; p = 0.283; Fig. 8). Similarly, there was no significant reduction in the risk of mortality among thoracic, upper GI, colorectal, or orthopedic surgeries, and no significant between group heterogeneity was observed (p = 0.898).
Laparoscopic versus open techniques
Although ERAS programs significantly reduced LOS in both laparoscopic (MD = −1.00; p < 0.001) and open (MD = −2.441; p < 0.001) colorectal surgeries, there was a significantly greater reduction seen among open surgeries (p < 0.001). No significant difference was found among readmission rates (RR = 0.680; p = 0.665 for laparoscopic and RR = 1.065; p = 0.914 for open) or overall mortality (RR = 3.060; p = 0.490 for laparoscopic and RR = 0.586; p = 0.556 for open).
Subgroup analysis comparing laparoscopic and open techniques was not performed for non-colorectal surgeries, due to insufficient number of studies.
Sensitivity analyses
Similar overall effect estimates for length of stay, 30-day readmission rates, overall mortality, total hospital costs, postoperative complications, time to first flatus, and time to first bowel movement were observed with the removal of any single study.
Publication bias
There was no asymmetry on the funnel plot and no evidence of publication bias for the primary end point (LOS) by either the Egger’s (p = 0.109) or Begg’s test (p = 0.722).
Discussion
Surgery represents a major trauma to the body, triggering a cascade of physiological responses, collectively termed the stress response [7]. Surgical recovery is a complex process encompassing physical, psychological, social, and economic factors [8, 9]. ERAS programs involve evidence-based perioperative care elements aimed at addressing issues such as insulin resistance, pain management, return of GI function, and the prevention of postoperative infections and respiratory complications [7, 10]. When integrated together, ERAS programs seek to improve patient recovery and outcomes, by reducing complications and facilitating earlier hospital discharge [7, 10].
The current meta-analysis demonstrates that ERAS programs are associated with significant reductions in LOS, total hospital costs, total complications, and earlier return of GI function, with no difference in overall mortality or 30-day readmission rates, which is consistent with previous meta-analyses [6, 11]. In particular, significant reductions in SSIs, cardiac and pulmonary complications were seen. By reducing postoperative complications, ERAS programs reduce the need for hospitalization, and in turn, decrease LOS and total costs. Despite extensive available data documenting the effectiveness of ERAS, significant disparities between published studies exists. Moreover, a majority of studies have involved only colorectal surgeries, and significant differences exist between the LOS reductions observed between different types of surgeries.
Nearly all published studies involving colorectal surgery patients, and ERAS programs have shown reductions in LOS, overall complication rates, and readmission rates in both open and laparoscopic cases. A greater reduction in LOS was observed with open surgeries, possibly attributable to the longer LOS associated with open surgeries compared to laparoscopic surgeries. Similarly, a meta-analysis by Greco et al. [11] reported a significant reduction in overall morbidity by 40% and LOS by 2.28 days, without increasing readmission rates. Furthermore, there were no significant differences in readmission rates or mortality between the laparoscopic and open approach, concluding that laparoscopic surgery with the ERAS program does not compromise patients safety [12].
ERAS programs have proved beneficial in reducing postoperative complications, LOS, and total costs associated with upper GI surgeries. However, this appears to come at a cost of a significant increase in 30-day readmission rates following. It has been speculated that increased postoperative complications in the elderly may contribute to the higher readmission rates. Although there were insufficient number of studies involving elderly patients to allow for a subgroup analysis, Bu et al. [13] reported a significant increase in readmission rates with the use of ERAS programs among the elderly patients aged 75–89 years, but not adult patients age 45–74 years, which were attributed to an increase in postoperative complications including nausea and vomiting, intestinal obstruction, and anastomotic leaks with the use of ERAS programs among the elderly patients.
In addition to improved patient outcomes, ERAS programs have been reported to improve quality of life (QOL) and patient satisfaction. Wang et al. [14] studied 117 patients undergoing colorectal surgery and reported higher QOL scores within the first 21 days among patients with the ERAS program, but similar QOL scores at day 28. A pre- and post-implementation study by Wu et al. [15] reported an improvement in patient satisfaction scores from the 37th percentile pre-implementation to >97th percentile post-implementation.
Despite the documented benefits of the ERAS programs, adoption has been slow, and multiple barriers to full implementation and utilization have been recognized [16–19]. Limited hospital resources and lack of manpower and time are most often cited as the major barriers to implementation [16]. However, ERAS programs also reduce total hospital costs and have shown to be cost-effective with savings evident in the initial implementation period [20, 21]. Johns Hopkins Hospital developed a model of net financial costs involved with implementing the ERAS program among colorectal surgeries [22]. Despite the high costs ($522,783) associated with implementing the ERAS program, there was a substantial $948,500 cost savings in just the first year, resulting in a net savings of $395,717. Savings were mostly a direct result of decreased LOS, with estimated cost reductions ranging from $830 to $3100 per day [22].
Although the results of this meta-analysis are significant, there are limitations to this study due to the variation and heterogeneity of the RCTs. The patient demographics, type of surgery, and the specific ERAS components utilized differed between the studies. Standard of care practices and average LOS also varies by country. Most studies included in this meta-analysis involved GI surgery, and only a limited number of studies examined orthopedic, thoracic, and vascular surgeries. Few studies involved the elderly patient population, and additional RCTs studying the safety and efficacy of the ERAS program in the elderly is required. This study only included elective surgeries; however, published studies have also demonstrated the benefits of ERAS programs among emergency surgeries. Lastly, ERAS programs primarily target patient outcomes prior to hospital discharge, while complete surgical recovery extends past hospital discharge. Long-term recovery and return of pre-surgical function and activities are rarely studied and require further studies.
Despite these limitations, ERAS programs are an effective and valuable tool for improving patient outcomes and accelerating recovery after surgery. By significantly reducing postoperative complications, including SSIs, ERAS programs reduce LOS and total costs. Given the number of surgical procedures performed, the risk of morbidity and mortality associated with surgery, and the significant reduction in LOS and total complications, surgeons should consider implementing ERAS programs in the care of surgical patients.
References
Rose J, Weiser TG, Hider P, Wilson L, Gruen RL, Bickler SW (2015) Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health Estimate. Lancet Glob Health 3(Suppl 2):S13–S20
Fearon KC, Ljungqvist O, Von MM, Revhaug A, Dejong CH, Lassen K et al (2005) Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 24(3):466–477
Kehlet H, Wilmore DW (2002) Multimodal strategies to improve surgical outcome. Am J Surg 183(6):630–641
Nanavati AJ, Prabhakar S (2014) Fast-track surgery: toward comprehensive peri-operative care. Anesth Essays Res 8(2):127–133
Varadhan KK, Neal KR, Dejong CH, Fearon KC, Ljungqvist O, Lobo DN (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr 29(4):434–440
Nicholson A, Lowe MC, Parker J, Lewis SR, Alderson P, Smith AF (2014) Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg 101(3):172–188
Carli F (2015) Physiologic considerations of Enhanced Recovery After Surgery (ERAS) programs: implications of the stress response. Can J Anaesth 62(2):110–119
Neville A, Lee L, Antonescu I, Mayo NE, Vassiliou MC, Fried GM et al (2014) Systematic review of outcomes used to evaluate enhanced recovery after surgery. Br J Surg 101(3):159–170
Feldman LS, Lee L, Fiore J Jr (2015) What outcomes are important in the assessment of Enhanced Recovery After Surgery (ERAS) pathways? Can J Anaesth 62(2):120–130
Nygren J, Thacker J, Carli F, Fearon KC, Norderval S, Lobo DN et al (2012) Guidelines for perioperative care in elective rectal/pelvic surgery: enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Clin Nutr 31(6):801–816
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M (2014) Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg 38(6):1531–1541. doi:10.1007/s00268-013-2416-8
Lei QC, Wang XY, Zheng HZ, Xia XF, Bi JC, Gao XJ et al (2015) laparoscopic versus open colorectal resection within fast track programs: an Update meta-analysis based on randomized controlled trials. J Clin Med Res 7(8):594–601
Bu J, Li N, Huang X, He S, Wen J, Wu X (2015) Feasibility of fast-track surgery in elderly patients with gastric cancer. J Gastrointest Surg 19(8):1391–1398
Wang H, Zhu D, Liang L, Ye L, Lin Q, Zhong Y et al (2015) Short-term quality of life in patients undergoing colonic surgery using enhanced recovery after surgery program versus conventional perioperative management. Qual Life Res 24(11):2663–2670
Wu CL, Benson AR, Hobson DB, Roda CP, Demski R, Galante DJ et al (2015) Initiating an enhanced recovery pathway program: an anesthesiology department’s perspective. Jt Comm J Qual Patient Saf 41(10):447–456
Pearsall EA, Meghji Z, Pitzul KB, Aarts MA, McKenzie M, McLeod RS et al (2015) A qualitative study to understand the barriers and enablers in implementing an enhanced recovery after surgery program. Ann Surg 261(1):92–96
Kahokehr A, Sammour T, Zargar-Shoshtari K, Thompson L, Hill AG (2009) Implementation of ERAS and how to overcome the barriers. Int J Surg 7(1):16–19
Hughes M, Coolsen MM, Aahlin EK, Harrison EM, McNally SJ, Dejong CH et al (2015) Attitudes of patients and care providers to enhanced recovery after surgery programs after major abdominal surgery. J Surg Res 193(1):102–110
Lyon A, Solomon MJ, Harrison JD (2014) A qualitative study assessing the barriers to implementation of enhanced recovery after surgery. World J Surg 38(6):1374–1380. doi:10.1007/s00268-013-2441-7
Roulin D, Donadini A, Gander S, Griesser AC, Blanc C, Hubner M et al (2013) Cost-effectiveness of the implementation of an enhanced recovery protocol for colorectal surgery. Br J Surg 100(8):1108–1114
Stowers MD, Lemanu DP, Hill AG (2015) Health economics in Enhanced Recovery After Surgery programs. Can J Anaesth 62(2):219–230
Stone AB, Grant MC, Pio RC, Hobson D, Pawlik T, Wu CL et al (2016) Implementation costs of an enhanced recovery after surgery program in the United States: a financial model and sensitivity analysis based on experiences at a quaternary academic medical center. J Am Coll Surg 222(3):219–225
Anderson AD, McNaught CE, MacFie J, Tring I, Barker P, Mitchell CJ (2003) Randomized clinical trial of multimodal optimization and standard perioperative surgical care. Br J Surg 90(12):1497–1504
Delaney CP, Zutshi M, Senagore AJ, Remzi FH, Hammel J, Fazio VW (2003) Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative care after laparotomy and intestinal resection. Dis Colon Rectum 46(7):851–859
Gatt M, Anderson AD, Reddy BS, Hayward-Sampson P, Tring IC, MacFie J (2005) Randomized clinical trial of multimodal optimization of surgical care in patients undergoing major colonic resection. Br J Surg 92(11):1354–1362
Recart A, Duchene D, White PF, Thomas T, Johnson DB, Cadeddu JA (2005) Efficacy and safety of fast-track recovery strategy for patients undergoing laparoscopic nephrectomy. J Endourol 19(10):1165–1169
Petersen MK, Madsen C, Andersen NT, Soballe K (2006) Efficacy of multimodal optimization of mobilization and nutrition in patients undergoing hip replacement: a randomized clinical trial. Acta Anaesthesiol Scand 50(6):712–717
Gralla O, Haas F, Knoll N, Hadzidiakos D, Tullmann M, Romer A et al (2007) Fast-track surgery in laparoscopic radical prostatectomy: basic principles. World J Urol 25(2):185–191
Khoo CK, Vickery CJ, Forsyth N, Vinall NS, Eyre-Brook IA (2007) A prospective randomized controlled trial of multimodal perioperative management protocol in patients undergoing elective colorectal resection for cancer. Ann Surg 245(6):867–872
Larsen K, Sorensen OG, Hansen TB, Thomsen PB, Soballe K (2008) Accelerated perioperative care and rehabilitation intervention for hip and knee replacement is effective: a randomized clinical trial involving 87 patients with 3 months of follow-up. Acta Orthop 79(2):149–159
Muehling BM, Halter GL, Schelzig H, Meierhenrich R, Steffen P, Sunder-Plassmann L et al (2008) Reduction of postoperative pulmonary complications after lung surgery using a fast track clinical pathway. Eur J Cardiothorac Surg 34(1):174–180
Borgwardt L, Zerahn B, Bliddal H, Christiansen C, Sylvest J, Borgwardt A (2009) Similar clinical outcome after unicompartmental knee arthroplasty using a conventional or accelerated care program: a randomized, controlled study of 40 patients. Acta Orthop 80(3):334–337
Ionescu D, Iancu C, Ion D, Al-Hajjar N, Margarit S, Mocan L et al (2009) Implementing fast-track protocol for colorectal surgery: a prospective randomized clinical trial. World J Surg 33(11):2433–2438. doi:10.1007/s00268-009-0197-x
Muehling B, Schelzig H, Steffen P, Meierhenrich R, Sunder-Plassmann L, Orend KH (2009) A prospective randomized trial comparing traditional and fast-track patient care in elective open infrarenal aneurysm repair. World J Surg 33(3):577–585. doi:10.1007/s00268-008-9892-2
Muller S, Zalunardo MP, Hubner M, Clavien PA, Demartines N (2009) A fast-track program reduces complications and length of hospital stay after open colonic surgery. Gastroenterology 136(3):842–847
Serclova Z, Dytrych P, Marvan J, Nova K, Hankeova Z, Ryska O et al (2009) Fast-track in open intestinal surgery: prospective randomized study (Clinical Trials Gov Identifier no. NCT00123456). Clin Nutr 28(6):618–624
Liu XX, Jiang ZW, Wang ZM, Li JS (2010) Multimodal optimization of surgical care shows beneficial outcome in gastrectomy surgery. J Parenter Enter Nutr 34(3):313–321
Wang D, Kong Y, Zhong B, Zhou X, Zhou Y (2010) Fast-track surgery improves postoperative recovery in patients with gastric cancer: a randomized comparison with conventional postoperative care. J Gastrointest Surg 14(4):620–627
Demanet J, Wattier JM, Colin P, Fantoni JC, Villers A, Lebuffe G (2011) Feasibility of fast track strategy for patients undergoing radical nephrectomy: a prospective randomized study: 8AP4-10. Eur J Anaesth 28(Suppl 48):120
Garcia-Botello S, de Canovas LR, Tornero C, Escamilla B, Espi-Macias A, Esclapez-Valero P et al (2011) Implementation of a perioperative multimodal rehabilitation protocol in elective colorectal surgery. A prospective randomised controlled study. Cir Esp 89(3):159–166
Lee TG, Kang SB, Kim DW, Hong S, Heo SC, Park KJ (2011) Comparison of early mobilization and diet rehabilitation program with conventional care after laparoscopic colon surgery: a prospective randomized controlled trial. Dis Colon Rectum 54(1):21–28
Roig JV, Garcia-Fadrique A, Salvador A, Villalba FL, Tormos B, Lorenzo-Linan MA et al (2011) Selective intestinal preparation in a multimodal rehabilitation program. Influence on preoperative comfort and the results after colorectal surgery. Cir Esp 89(3):167–174
Sokouti M, Aghdam BA, Golzari SE, Moghadaszadeh M (2011) A comparative study of postoperative pulmonary complications using fast track regimen and conservative analgesic treatment: a randomized clinical trial. Tanaffos 10(3):12–19
Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF et al (2011) Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg 254(6):868–875
Wang G, Jiang ZW, Xu J, Gong JF, Bao Y, Xie LF et al (2011) Fast-track rehabilitation program vs conventional care after colorectal resection: a randomized clinical trial. World J Gastroenterol 17(5):671–676
Chen HJ, Xin JL, Cai L, Tao ZH, Yuan HS, Bing CH et al (2012) Preliminary experience of fast-track surgery combined with laparoscopy-assisted radical distal gastrectomy for gastric cancer. J Gastrointest Surg 16(10):1830–1839
Kim YM, Yim HW, Jeong SH, Klem ML, Callaway CW (2012) Does therapeutic hypothermia benefit adult cardiac arrest patients presenting with non-shockable initial rhythms?: a systematic review and meta-analysis of randomized and non-randomized studies. Resuscitation 83(2):188–196
Ren L, Zhu D, Wei Y, Pan X, Liang L, Xu J et al (2012) Enhanced Recovery After Surgery (ERAS) program attenuates stress and accelerates recovery in patients after radical resection for colorectal cancer: a prospective randomized controlled trial. World J Surg 36(2):407–414. doi:10.1007/s00268-011-1348-4
Wang G, Jiang Z, Zhao K, Li G, Liu F, Pan H et al (2012) Immunologic response after laparoscopic colon cancer operation within an enhanced recovery program. J Gastrointest Surg 16(7):1379–1388
Wang G, Jiang ZW, Zhao K, Gao Y, Liu FT, Pan HF et al (2012) Fast track rehabilitation programme enhances functional recovery after laparoscopic colonic resection. Hepatogastroenterology 59(119):2158–2163
Yang D, He W, Zhang S, Chen H, Zhang C, He Y (2012) Fast-track surgery improves postoperative clinical recovery and immunity after elective surgery for colorectal carcinoma: randomized controlled clinical trial. World J Surg 36(8):1874–1880. doi:10.1007/s00268-012-1606-0
Feng F, Ji G, Li JP, Li XH, Shi H, Zhao ZW et al (2013) Fast-track surgery could improve postoperative recovery in radical total gastrectomy patients. World J Gastroenterol 19(23):3642–3648
Jones C, Kelliher L, Dickinson M, Riga A, Worthington T, Scott MJ et al (2013) Randomized clinical trial on enhanced recovery versus standard care following open liver resection. Br J Surg 100(8):1015–1024
Lemanu DP, Singh PP, Berridge K, Burr M, Birch C, Babor R et al (2013) Randomized clinical trial of enhanced recovery versus standard care after laparoscopic sleeve gastrectomy. Br J Surg 100(4):482–489
Ni CY, Yang Y, Chang YQ, Cai H, Xu B, Yang F et al (2013) Fast-track surgery improves postoperative recovery in patients undergoing partial hepatectomy for primary liver cancer: a prospective randomized controlled trial. Eur J Surg Oncol 39(6):542–547
Feng F, Li XH, Shi H, Wu GS, Zhang HW, Liu XN et al (2014) Fast-track surgery combined with laparoscopy could improve postoperative recovery of low-risk rectal cancer patients: a randomized controlled clinical trial. J Dig Dis 15(6):306–313
Gonenc M, Dural AC, Celik F, Akarsu C, Kocatas A, Kalayci MU et al (2014) Enhanced postoperative recovery pathways in emergency surgery: a randomised controlled clinical trial. Am J Surg 207(6):807–814
Jia Y, Jin G, Guo S, Gu B, Jin Z, Gao X et al (2014) Fast-track surgery decreases the incidence of postoperative delirium and other complications in elderly patients with colorectal carcinoma. Langenbecks Arch Surg 399(1):77–84
Li K, Li JP, Peng NH, Jiang LL, Hu YJ, Huang MJ (2014) Fast-track improves post-operative nutrition and outcomes of colorectal surgery: a single-center prospective trial in China. Asia Pac J Clin Nutr 23(1):41–47
Lu H, Fan Y, Zhang F, Li G, Zhang C, Lu L (2014) Fast-track surgery improves postoperative outcomes after hepatectomy. Hepatogastroenterology 61(129):168–172
Mari GM, Costanzi A, Maggioni D, Origi M, Ferrari GC, De MP et al (2014) Fast-track versus standard care in laparoscopic high anterior resection: a prospective randomized-controlled trial. Surg Laparosc Endosc Percutaneous Tech 24(2):118–121
Nanavati AJ, Prabhakar S (2014) A comparative study of ‘fast-track’ versus traditional peri-operative care protocols in gastrointestinal surgeries. J Gastrointest Surg 18(4):757–767
Zhao G, Cao S, Cui J (2014) Fast-track surgery improves postoperative clinical recovery and reduces postoperative insulin resistance after esophagectomy for esophageal cancer. Support Care Cancer 22(2):351–358
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lau, C.S.M., Chamberlain, R.S. Enhanced Recovery After Surgery Programs Improve Patient Outcomes and Recovery: A Meta-analysis. World J Surg 41, 899–913 (2017). https://doi.org/10.1007/s00268-016-3807-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3807-4