Abstract
Background
The incidence of esophagogastric junction (EGJ) carcinoma is increasing, but its optimal surgical management remains controversial.
Methods
We retrospectively reviewed the database of 400 patients with Siewert type II EGJ carcinoma who were treated surgically at 7 institutions between March 1986 and October 2010. We examined the clinicopathological characteristics, prognostic factors, and risk factors associated with each recurrence pattern.
Results
The 5-year overall survival rate of all patients with Siewert type II EGJ carcinoma was 58.4 %. Multivariate analysis showed that T and N stages were independent prognostic factors. We also found that the incidence of lower mediastinal lymph node metastasis (17.7 %) and para-aortic lymph node metastasis (16.1 %) was relatively high. In addition, the para-aortic lymph nodes (N = 39, 9.8 %) were the most frequent node recurrence site, followed by the mediastinal lymph nodes (N = 23, 5.8 %). Lung recurrence was more common than was peritoneal recurrence. Considering each type of recurrence, multivariate analysis showed that the differentiated type was associated with a higher risk of lung recurrence than was the undifferentiated type, and N stage (pN2–3) and positive venous invasion were independent risk factors for liver recurrence.
Conclusions
This study is one of the largest retrospective studies to evaluate patients with Siewert type II EGJ carcinoma. Para-aortic and mediastinal lymph node metastasis and recurrence rates were relatively high. During the postoperative follow-up of patients with differentiated Siewert type II EGJ carcinoma, patients should be monitored for lung recurrence more closely than that for peritoneal recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of adenocarcinoma of the esophagogastric junction (EGJ) is increasing in developed countries [1–3]. The Siewert classification of EGJ adenocarcinoma has been widely accepted [4]. Siewert type II EGJ adenocarcinomas are located along the borderline between the mediastinum and abdomen; they can metastasize to both cavities. Thus, its optimal surgical management, including surgical approach (transthoracic or transhiatal), range of nodal dissection, and type of gastrectomy, remains controversial and has attracted considerable interest [5–9]. Siewert type II EGJ adenocarcinoma is currently treated using a multimodal approach involving surgery with a curative intent; however, outcomes remain unsatisfactory, even after curative resection [5–10].
Further information regarding prognostic factors and recurrence patterns of surgically treated patients with Siewert type II cancer is important for future strategic therapeutic planning. Oncological outcomes of Siewert type II EGJ adenocarcinoma have been reported by many researchers; however, the number of patients analyzed has not been adequate. Therefore, we aimed to clarify the clinicopathological characteristics, prognostic factors, and recurrence patterns of patients with Siewert type II EGJ carcinoma. In addition, we examined the risk factors for recurrence and each type of recurrence. This is the first report to examine the risk factors for each type of recurrence.
To the best of our knowledge, this study is one of the largest multicenter retrospective studies to evaluate patients with Siewert type II EGJ carcinoma.
Materials and methods
Patients
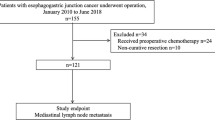
In this study, we retrospectively examined the medical records of 400 patients with Siewert type II EGJ carcinoma who underwent surgical treatment at 7 institutions between March 1986 and October 2010 in Japan. All tumors were histologically diagnosed as adenocarcinoma. Tumor staging was performed according to the International Union against Cancer tumor–node–metastasis (TNM) staging system [11]. Patients who underwent palliative (R2) surgery were excluded. This study (HIK-01) was approved by the Steering Committee of the Young Gastric Surgeons Research Group in Japan and the institutional review board of Keio University Hospital. We examined the overall survival (OS) of patients, distribution of lymph node metastasis, and recurrence patterns. Additionally, we examined the prognostic factors and risk factors associated with each recurrence pattern for 331 patients who underwent R0 surgery without preoperative chemotherapy.
Measurement of the distance from the EGJ to the distal end of the tumor
After resection, a fresh specimen was opened longitudinally, and lymph nodes were removed for pathological examination. The resected specimens were stretched and pinned to a board. The distance from the center of the tumor to the EGJ was measured and recorded by the surgeon. Siewert type II EGJ carcinoma was defined as a case where the center of the tumor was located 1 cm above and 2 cm below the EGJ. The EGJ was defined as the region where the tubular esophagus anatomically joins the stomach, based on macroscopic findings of the resected specimens.
Statistical analysis
OS was defined as the time from surgery to death from any cause. Survival curves were estimated using the Kaplan–Meier method. A Cox proportional hazards model was used for the univariate and multivariate survival analyses. The impact of clinicopathological factors on recurrence was investigated using univariate and multivariate logistic regression analyses. P values of <0.05 were considered statistically significant, and multivariate analysis was performed for variables whose P value was <0.10. SPSS Statistics software, version 22 (IBM Corp., Armonk, NY, USA) was used for all statistical analyses.
Results
Clinical parameters and pathological findings
The clinical parameters and pathological findings of the 400 patients with Siewert type II EGJ carcinoma are shown in Table 1. There was a predominance of male patients (79.0 %) in our study. The median tumor length was 50 mm, and the median esophageal invasion length was 7.5 mm. The transhiatal approach was used more often (62.7 %) than the right thoracotomy (10.0 %) and left thoracoabdominal approaches (27.3 %). Of the 370 patients who underwent lower esophagectomy, the transhiatal approach was used in 251 patients (67.8 %) and the transthoracic approach in 119 patients (32.2 %).
Survival rate
The 5-year OS rate of all patients with Siewert Type II EGJ adenocarcinoma in this study was 58.4 %. The median follow-up duration was 5.2 years (range, 1.0–20.6 years) for patients who survived.
We evaluated the 5-year OS rate according to tumor depth, N stage, TNM stage, and residual tumor stage (Fig. 1a–d). Patients with pT1 and pT2 carcinoma showed good outcomes (5-year OS rate of 90.6 and 81.3 %, respectively). The 5-year OS rate of patients with pT3 and pT4 carcinoma was low at 46.6 and 41.8 %, respectively. The 5-year OS rate for pN0 and pN1 patients was 77.4 and 73.2 %, respectively, and it decreased to 54.7 and 22.0 % for pN2 and pN3 patients, respectively. The 5-year OS rate according to the stage was as follows: stage I, 87.4 %; stage II, 70.9 %; stage III, 51.4 %; and stage IV, 12.6 %. The 5-year OS rate for patients who underwent R0 resection was 60.8 %, compared with the rate of 25.9 % for those who underwent R1 resection.
a Overall survival curves in patients with Siewert type II esophagogastric junction carcinoma according to tumor depth stage. b Overall survival curves in patients with Siewert type II esophagogastric junction carcinoma according to N stage. c Overall survival curves in patients with Siewert type II esophagogastric junction carcinoma according to TNM stage. d Overall survival curves in patients with Siewert type II esophagogastric junction carcinoma according to residual tumor stage
The results of the univariate and multivariate Cox regression analyses for OS are shown in Table 2. Univariate analysis showed that T and N stages, lymphatic invasion, venous invasion, >30 mm gastric invasion, postoperative chemotherapy use, and tumor length >50 mm were significant predictors of survival. Multivariate analysis showed that T and N stages were independent prognostic factors. The hazard ratio for early death was 3.120 (95 % confidence interval 1.761–5.527) for pT3–T4 versus pT1–T2 and 2.013 (95 % confidence interval 1.347–3.006) for pN2–N3 versus pN0–N1.
Distribution of lymph node metastasis
The distribution of lymph node metastases is shown in Table 3. Most lymph node metastases were located in the lesser curvature area and right paracardiac area. Lower mediastinal lymph node metastasis was observed in 37 of 208 patients (17.7 %) who underwent lower mediastinal lymph node dissection. Sixty-seven of 208 patients (32.2 %) underwent lower mediastinal dissection by the transhiatal approach. Para-aortic lymph node metastasis was observed in 22 of 136 patients (16.1 %) who underwent para-aortic lymph node dissection.
Recurrence patterns
The initial recurrence patterns are shown in Table 4. One hundred fifty-one (37.7 %) of the 400 patients experienced relapse, and 207 recurrence sites were considered to be the initial recurrence sites. Sixty-three (15.8 %) of the 400 patients showed lymph node recurrences in ≥1 region. The para-aortic lymph nodes (N = 39, 9.8 %) were the most frequent lymph node recurrence site, followed by the mediastinal lymph nodes (N = 23, 5.8 %).
With regard to hematogenous recurrence, 44 patients experienced liver recurrence and 29 patients experienced lung recurrence. Peritoneal recurrence was observed in 27 patients.
Risk factors associated with each recurrence pattern
We examined the risk factors for recurrence and each type of recurrence (para-aortic lymph node, mediastinal lymph node, lung, liver, and peritoneal recurrence) by logistic regression analysis. The results of univariate and multivariate logistic regression analyses are shown in Table 5. With regard to each type of recurrence, multivariate analysis showed that T stage (pT3–4) was an independent risk factor for para-aortic lymph node and lung recurrence. N stage (pN2–3) and positive venous invasion were independent risk factors for liver recurrence. Being less than 65 years old was independent risk factor for mediastinal recurrence. The undifferentiated type had at lower risk of lung recurrence than did the differentiated type.
Discussion
We retrospectively examined the clinicopathological characteristics, prognostic factors, recurrence patterns, and risk factors associated with each recurrence pattern of Siewert type II EGJ carcinoma. This study is one of the largest multicenter, retrospective studies to evaluate patients with Siewert type II EGJ carcinoma and is the first report to examine the risk factors for each type of recurrence.
We examined prognostic factors in patients who underwent R0 surgery without preoperative chemotherapy. Multivariate analysis showed that pT and pN stages were independent prognostic factors. These results are also in line with those reported previously [5, 10, 12, 13]. With regard to gastric cancer, pT and pN stages were also reported as independent prognostic factors by another group [14]. We found that the para-aortic lymph nodes (N = 39, 9.8 %) were the most frequent lymph node recurrence site, followed by the mediastinal lymph nodes (N = 23, 5.8 %). We also found that the incidence of lower mediastinal lymph node metastasis (17.7 %) and para-aortic lymph node metastasis (16.1 %) was relatively high.
According to the results of a multicenter randomized controlled trial in Japan (Japan Clinical Oncology Group [JCOG] 9501), para-aortic nodal dissection is no longer performed for Siewert type II EGJ carcinoma in several institutions [15]. In this study, only 137 patients (33.1 %) underwent para-aortic lymph node dissection. However, the target of JCOG 9501 was gastric cancer and not EGJ carcinoma. Anatomically, EGJ is proximal to the para-aortic region, which is why lymph node metastasis and recurrence are often observed. Thus, the necessity of para-aortic nodal dissection for Siewert type II EGJ carcinoma remains controversial. In addition, the benefit of mediastinal lymph node dissection remains controversial. Omloo et al. [8] reported that patients with adenocarcinoma of the mid/distal esophagus and 1–8 metastatic lymph nodes appear to benefit from extended transthoracic esophagectomy. On the other hand, Sasako et al. reported that the left thoracoabdominal approach does not improve survival rates after applying the transhiatal approach and that it can lead to higher morbidity rates in patients with Siewert type II or III EGJ carcinomas with esophageal invasion of ≤3 cm [9]. As far as we know, prospective studies have not been conducted to clarify the benefit of para-aortic and mediastinal lymph node dissection in patients with Siewert type II EGJ carcinomas. From our results and those of previous reports, a prospective study (UMIN000013205) is ongoing to determine the true incidence and benefit of para-aortic and mediastinal lymph node dissection among such patients.
In this study, we examined the recurrence patterns and risk factors for each recurrence pattern. These results highlight the recurrence types that should be closely monitored during follow-up. Some authors reported the recurrence patterns of a small number of patients with Siewert type II EGJ carcinoma [12, 13, 16]. However, they could not examine the risk factors for each recurrence pattern owing to the small number of patients. We found that lung recurrence was more common than was peritoneal recurrence. However, in gastric cancer, lung recurrence is rare, and peritoneal recurrence is the most frequent recurrence pattern [17, 18]. Siewert type II EGJ carcinoma is located along the borderline between the abdominal and thoracic cavities, with venous return to the azygos and portal venous system. Thus, Siewert type II EGJ carcinoma is associated with a lower risk of peritoneal recurrence and a higher risk of lung recurrence than is gastric cancer. Interestingly, patients with differentiated adenocarcinoma were at a significantly higher risk of lung recurrence as an initial recurrence than were patients with the undifferentiated type. Differentiated-type gastric cancer is known to have a higher risk of hematogenous recurrence than does the undifferentiated type of gastric cancer [17, 18]. N stage (pN2–3) and positive venous invasion were independent risk factors for liver recurrence.
This study had some limitations. First, this was a retrospective study. Second, preoperative chemotherapy was also chosen according to the preference of the surgeons in this study. Third, the surgical strategy was determined by the surgeon; thus, various surgical procedures were included in this study.
This study is one of the largest retrospective studies aimed at evaluating patients with Siewert type II EGJ carcinoma. We found that the N stage was an independent prognostic factor. Moreover, we found that para-aortic and mediastinal lymph node metastasis and recurrence rates were relatively high. With regard to each type of recurrence, the differentiated type was an independent risk factor for lung recurrence, and N stage (pN2–3) and positive venous invasion were independent risk factors for liver recurrence.
References
Blot WJ, Devesa SS, Kneller RW et al (1991) Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA 265:1287–1289
Devesa SS, Blot WJ, Fraumeni JF Jr (1998) Changing patterns in the incidence of esophageal and gastric carcinoma in the United States. Cancer 83:2049–2053
Hansen S, Wiig JN, Giercksky KE et al (1997) Esophageal and gastric carcinoma in Norway 1958–1992: incidence time trend variability according to morphological subtypes and organ subsites. Int J Cancer 71:340–344
Siewert JR, Stein HJ (1998) Classification of adenocarcinoma of the oesophagogastric junction. Br J Surg 85:1457–1459
Yamashita H, Katai H, Morita S et al (2011) Optimal extent of lymph node dissection for Siewert type II esophagogastric junction carcinoma. Ann Surg 254:274–280
Hosokawa Y, Kinoshita T, Konishi M et al (2012) Clinicopathological features and prognostic factors of adenocarcinoma of the esophagogastric junction according to Siewert classification: experiences at a single institution in Japan. Ann Surg Oncol 19:677–683
Ito H, Inoue H, Odaka N et al (2013) Clinicopathological characteristics and optimal management for esophagogastric junctional cancer; a single center retrospective cohort study. J Exp Clin Cancer Res 32:2
Omloo JM, Lagarde SM, Hulscher JB et al (2007) Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the mid/distal esophagus: five-year survival of a randomized clinical trial. Ann Surg 246:992–1000
Sasako M, Sano T, Yamamoto S et al (2006) Left thoracoabdominal approach versus abdominal-transhiatal approach for gastric cancer of the cardia or subcardia: a randomised controlled trial. Lancet Oncol 7:644–651
Siewert JR, Feith M, Werner M et al (2000) Adenocarcinoma of the esophagogastric junction: results of surgical therapy based on anatomical/topographic classification in 1,002 consecutive patients. Ann Surg 232:353–361
Sobin LH, Gospodarowicz MK, Wittekind CH (2009) TNM classification of malignant tumours, 7th edn. Wiley-Blackwell, New York
Waymann J, Bennett MK, Raimes SA et al (2002) The pattern of recurrence of adenocarcinoma of the oesophago-gastric junction. Br J Cancer 86:1223–1229
Hulscher JB, van Sandick JW, Tijssen JG et al (2000) The recurrence pattern of esophageal carcinoma after transhiatal resection. J Am Coll Surg 191:143–148
Zhang J, Niu Z, Zhou Y, Cao S (2013) A comparison between the seventh and sixth editions of the American Joint Committee on Cancer/International Union Against classification of gastric cancer. Ann Surg 257:81–86
Sasako M, Sano T, Yamamoto S et al (2008) D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med 359:453–462
HosokawaY Kinoshita T, Konishi M et al (2014) Recurrence patterns of esophagogastric junction adenocarcinoma according to Siewert’s classification after radical resection. Anticancer Res 34:4391–4397
Katai H, Maruyama K, Sasako M et al (1994) Mode of recurrence after Gastric cancer Surgery. Dig Surg 11:99–103
Maehara Y, Hasuda S, Koga T et al (2000) Postoperative outcome and sites of recurrence in patients following curative resection of gastric cancer. Br J Surg 87:353–357
Acknowledgments
We thank Prof. Yuichiro Doki and Prof. Yuko Kitagawa for supervising this study. This study received no grant support.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Tatsuo Matsuda, Yukinori Kurokawa, and Takaki Yoshikawa have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Matsuda, T., Kurokawa, Y., Yoshikawa, T. et al. Clinicopathological Characteristics and Prognostic Factors of Patients with Siewert Type II Esophagogastric Junction Carcinoma: A Retrospective Multicenter Study. World J Surg 40, 1672–1679 (2016). https://doi.org/10.1007/s00268-016-3451-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3451-z