Abstract
Background
Familial papillary thyroid carcinoma (familial PTC) is well known to present with aggressiveness; however, the characteristics and the prognostic outcomes of familial papillary thyroid microcarcinoma (familial micro-PTC) are not well established. The overall aim of this study was to analyze the clinicopathological outcomes of familial micro-PTC.
Methods
Between 1996 and 2006, 2071 patients underwent thyroid surgery for papillary thyroid carcinoma. The clinicopathological outcomes for familial PTC and sporadic PTC were compared, and familial micro-PTC data were sub-analyzed.
Results
There were significant differences in multifocality, bilaterality, extent of surgery, and recurrence between familial PTC and sporadic PTC (p < 0.05). There was no significant difference in the number of affected family members in the familial PTC group. In patients with familial micro-PTC, less aggressiveness was noted in multifocality, extrathyroidal invasion, tumor stage at time of initial surgery, central lymph node metastasis, and recurrence than in those with familial PTC tumors >1 cm in diameter (p < 0.05). The multivariate analysis including recurrence showed no significant difference between familial micro-PTC patients and sporadic micro-PTC patients.
Conclusion
When familial PTC was compared with sporadic PTC, our results support the recommendation for more invasive familial PTC surgery. However, familial micro-PTC outcomes differed from familial PTC tumors >1.0 cm in diameter. It was similar to sporadic micro-PTC, illustrating that familial micro-PTC is less aggressive and that a less invasive surgical treatment could be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid carcinoma is one of the representative malignancy in women with more than 90 % diagnosed as differentiated thyroid carcinomas, fortunately having a favorable prognosis [1]. Detection of thyroid carcinoma has increased recently with advancements in health screening [2] such as thyroid ultrasound (US) and fine-needle aspiration biopsy (FNAB). Both techniques have permitted most thyroid carcinomas to be detected at an early stage, thus offering favorable outcomes after treatment [3, 4]. Screening examinations and thorough history taking have also contributed to the early detection of common sporadic papillary thyroid carcinoma (sporadic PTC), as well as to the differentiation of these carcinomas from familial PTC [5].
The first familial non-medullary thyroid carcinoma (familial non-MTC), reported in 1955 by Robinson and Orr [6], was classified as a non-medullary thyroid carcinoma with no history of other neoplasm in two or more first-degree relatives, including the index patient [7]. Although many pathologic and genetic studies have been developed in sub-types of thyroid carcinomas, a prognosis related gene for familial non-MTC is yet to be found [8, 9]. While the majority of familial non-MTCs are familial PTCs, familial non-MTCs are more aggressive, associate with poor prognoses, and require more invasive surgery than sporadic PTCs [10–14]. However, several papers have reported that familial PTCs do not tend to have worse prognosis and familial PTC therapeutic strategy does not have to differ from sporadic PTCs [15–17].
Surgery for sporadic papillary thyroid microcarcinoma (sporadic micro-PTC) is known to be less invasive than for sporadic PTC, where tumor size is an independent prognostic factor [18, 19]. In contrast, the extent of surgery for familial micro-PTC compared to familial PTC still remains controversial [20]. Since sporadic micro-PTC is less aggressive than sporadic PTC, we evaluated the characteristics and prognostic outcomes of familial micro-PTC compared to familial PTC and sporadic micro-PTC.
Materials and methods
Study population
This retrospective study analyzed records of 2733 patients who underwent thyroidectomy for PTC between 1996 and 2006 by a single experienced surgeon at the Asan Medical Center (IRB 2013-0291). Of 2733 patient records, 2071 contained complete data profiles. These 2071 patients were classified as presenting; PTC with no history of familial neoplasms, PTC with a family history of two first-degree relatives, or PTC with a family history of three or more first-degree relatives. Carcinoma was confirmed in all patients by histopathology. Patients underwent total thyroidectomy with ipsilateral for unilateral carcinoma, total thyroidectomy with bilateral central lymph node dissection for bilateral carcinoma, or hemithyroidectomy with ipsilateral central lymph node dissection according to the disease status.
Hemithyroidectomy patients received thyroid hormone to suppress thyroid-stimulating hormone (TSH) below the normal range, whereas total thyroidectomy patients received thyroid hormone to maintain the thyroid function and TSH at low range (<0.04 μU/ml). Patients were followed postoperatively by routine examinations every 3–6 months within a year after surgery and yearly thereafter. Thyroid function tests and thyroid US were performed on hemithyroidectomy patients, and a stimulated thyroglobulin level examination with radioiodine ablation was additionally performed on total thyroidectomy patients to evaluate disease recurrence. When an indeterminate nodule was found by US, the FNAB was performed. Disease recurrence was confirmed by histopathology.
Statistical analysis
Clinicopathological characteristics and prognostic outcomes such as age, gender, tumor size, multifocality, bilaterality, extrathyroidal invasion, tumor stage at time of initial surgery, extent of surgery, central lymph node metastasis, recurrence, and recurrence-free survival (RFS) were obtained. Comparative analysis was performed on familial PTC and sporadic PTC groups. For the familial PTC group, the outcomes were analyzed on the basis of affected family members with first-degree relatives. In addition, familial micro-PTC patients having a tumor size ≤1.0 cm in diameter were analyzed separately and were compared with familial PTC having a tumor size >1.0 cm in diameter, and sporadic micro-PTC outcomes.
Statistical analysis was performed with SPSS (version 16.0; SPSS Inc., Chicago, IL, USA). The χ 2 test was used for categorical variables, and the two-tailed t test was used for continuous variables. The Kaplan–Meier method was used. A p value <0.05 was considered statistically significant.
Results
General
Out of 2071 patients, there were 1833 (88.5 %) sporadic PTC and 238 (11.5 %) familial PTC patients. During initial diagnosis, 28 (11.8 %) familial PTC patients had lateral neck node metastasis, and modified radical neck dissection was performed. Among 238 familial PTC patients, 199 (83.6 %) and 39 (16.4 %) had a history of PTC in two and three or more first-degree relatives, respectively. Family histories of PTC were obtained prior to thyroid surgery in 113 (47.5 %) patients. The remaining 125 (52.5 %) patients were confirmed during a follow-up visit or by telephone communication. The overall postoperative follow-up duration was 118.0 ± 42.9 months.
Analysis of familial papillary thyroid carcinoma patients and sporadic papillary thyroid carcinoma patients
Table 1 compares clinicopathological characteristics and prognostic outcomes between familial PTC and sporadic PTC groups. There were no significant differences in age, gender, tumor size, extrathyroidal invasion, tumor stage at time of initial surgery, and central lymph node metastasis between groups (p > 0.05); however, there were differences in multifocality, bilaterality, and extent of surgery (p < 0.05). Recurrence rates were 9.7 and 6 % in familial PTC and sporadic PTC patients, respectively (p = 0.049). Under the multivariable cox model, familial type was the only variable affecting the recurrence showing higher hazard risk (1.623) than sporadic type (p = 0.024).
Analysis of familial papillary thyroid carcinoma patients according to the number of affected family members
Two hundred and thirty-eight familial PTC patients were grouped on the basis of the number of first-degree relatives with PTC. One hundred and ninety-nine (83.6 %) patients had two first-degree relatives with PTC, and 39 (16.4 %) patients had three or more first-degree relatives with PTC. There were no significant differences in age, gender, tumor size, multifocality, bilaterality, extrathyroidal invasion, tumor stage at time of initial surgery, extent of surgery, central lymph node metastasis, and recurrence (Table 2). The RFS for patients with two and three or more affected family members at 10 years post-operation were 82 and 80.8 %, respectively, showing no difference in the overall RFS (p > 0.05).
Analysis of familial papillary thyroid microcarcinoma patients
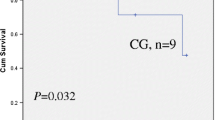
The familial PTC patients were sub-grouped on the basis of tumor size (≤1.0 cm in diameter or >1.0 cm), and 94 (39.5 %) patients had familial micro-PTC. Three (3.2 %) of these patients had lateral neck node metastasis, and modified radical neck dissection was performed. The overall postoperative follow-up duration was 91.2 ± 28.3 months. There were no differences in age and bilaterality (Table 3); however, there were significant differences in gender, multifocality, extrathyroidal invasion, tumor stage at time of initial surgery, extent of surgery, and central lymph node metastasis (p < 0.05). The recurrence rate was much higher in familial PTC with tumor size >1.0 cm having 14.6 % compared to 2.1 % in familial micro-PTC patients. However, RFS rate for familial micro-PTC and familial PTC patients with a tumor size >1 cm in diameter at 10 years post-operation were 84.7 and 78.7 %, respectively, and there was no difference in the overall RFS (p > 0.05) (Fig. 1).
Analysis of familial papillary thyroid microcarcinoma patients and sporadic papillary thyroid microcarcinoma patients
The percentage of familial micro-PTC was 39.5 % (94 of 238) among familial PTC patients, and sporadic micro-PTC patients were 26.8 % (462/1833) among sporadic PTC patients. The multivariate and univariate analysis showed no significant differences (p > 0.05). The recurrence rates were 2.1 % (2 of 94) in familial micro-PTC and 2.6 % (12/462) in sporadic micro-PTC showing no difference in RFS (Fig. 2).
Discussion
In our study, familial PTC was more aggressive than sporadic PTC with regard to multifocality and bilaterality, and surgery for familial PTC was more invasive. There was also a difference in the familial PTC recurrence rate, which was statistically higher than that of the sporadic PTC group (p < 0.05). Our results on the aggressiveness of FNMTC and on the recommendation for total thyroidectomy correlated with previously published results [10, 13, 21]. While some studies have supported therapeutic or prophylactic lateral functional neck dissection for familial PTC [11, 12], the extent of surgery and quality of life after the surgery should be carefully considered given the low recurrence rate of PTC.
On the other hand, recent studies have reported no significant differences in multifocality, surgical management, recurrence, and postoperative prognosis between sporadic and familial PTC patients [15, 16]. Maxwell et al. [15] reported that familial PTC patients do not have a worse prognosis than sporadic PTC. For patients with familial PTC, Ito et al. [16] recommended either total thyroidectomy or a therapeutic strategy similar to that of sporadic PTC. Even though familial PTC is aggressive, associates with a poor prognosis, and involves invasive surgery (i.e., total thyroidectomy), life expectancy and survival rates of those with familial PTC were not affected [14]. While Uchino et al. [11] recommended total thyroidectomy with modified radical neck dissection for FNMTC patients, they also reported no difference in prognostic outcome between FNMTC and sporadic PTC.
In previous reports, the number of affected family members was taken into account when studying familial PTC patients where family members were separated on the basis of family history (i.e., a family history of either two or three first-degree relatives with familial PTC). Alsanea et al. [10] reported that the number of affected family members correlated with FNMTC aggressiveness and poor outcome. Triponez et al. [14] recommended more invasive surgery for patients with three or more first-degree relatives, whereas another group reported worse outcomes for second generation patients than for first generation patients [22]; however, this trend was not observed in our data. There were no significant differences in any clinicopathological parameters, including recurrence and RFS rates. Instead, we showed that the familiality, and not the number of affected family members, to be a risk factor for PTC patients.
To address the debate on which surgical approach is best for a patient with familial PTC, tumors were analyzed on the basis of size (≤1.0 or >1.0 cm in diameter) and grouped as either familial micro-PTC or familial PTC (tumor size >1.0 cm in diameter). There were significant differences in multifocality, extrathyroidal invasion, tumor stage at time of initial surgery, central lymph node metastasis, and recurrence in familial micro-PTC patients compared with those with familial PTC tumors >1 cm in diameter. Sixty-five (69.1 %) patients received surgery more invasive than total thyroidectomy, and 29 (30.9 %) patients received hemithyroidectomy. Lupoli et al. [20] described the clinical and prognostic characteristics of familial micro-PTC patients and recommended radical treatment since familial micro-PTC displays an unfavorable outcome. However, there was no correlation between recurrence and the type of surgery performed since three out of seven familial micro-PTC patients had local or distant metastases. Near-total or total thyroidectomy was performed on all three patients in their study. We showed significant differences in multifocality, extrathyroidal invasion, tumor stage at time of initial surgery, central lymph node metastasis, and recurrence in familial micro-PTC patients, illustrating that familial micro-PTC is less aggressive than familial PTC.
In addition, since sporadic micro-PTC is well known to have more favorable prognostic outcomes than sporadic PTC, we compared between familial micro-PTC and sporadic micro-PTC. In results, we could not find any risk factors affecting the prognosis of familial micro-PTC leading to higher recurrence rate or poor prognosis. These could suggest that the familial micro-PTC (excluding the familial PTC with tumor size >1.0 cm) has similar prognosis compared to sporadic micro-PTC. However, since there were only a few number of recurrence in papillary microcarcinoma patient groups in our study duration, we were to assume that recurrence rate are alike for now, but could change along further follow-up.
We believe that more invasive surgery (i.e., total thyroidectomy) is needed for familial PTC because there were differences in recurrence rate between familial PTC and sporadic PTC, although recurrence rates were below 10 % for both types of carcinoma. For familial PTC, the number of affected family members was not a higher risk factor. And, in familial micro-PTC patients the overall characteristics and prognostic outcomes were favorable than the familial PTC with very low recurrence rate and similar to that of sporadic micro-PTC.
While the incidence of familial PTC at our institution was higher than that of other studies [7, 11], data collected from a single large institution might not represent the true consensus in disease incidence. It is also possible that familial PTC patients having two affected family members might not represent the actual family history and in portion, the incidentally found sporadic cases within the family members could be included, an increasing incidence condition under the affect of health care screening system in Korea [9]. For this reason, more invasive surgery such as total thyroidectomy should be avoided for familial micro-PTC patients since sporadic cases of PTMC might be included.
To conclude, our results illustrate that less invasive surgery (i.e., hemithyroidectomy with ipsilateral central lymph node dissection) could be suggested for familial micro-PTC as favorable postoperative outcomes are expected with less aggressive treatment approach.
References
Sherman SI (2003) Thyroid carcinoma. Lancet 361:501–511
Grodski S, Delbridge L (2009) An update on papillary microcarcinoma. Curr Opin Oncol 21:1–4
Grodski S, Brown T, Sidhu S et al (2008) Increasing incidence of thyroid cancer is due to increased pathologic detection. Surgery 144:1038–1043 discussion 1043
Schlumberger MJ (1998) Papillary and follicular thyroid carcinoma. N Engl J Med 338:297–306
Uchino S, Noguchi S, Yamashita H et al (2004) Detection of asymptomatic differentiated thyroid carcinoma by neck ultrasonographic screening for familial nonmedullary thyroid carcinoma. World J Surg 28:1099–1102. doi:10.1007/s00268-004-7676-x
Robinson DW DW, Orr TG (1955) Carcinoma of the thyroid and other diseases of the thyroid in identical twins. AMA Arch Surg 70:923–928
Grossman RF, Tu SH, Duh QY et al (1995) Familial nonmedullary thyroid cancer. An emerging entity that warrants aggressive treatment. Arch Surg 130:892–897 discussion 898–899
DeLellis RA (2006) Pathology and genetics of thyroid carcinoma. J Surg Oncol 94:662–669
Dotto J, Nose V (2008) Familial thyroid carcinoma: a diagnostic algorithm. Adv Anat Pathol 15:332–349
Alsanea O, Wada N, Ain K et al (2000) Is familial non-medullary thyroid carcinoma more aggressive than sporadic thyroid cancer? A multicenter series. Surgery 128:1043–1050 discussion 1050–1041
Uchino S, Noguchi S, Kawamoto H et al (2002) Familial nonmedullary thyroid carcinoma characterized by multifocality and a high recurrence rate in a large study population. World J Surg 26:897–902. doi:10.1007/s00268-002-6615-y
Sturgeon C, Clark OH (2005) Familial nonmedullary thyroid cancer. Thyroid 15:588–593
Sippel RS, Caron NR NR (2007) An evidence-based approach to familial nonmedullary thyroid cancer: screening, clinical management, and follow-up. World J Surg 31:924–933. doi:10.1007/s00268-006-0847-1
Triponez F, Wong M, Sturgeon C et al (2006) Does familial non-medullary thyroid cancer adversely affect survival? World J Surg 30:787–793. doi:10.1007/s00268-005-0398-x
Maxwell EL, Hall FT, Freeman JL (2004) Familial non-medullary thyroid cancer: a matched-case control study. Laryngoscope 114:2182–2186
Ito Y, Kakudo K, Hirokawa M et al (2009) Biological behavior and prognosis of familial papillary thyroid carcinoma. Surgery 145:100–105
Moses W, Weng J, Kebebew E (2011) Prevalence, clinicopathologic features, and somatic genetic mutation profile in familial versus sporadic nonmedullary thyroid cancer. Thyroid 21:367–371
Besic N, Pilko G, Petric R et al (2008) Papillary thyroid microcarcinoma: prognostic factors and treatment. J Surg Oncol 97:221–225
Bernet V (2010) Approach to the patient with incidental papillary microcarcinoma. J Clin Endocrinol Metab 95:3586–3592
Lupoli G, Vitale G, Caraglia M et al (1999) Familial papillary thyroid microcarcinoma: a new clinical entity. Lancet 353:637–639
Alsanea O, Clark OH (2001) Familial thyroid cancer. Curr Opin Oncol 13:44–51
Capezzone M, Marchisotta S, Cantara S et al (2008) Familial non-medullary thyroid carcinoma displays the features of clinical anticipation suggestive of a distinct biological entity. Endocr Relat Cancer 15:1075–1081
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sung, TY., Lee, Ym., Yoon, J.H. et al. Surgical Management of Familial Papillary Thyroid Microcarcinoma: A Single Institution Study of 94 Cases. World J Surg 39, 1930–1935 (2015). https://doi.org/10.1007/s00268-015-3064-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3064-y