Abstract
Background
This study aimed to document thyroidectomy outcomes in the surgical endocrine unit, Mulago Hospital, Kampala, Uganda. The burden of global surgical disease is currently receiving much attention, especially in countries experiencing epidemiological transition. There is a paucity of publications on surgical outcomes from Sub-Saharan Africa. International thyroid guidelines from high-income countries do not factor in the logistical challenges or the advanced pathology faced by the surgeon in resource-limited settings.
Methods
This was a prospective cohort study in 2013. Eight peri-operative variables of poor outcome were analysed statistically against six outcomes variables. Data was collected from 0 to 6 months post-operatively.
Results
Forty-two thyroidectomies were performed over a 3-month period (female = 38). Intraoperative events recorded included rebleeding = 10 %, infection = 0 %, transient voice symptoms = 30 %, transient hypocalcaemia = 12.5 %, recurrent laryngeal nerve (RLN) paralysis = 7.5 % and permanent hypocalcaemia = 15 %. There was a weak powered association between RLN paralysis and total thyroidectomy and smaller thyroid size. There were associations between large thyroid size and both permanent hypocalcaemia and rebleeding. Younger patients showed statistically more transient voice changes compared to older patients. Older patients were statistically more likely to develop rebleeding. Shorter operative duration was associated with transient voice change, permanent hypocalcaemia and rebleeding. Airway difficulties and transient hypocalcaemia were statistically significant in prolonged procedures.
Conclusions
Whilst the thyroidectomy outcomes are not equal to international standards, an acceptable standard is achievable in this resource-limited setting. Poor outcomes are multifactorial but extremes of thyroid size, extremes of operation duration and total thyroidectomies all have statistically poorer outcomes in this setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
We report the first prospective hospital-based series of thyroidectomies in Uganda. These are original and rare data on outcomes in Sub-Saharan Africa. Mulago Hospital is the tertiary referral hospital in Uganda (Fig. 1). The annual per capita income in Uganda is $420, which places it in the low-income category as defined by the World Bank [1]. Compared with developed countries, thyroid disease requiring surgery is a major burden in Sub-Saharan Africa. The WHO estimates that 43 % of the African population have insufficient iodine intake [2]. Despite the Ugandan government’s introduction of a universal policy of salt iodization in 1993, iodine deficiency is still above 36 %, constituting a severe public health problem [3]. Goitrogens also add to the problem. These include thiocyanates, which are found in poorly detoxified cassava, a food staple that is commonly eaten as a source of carbohydrate [4]. Selenium deficiency has also been reported as a contributory factor in the occurrence of endemic goitre in Africa [5]. Papillary cancer is the most common thyroid cancer in Uganda. This was also found in other areas of Africa [6].
Sub-Saharan Africa accounts for 24 % of the global disease burden but has only 3 % of the global health workforce [7]. In Uganda a shortage of trained health workers [8, 9] is one of the barriers to accessing healthcare [10]. This often results in surgical task shifting and less qualified surgeons performing specialised surgery. This paper’s overview of outcomes in Mulago’s surgical endocrine unit is a valuable reference for the non-specialist African surgeon. International thyroid guidelines do not allow for the non-specialist surgeon nor the advanced thyroid pathology that presents in resource-limited settings. The inability of patients to afford pre-operative investigations, to adhere to long-term medication regimens or to return for post-operative follow-up also presents logistical challenges not seen in the developed world.
In 2012, there were 104 thyroidectomies performed through the publicly funded system in Mulago Hospital. This study aimed to recruit a third of this number in order to produce a representative overview of surgical outcomes. The prospective nature of this study reduced recall bias. This was imperative in this setting where retrospective documentation was not always accurate, reliable or available.
Materials and methods
All thyroidectomy patients admitted to the endocrine ward over a 3-month period in 2013 were recruited to the study on an intention to treat basis. All patients gave informed consent. Eight peri-operative variables of poor outcome (Table 1) were identified through a PubMed literature search and using published British and American guidelines [11–13]. Post-operatively, each patient was examined and interviewed at day 1 (early), day 7 (intermediate) and 6 months (late). Six outcome variables were identified. The first three outcomes were considered early/intermediate and the last three late. All permutations of the eight peri-operative variables were analysed statistically against the outcome variables for significance using Fisher’s exact test and Student’s t test as applicable. Multivariate analysis was not performed as insufficient number of variables approached the threshold for significance. All analysis was performed using Graphpad Prism version 6 (Graphpad Software Inc.) p < 0.05. The sample size was small due to the limited time period of the principal researcher in Uganda and the need to collect all data prospectively. All patients were followed up by mobile phone; however, due to the patient remoteness and socioeconomic constraints, this was a challenge. Over 95 % of patients had serum thyroid function, chest X-ray, ultrasound, indirect laryngoscopy (IDL) and fine needle aspiration cytology (FNAC) pre-operatively. FNAC was the most common test omitted. Only one patient had advanced diagnostic imaging, a computerized tomographic (CT) which showed marked tracheal compression. Only one patient had had previous thyroid surgery. The vast majority of the patient cohort was ASA 1. Hypertension was the most common comorbidity. Each patient was interviewed pre-operatively by a researcher and their demographics and their consent to participate in the study obtained. Each individual operation was observed and the critical steps documented. These included exposure of recurrent laryngeal nerve(s) (RLN), exposure and protection of parathyroid glands, ligation of superior thyroid vessels and inferior thyroid vessels close to capsule, division of strap muscles and presence of retrosternal extension (Table 2). The equipment used involved a standard surgical set and diathermy. The working diagnosis was based on both the cytology from the FNAC and on clinical examination. Transient Hypocalcaemia was measured clinically by examining for circumoral paraesthesia, carpopedal spasm, muscle fasciculation’s, Trosseau’s and Chvosteks signs. If there was a high index of clinical suspicion serology was performed, voice quality was assessed clinically and an IDL performed only where clinical concern as justified in a 2012 paper by Henry LR et al. [14]. All patients had TFTs at 6 months. Of the 21 patients reported to have deranged TFTs, treatment was only instigated if patients were clinically symptomatic.
Results and discussion
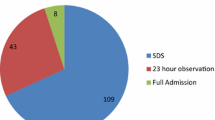
There were 43 patients recruited to this study (Table 3). The operating team comprised three surgeons, a consultant endocrine surgeon and two second year endocrine surgical trainees, who had completed 3 years general surgical training. Seven operations were performed exclusively by the consultant surgeon and 33 were performed independently by the endocrine surgical trainees. International figures for complications vary, but for comparison purposes results from a Scandinavian registry that followed 3,660 patients from 2004 to 2006 were employed [15]. In Uganda, the majority of thyroidectomies performed were for iodine deficient multinodular goitre (MNG). Common presentations to the outpatient clinic included pressure symptoms, hyperthyroidism or cosmetic concerns [16]. The average thyroid weight was 137 g. Other common indications for thyroidectomy were thyroid cancer and Graves’ disease. This correlates with the literature available on thyroid disease in other areas in Africa [17, 18]. Graves’ disease is diagnosed clinically, as antibody testing is not available. Surgery for Graves’ disease is offered for failed medical treatment, severe reaction to the antithyroid medication, enlarged glands which ideally would require costly high-dose radiation and poor patient compliance to drugs. Graves’ patients are given Lugols’ iodine for 2 weeks pre-operatively to reduce the vascularity of the gland. Patients are put on a waiting list for admission to the ward, once they have a haemoglobin measurement, thyroid function tests, FNAC, IDL and a thoracic inlet X-ray performed. Six patients needed pre-surgical treatment for hyperthyroidism. FNAC’s are not routinely ultrasound guided. Fibre optic laryngoscopy is available but utilised only in a few cases. CT scans and radioisotope scans are available in Kampala but are unaffordable for the vast majority of patients. In developed countries total thyroidectomy is the advocated treatment for cancer, Graves’s diseases and increasingly for benign disease. In Mulago Hospital, the choice of operation usually depends on the pathology and the likelihood of the patient affording lifelong thyroxine. The standard practice is to remove all grossly abnormal thyroid tissue and leave normal looking tissue behind. This approach is taken as many patients may never return for follow-up after surgery or replacement thyroxine may not be affordable. The pseudocapsule which contains the compressed normal thyroid tissue is used as the plane of dissection. In a lobectomy, the true capsule is used as the plane of dissection. A total thyroidectomy is only performed where cancer is suspected either pre-operatively or intraoperatively. Therapeutic lymph node dissection is performed only where the surgeon is concerned about extra-thyroid invasion. The use of peri-operative antibiotics is surgeon-dependant. A nurse anaesthetist manages the patient’s airway intraoperatively, with consultant anaesthetist’s input if required. Post-operatively, the patient is brought back to the ward, monitored for 24 h and discharged. There is an intensive care unit available for high-risk cases. Follow-up involves clinical examination, thyroid function tests and serum calcium only if symptomatic. Serum monitoring of thyroglobulin or calcitonin are not available, nor is genetic screening.
RLN paralysis demonstrated a low-powered association where total thyroidectomy was performed (0.005) and where thyroid size was smaller (p = 0.04). Three patients developed permanent RLN paralysis in this study (Table 4). All of these cases were total thyroidectomies. One was redo surgery for MNG performed by a trainee surgeon. Two cases were for cancer, performed by the consultant surgeon and the nerve was clearly identified intraoperatively. There were associations between large thyroid size and permanent hypocalcaemia (0.01) and rebleeding (p = 0.03). Transient voice change was significant in younger patients (p = 0.02). Older patients were statistically more likely to develop a rebleeding (p = 0.01). Rebleeding also occurred in the Scandinavian study with increasing age. Rebleeding occurred in four patients in the Mulago study. One required formal evacuation of the haematoma, two had drains left in situ post-operatively, and the other needed post-operative haematoma aspiration. Shorter operative duration was associated with transient voice change (p = 0.05), permanent hypocalcaemia (p = 0.01) and rebleeding (p = 0.01). Perhaps this reflects the sacrifice of meticulous surgery to operation speed. No patients developed infection in the Mulago study. This may be a reflection of antibiotic administration despite categorisation as clean surgery. The Scandinavian study found infection to be associated with lymph node dissection. Only one patient had lymph node dissection in this study. Airway difficulties (p = 0.02) and transient hypocalcaemia (p = 0.002) were statistically significant in prolonged surgery (>100 min). Only one case was cancelled due to intubation difficulties. Two patients required delayed extubation in the ICU setting because of tracheomalacia. Another three patients complained of breathing difficulties post-operatively.
Whilst the thyroidectomy outcomes are not equal to international standards, an acceptable standard is achievable in this resource-limited setting. The legacy of this study would be to raise the bar from an acceptable standard to an excellent standard in Mulago Hospital. This presents an opportunity for international partnership with an experienced endocrine surgical unit. Cost-effective ways of knowledge sharing include regular video conferencing and scheduling of international teaching visits. In the long term, an international partnership would foster an environment of cross-centre learning and surgical excellence. In summary, poor outcomes in this setting are multifactorial but extremes of thyroid size, extremes of operation duration and total thyroidectomies have been shown to have statistically poorer outcomes.
References
World Bank. http://data.worldbank.org/country/uganda
Andersson M et al (2005) Current global iodine status and progress over the last decade towards the elimination of iodine deficiency. Bull World Health Organ 83(7):518–525
Bimenya GS et al (2002) Monitoring the severity of iodine deficiency disorders in Uganda. Afr Health Sci 2(2):63–68
Taga I et al (2008) Youth of West-Cameroon are at high risk of developing IDD due to low dietary iodine and high dietary thiocyanate. Afr Health Sci 8(3):180–185
Kishosha PA, Galukande M, Gakwaya AM (2011) Selenium deficiency a factor in endemic goiter persistence in Sub-Saharan Africa. World J Surg 35(7):1540–1545. doi:10.1007/s00268-011-1096-5
Woodruff SL et al (2010) Global variation in the pattern of differentiated thyroid cancer. Am J Surg 200(4):462–466
Guilbert JJ (2006) The World Health Report 2006: working together for health. Educ Health (Abingdon) 19(3):385–387
Ozgediz D et al (2008) Africa’s neglected surgical workforce crisis. Lancet 371(9613):627–628
Ozgediz D et al (2008) The neglect of the global surgical workforce: experience and evidence from Uganda. World J Surg 32(6):1208–1215. doi:10.1007/s00268-008-9473-4
Grimes CE et al (2011) Systematic review of barriers to surgical care in low-income and middle-income countries. World J Surg 35(5):941–950. doi:10.1007/s00268-011-1010-1
American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer et al (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19(11):1167–1214. doi:10.1089/thy.2009.0110
Chandrasekhar SS et al (2013) Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol 148(6 Suppl):S1–S37
British Thyroid Association (2007) Guidelines for the management of thyroid cancer. http://www.british-thyroid-association.org/news/Docs/Thyroid_cancer_guidelines_2007.pdf
Henry LR, Abad JD, Stojadinovic A (2012) The voice, not the nerve, is the functionally relevant endpoint. J Surg Oncol 106(8):1005–1006
Bergenfelz AO (2008) Complications of thyroid surgery. Scandinavian quality register for thyroid and parathyroid surgery. Langenbecks Arch Surg 393:667–673
Fualal J (2012) Characterising thyroid disease and identifying barriers to care in Uganda. World J Endocr Surg 4(2):47–53
Ogbera AO, Kuku SF (2011) Epidemiology of thyroid diseases in Africa. Indian J Endocrinol Metab 15(Suppl 2):S82–S88
Rumstadt B et al (2008) Thyroid surgery in Burkina Faso, West Africa: experience from a surgical help program. World J Surg 32(12):2627–2630. doi:10.1007/s00268-008-9775-6
Acknowledgments
The author would like to thank Professor K. Barry, Mayo General Hospital, Ireland for his help.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O Donohoe, N., Kintu-Luwaga, R., Bolger, J. et al. A Prospective Analysis of Thyroidectomy Outcomes in a Resource-Limited Setting. World J Surg 39, 1708–1711 (2015). https://doi.org/10.1007/s00268-015-3009-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3009-5