Abstract
Despite an increasing burden of injuries, prehospital transport systems remain underdeveloped in many low- and middle-income countries. Little information exists on the use of prehospital services for trauma patients in Zambia.
Method
A prospective, observational study of trauma presentations was undertaken for 6 months in Lusaka, Zambia, to establish the epidemiology and outcomes of injury in the region. In addition to demographics and mechanism of injury, data were collected on prehospital transport as well as inpatient resources utilization. Trained study personnel gathered data on trauma presentations 24 h a day. Statistical analysis was conducted using SAS 9.3 from a Microsoft® Access database.
Results
3498 trauma patients were enrolled in the study on arrival to University Teaching Hospital (UTH). 3264 patients had a transport means recorded (95.3 %). Two-thirds (66 %) arrived within 6 h of injury, and 23 % arrived within the first hour after injury. A majority arrived by private vehicle (53.4 %) or public transport (37.7 %); only 5.9 % were transported by public or private ambulance. Of those arriving within the first hour after injury, 69.1 % came by private car, 24.6 % by public transport and 3.1 % by ambulance. There was a small statistical increase in Kampala Trauma Score II among ambulance arrivals.
Conclusion
Trauma patient use a variety of transport methods to get to UTH. A majority of patients use no formal ambulance transport. Despite this fact, a majority arrives within 6 h of injury but receive no formal prehospital care. An integrated, multilayered prehospital care and transport system may be the most effective approach for Zambia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 2013, 973 million people suffered injuries requiring health services and 4.8 million died from injuries [1]. Previous studies have indicated that 90 % of injury deaths occur in low- and middle-income countries (LMICs) [2]. Survival from severe injuries is linked to rapid initiation of treatment. Achieving this goal requires a system of prehospital transport—formal or informal—to assist those who could not otherwise reach care due to physical or resource limitations. This essential component of effective emergency care is lacking in many LMICs. When present, such systems are varied in type, limited in scope, hampered by long distances and poor infrastructure, and are most frequently used by either wealthy individuals or for inter-facility transport [3–6].
Prehospital systems and their performance are poorly studied in low-resource settings. The paucity of high-quality research on emergency and prehospital care in LMICs results in a critical lack of data for planning and an underestimate of the public health problem posed by the lack of such services [7, 8].
The insufficient availability of prehospital transport is especially acute in Africa despite data that show the majority of trauma fatalities in Africa occur before an injured patient ever receives care [3]. Reasons cited for this gap in emergency services include difficulty in providing adequate coverage to dispersed populations over large distances, as well as the perceived high cost of providing prehospital care on the model of high-income countries.
Recent studies in LMICs, however, have cited the effective use of diverse prehospital transport methods including private vehicles, public transport, commercial transport, police transport, nonmotorized transport, as well as formal Emergency Medical Services (EMS) [9–12]. Since a higher proportion of patients in LMICs with salvageable injuries die outside the hospital than in high-income countries [4], emphasis must be made on prioritizing rapid transport of sick and injured patients by any means to health facilities.
Over a 6-month period, a trauma registry at University Teaching Hospital (UTH) in Lusaka, Zambia, was established to study the epidemiology and outcomes of injury within the Lusaka area. The goal of this portion of the trauma study was to assess the patterns of prehospital transport for trauma patients, as well as evaluate whether those methods were related to either injury severity or time to presentation for care.
Materials and methods
From September 2011 to February 2012 a prospective, observational study was conducted to capture data on trauma patients presenting to UTH in Lusaka, Zambia—a 1400-bed urban, tertiary hospital that is the primary referral hospital for 1.5 million people in Lusaka and the academic referral hospital for the country.
The hospital Accident and Emergency (A&E) departments are divided by specialty with four main A&E units—surgical (casualty), medical, pediatric, and obstetric. Patients presenting to A&E units are cared for 24 h a day by nurses, clinical officers, and physicians overseen by consultant physicians. Resources at UTH include full laboratory and blood bank services, an intensive care unit, a radiology department with available radiography, computed tomography, magnetic resonance, and ultrasound imaging (the latter three modalities are not routinely used for emergency patients) and operating theaters available 24 h a day.
Data were collected by dedicated research staff on all trauma presentations (including pediatric trauma patients) using a standardized data collection instrument. Data were collected contemporaneously at the time of the trauma presentations. Data were abstracted from the clinical records and supplemented when necessary by direct interview of the patient or their representative. Research personnel were trained in study protocols, use of study instruments, and research ethics. Most were nurses, ancillary medical staff or medical students but had no clinical responsibilities while collecting data. Inpatient data collection occurred twice daily on the wards and intensive care unit to capture outcomes and inpatient resource utilization. Principal Investigators and a Nurse Study Coordinator provided oversight of the data collection.
Registry data included demographics (age, gender, residence, and occupation); injury (injury mechanism, circumstances, location, and time); prehospital transport (method and timing of transport to the hospital); as well as clinical data (vital signs, injuries, and body locations affected, A&E disposition). For admitted patients, resource utilization data were recorded including length of stay, HIV testing, operative procedures, use of blood products, and 30-day vital status. An injury severity score was calculated for each patient using the revised Kampala Trauma Score (KTS II) [13–15].
Data were recorded on study forms and entered into an electronic database using Teleforms®. Teleforms® enables hand-written text to be translated to computer readable files and data was then stored in a Microsoft® Access database. Data were analyzed using SAS (9.3, SAS Institute, Cary, NC, USA) for all data summaries and statistical analyses.
Quantitative data were summarized using frequencies and proportions for categorical variables; means and medians were used for continuous variables. χ 2 tests were used to test for differences in categorical variables. After establishing normality of distribution, t-tests were used to test for differences in continuous variables. In order to rule out any bias introduced by excluding 1195 patients with missing data from length of stay (LOS) outcomes, transportation method, KTS II score, and mortality were compared between patients with LOS data and those missing LOS data using a χ 2 test.
Results
This study captured data on 3498 trauma patients presenting to the surgical casualty ward at UTH in Lusaka from September 2011 to February 2012 (3425 arrived alive, 73 patients coded as “brought in dead”). Figure 1 shows the study profile of trauma registry patients.
Transport method and time to hospital
Of the 3425 patients arriving alive to the hospital, data on transport method and transit time are available for 3264 individuals (95.3 %). Despite being a regional and national referral hospital, 66 % of patients arrived within 6 h of the original injury and about a quarter of patients (23 %) arrived within 1 h of injury.
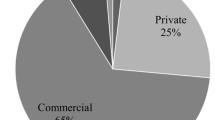
The majority of trauma patients arrived via private car (1743, 53.4 %) or public transport (1231, 37.7 %). Only a small number of patients arrived via any form of ambulance (194, 5.9 %). While the type of vehicle was also a variable to be collected, this data element was recorded 23 % of the time (primarily for patients involved in road traffic accidents) and was excluded from overall analysis. Of 745 patients arriving within the first “golden hour,” 95.0 % presented using private or public transport. The remainder used public or private ambulance services or were brought in by the police.
Median times to presentation were significantly higher for ambulance transports. This may be affected by public ambulances which are often used for inter-facility transport representing the second leg of transport to care. When splitting out public from private ambulances time to presentation was noted to be shortest for private ambulance services (1.71 h), followed by private car and “Other” (primarily police transport) both which had median times to presentation of 2 h (Table 1). The percentages of patients arriving within the first hour after trauma were identical for private ambulance and private vehicle (29.5 %). Among RTAs, there was a higher percentage of ambulance transports for trauma events involving a fatality at the scene (29.6 vs 6.9 %, P < 0.001, Fig. 2).
The method of transport used was not significantly associated with either time to presentation or distance with the exception of those patients who either presented on foot or by other (e.g., police) transport. Both of these groups represented patients who presented early and from locations nearby to UTH (< 30 km; Fig. 2).
KTS II score
Of 3425 patients arriving alive to the hospital, 2784 patients had both transport type and injury severity (KTS II) scores available. There were slight, though statistically significant, differences in the KTS II scores of patients by transport type (P = 0.0072, Table 2) with patients presenting by ambulance having marginally lower KTSII scores than those presenting by other means.
Of 3425 patients who arrived alive to the hospital, 1769 with documented transport method were admitted to the hospital. Of these, only 151 (8.6 % of 1769 admitted) had exact length of stay (LOS) data available (142 were discharged; 6 died; 3 left against medical advice).
Admission status
In addition, 408 patients were admitted for less than 24 h and 15 patients were still in the hospital at the end of inpatient data collection (30 days) with an unknown discharge date. This yields a total of 574 patients (32.6 %) with LOS data and methods of transport for analysis (Table 3). Comparison of the modes of transport, KTS score, and mortality for patients for whom LOS data were available and those where LOS data was absent demonstrated no significant differences, suggesting that excluding them from the LOS analysis does not introduce bias. While there was a trend toward higher rate of admission for patients transported by ambulance or private vehicle, the overall trend was not statistically significant (P = 0.1216) (Fig. 3).
Discussion
While there were no city-wide or national trauma registries in Zambia to estimate the percentage that presented to UTH, no other facilities existed in the region with advanced trauma care capacities at the time of this study. The number of patients presenting to private hospitals could not be estimated as part of this study.
These data demonstrate that only 6 % of trauma patients presented to UTH via public or private ambulance. This number only increases to 6.9 % when police and air transports were included. While a wide range of prehospital systems exist across Africa—each with different structures, capabilities, and transport times—this low rate of formal prehospital transport is consistent with other studies across the continent [16–26].
University Teaching Hospital is a regional and national referral hospital. During the period of the study, it also functioned as the main district hospital for trauma patients in Lusaka District. Most patients in the study resided locally with less than 2 % referred from outlying areas. This may explain the relatively rapid transport times noted in this study.
Furthermore, the relative speed of private and public transport to deliver injured patients to emergency care noted is likely indicative of the fact that this study was carried out in a densely populated urban capital where distances to the referral facility (UTH) are small. While these results are consistent with data from other urban settings across Africa [22–30], care must be taken not to extrapolate directly to other settings with wider catchment areas or rural areas where patients may be transported over long distances to district or regional hospitals.
The small difference in mean KTS II scores for patients compared by means of prehospital transport were statistically significant but unlikely to have clinical significance (8.11–8.5). Such patients are characterized by mild to moderate injuries with similar clinical outcomes. As such injury severity as prognosticated by the KTS II was not considered to vary with prehospital transport method. There was an increasing trend for ambulance use noted in the patients admitted for greater than 4 weeks duration.
There were 628 (18.3 %) of patients for whom a KTS II could not be calculated. These data were missing for primarily an inability to measure BP accurately on very small pediatric patients and morbidly obese patients due to lack of appropriately sized BP cuffs in the Casualty ward. This problem was noted at the first interim analysis and additional equipment was procured to ensure the ability to accurately measure BP and this complete the KTS II score.
Some patients were referred to UTH for either specialty care for significant injuries or simply for prolonged inpatient care, which may not have been available at smaller facilities. Without information on whether the final transport recorded was from the scene of a trauma or, as is commonly the case, from another health facility, makes interpretation of this finding limited.
Patients “Brought in Dead” typically represented a heterogeneous mix of patients who expired prior to arrival as well as those who expired during the first 24 h of their emergency evaluation and treatment in the Casualty Ward or the Surgical Admitting Ward. For data collected in this study, Brought in Dead refers only to patients that arrived at UTH having expired.
This study was not primarily focused on evaluating informal prehospital care, nor did we uniformly collect data on care provided by laypersons or police prior to arrival. Anecdotal reports from hospital staff demonstrated very little in the way of prehospital care provided by nonambulance personnel and any care provided took the form of bandaging of wounds and was not carried out as part of a structured management plan as may be the case when lay-responders are trained to conduct basic first aid interventions prior to hospital transport.
The government of Zambia has made recent investments to procure several hundred new ambulances and has begun to distribute this fleet of emergency vehicles across the country. While prehospital ambulance-based services may be necessary for transporting a subset of critically ill patients, these data suggest that significant improvements in prehospital care and transport may be achieved by targeting other factors (such as the public transport system) when developing a rational prehospital system. Studies in other highly urbanized settings in LMICs have demonstrated limited efficacy and coverage of the population using resource intensive prehospital systems based around centralized dispatch of expensive prehospital transport vehicles [3–5, 10, 11, 31–33].
The high percentage of injured patients who used public transportation to reach UTH for treatment (38 %) indicates the transport system may be an important target for intervention when developing a city-wide prehospital care plan. One improvement may be to have dedicated shuttles that transport patients from densely populated and/or low-income neighborhoods of the city directly to the local hospital without making standard stops like other buses. Such a simple intervention would provide more rapid transport of low-income patients to care—albeit on a scheduled rather than emergent basis. Planning for the efficient transport of patients who are unable to secure private transportation is an important part of any prehospital system.
Data have demonstrated that investments in basic and intermediate prehospital care, which leverage the human resources of lay providers and provide basic rapid transport to care, can be on par with the cost-effectiveness of more widely implemented health interventions, as measured by cost per DALY averted [5, 34]. High-tech, advanced life support prehospital systems may not achieve the same degree of cost-effectiveness [3, 32]. For low-income countries with limited resources, such systems may inappropriately tip the balance away from provision of basic service to a large percentage of the population toward advanced services being provided to a comparatively small number of individuals. In countries without well-established prehospital systems, such imbalance could hamper the ability of prehospital care to demonstrate real impact on the overall health of the population. Such limitations are real and point to the need to develop and evaluate models of prehospital transport and care that are most cost-effective in these settings.
While the majority of the world’s population lives in areas without access to formal emergency medical services, informal patterns of prehospital transport and care do in fact exist. By capitalizing on these existing patterns and augmenting communities’ own ability to stabilize sick and injured patients, prehospital systems can greatly leverage their scope and coverage of the populations they serve. For example, programs in several African countries have focused on training lay-responders, transport drivers or police personnel in basic first aid, hemorrhage control, splinting of injured extremities, and proper transfer of patients to prevent secondary injuries in transport, and have shown promise [3, 11, 12, 35, 36]. An integrated prehospital system in Zambia in the future might make effective use of a multilayered approach which incorporates training of members of local communities; first responders, such as public school teachers, police personnel, and transport drivers; as well as public and private ambulance transport to more effectively provide prehospital care to injured patients in Lusaka and throughout the country.
Conclusion
Injured patients in Lusaka present to the University Teaching Hospital by a variety of transport methods. The majority do not use ambulance transport of any kind. The majority of patients arrive expeditiously, despite the limited use of formal prehospital services. In the future, prehospital care planning in Lusaka could use an integrated, multipronged approach that incorporates community members, health professionals, and coordinates existing public transport services to best facilitate the rapid aid and transport of injured patients to care at local health facilities.
References
Haagsma JA, Graetz N, Bolliger I et al (2015) The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev 22:3–18
Chandran A, Hyder AA, Peek-Asa C (2010) The global burden of unintentional injuries and an agenda for progress. Epidemiol Rev 32:110–112
Mock C (2009) Strengthening prehospital trauma care in the absence of formal emergency medical services. World J Surg 33:2510–2511
Mock CN, Jurkovich GJ, nii-Amon-Kotei D et al (1998) Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. J Trauma 44:804–814
Kobusingye Olive C, Hyder Adnan A, Bishai David et al (2008) Emergency medical services (Chap 68). WHO, Washington
Lagarde E (2007) Road traffic injury is an escalating burden in Africa and deserves proportionate research efforts. PLoS Med 4:e170
Chen G (2010) Road traffic safety in African countries–status, trend, contributing factors, countermeasures and challenges. Int J Inj Control Saf Promot 17:247–255
Hsia R, Razzak J, Tsai AC et al (2010) Placing emergency care on the global agenda. Ann Emerg Med 56:142–149
Kobusingye OC, Hyder AA, Bishai D et al (2005) Emergency medical systems in low- and middle-income countries: recommendations for action. Bull World Health Organ 83:626–631
London JA, Mock CN, Quansah RE et al (2001) Priorities for improving hospital-based trauma care in an African city. J Trauma 51:747–753
Mock CN, Tiska M, Adu-Ampofo M et al (2002) Improvements in prehospital trauma care in an African country with no formal emergency medical services. J Trauma 53:90–97
Tiska MA, Adu-Ampofo M, Boakye G et al (2004) A model of prehospital trauma training for lay persons devised in Africa. Emerg Med J 21:237–239
Owor G, Kobusingye O (2001) Trauma registries as a tool for improved clinical assessment of trauma patients in an urban African hospital. East Cent Afr J Surg 6:57–63
MacLeod JBA, Kobusingye O, Frost C et al (2003) A comparison of the Kampala Trauma Score (KTS) with the Revised Trauma Score (RTS), Injury Severity Score (ISS) and the TRISS method in a Ugandan Trauma Registry. Eur J Trauma 29:392–398
Weeks SR, Juillard CJ, Monono ME et al (2012) Is the kampala trauma score an effective predictor of mortality in low-resource settings? A comparison of multiple trauma severity scores. J Surg Res 172:254
Ahidjo KA, Olayinka SA, Ayokunle O et al (2011) Prehospital transport of patients with spinal cord injury in Nigeria. J Spinal Cord Med 34:308–311
Bruce J, Schmollgruber S, Eales J et al (2003) Inury surveillance at a level I trauma centre in Johannesburg, South Africa. Health Sa Gesondheid 8:3–12
Chichom Mefire A, Etoundi Mballa GA, Azabji Kenfack M et al (2013) Hospital-based injury data from level III institution in Cameroon: retrospective analysis of the present registration system. Injury 44:139–143
Hodkinson PW (2009) Wallis LA Cross-sectional survey of patients presenting to a South African urban emergency centre. Emerg Med J 26:635–640
Hsia RY, Ozgediz D, Mutto M et al (2010) Epidemiology of injuries presenting to the national hospital in Kampala, Uganda: implications for research and policy. Int J Emerg Med 3:165–172
Kobusingye OC, Guwatudde D, Owor G et al (2002) Citywide trauma experience in Kampala, Uganda: a call for intervention. Inj Prev 8:133–136
Solagberu BA, Adekanye AO, Ofoegbu CPK et al (2002) Clinical spectrum of trauma at a university hospital in Nigeria. Eur J Trauma 28:365–369
Solagberu BA, Adekanye AO, Ofoegbu CPK et al (2003) Epidemiology of trauma deaths. West Afr J Med 22:177–181
Solagberu BA, Ofoegbu CKP, Abdur-Rahman LO et al (2009) Prehospital care in nigeria: a country without emergency medical services. Niger J Clin Pract 12:29–33
Oluwadiya KS, Olakulehin AO, Olatoke SA et al (2005) Prehospital care of the injured in South Western Nigeria: a hospital based study of four tertiary level hospitals in three states. Annu Proc Assoc Adv Automot Med 49:93–100
Hanewinckel R, Jongman HP, Wallis LA et al (2010) Emergency medicine in Paarl, South Africa: a cross-sectional descriptive study. Int J Emerg Med 3:143–150
Oluwadiya KS, Olakulehin AO, Olatoke SA et al (2005) Prehospital care of the injured in South Western Nigeria: a hospital based study of four tertiary level hospitals in three states. Annu Proc Assoc Adv Automot Med 49:93–100
Otieno T, Woodfield JC, Bird P et al (2004) Trauma in rural Kenya. Injury 35:1228–1233
Saidi HS (2003) Initial injury care in Nairobi, Kenya: a call for trauma care regionalisation. East Afr Med J 80:480–483
Solagberu BA, Ofoegbu CK, Nasir AA et al (2006) Motorcycle injuries in a developing country and the vulnerability of riders, passengers, and pedestrians. Inj Prev 12:266–268
Hauswald M, Yeoh E (1997) Designing a prehospital system for a developing country: estimated cost and benefits. Am J Emerg Med 15:600–603
Roy N, Murlidhar V, Chowdhury R et al (2010) Where there are no emergency medical services—prehospital care for the injured in Mumbai, India. Prehosp Disaster Med 25:145–151
Nielsen K, Mock C, Joshipura M et al (2012) Assessment of the status of prehospital care in 13 low- and middle-income countries. Prehosp Emerg Care 16:381–389
Adeloye D (2012) Prehospital trauma care systems: potential role toward reducing morbidities and mortalities from road traffic injuries in Nigeria. Prehosp Disaster Med 27:536–542
Jayaraman S, Mabweijano JR, Lipnick MS et al (2009) Current patterns of prehospital trauma care in Kampala, Uganda and the feasibility of a lay-first-responder training program. World J Surg 33:2512–2521
Jayaraman S, Mabweijano JR, Lipnick MS et al (2009) First things first: effectiveness and scalability of a basic prehospital trauma care program for lay first-responders in Kampala, Uganda. PLoS ONE 4:e6955
Acknowledgments
Data collection was funded by MercyFlyers, Zambia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest to report.
Ethical approval
Ethical approval for the study was obtained from the University of Zambia Research Ethics Committee and the Boston University Institutional Review Board. A waiver of informed consent for participating in the study was granted by both ethical review boards. Additional approval was obtained from the Zambian Ministry of Health.
Rights and permissions
About this article
Cite this article
Mowafi, H., Oranmore-Brown, R., Hopkins, K.L. et al. Analysis of Prehospital Transport Use for Trauma Patients in Lusaka, Zambia. World J Surg 40, 2868–2874 (2016). https://doi.org/10.1007/s00268-016-3629-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3629-4