Abstract
Background
This study was designed to establish a new diagnostic criteria of preoperative nodal status with high specificity on multidetector row computed tomography (MDCT) to extract advanced gastric cancer (GC) patients with an unfavorable prognosis.
Method
From total of 480 GC patients who underwent surgical resection, 58 consecutive patients with a preoperative diagnosis of nodal metastasis on MDCT were included in this retrospective study. Nodal status on MDCT was reassessed and a prognostic analysis was performed in the present study.
Results
Among several clinical nodal diagnostic criteria on MDCT, a cut-off value of the short-axis diameter measuring ≥15 mm showed the highest specificity (100 %). The prognostic analysis revealed that patients with nodal counts on MDCT of ≥3 (p = 0.035) as well as those with a nodal diameter ≥15 mm (p < 0.001) had a significantly poor prognosis. When patients with nodal counts ≥3 and at least one node that was ≥15 mm in diameter on MDCT were defined as having extensive lymph node metastasis (ELM) that had a significantly poor prognosis (5-year survival rates of 20 %, p < 0.001), and ELM was also an independent poor prognostic factor in advanced GC (p = 0.033, hazard ratio 4.038).
Conclusion
GC patients with nodal counts ≥3 and at least one node that was ≥15 mm in diameter on MDCT have extremely worse prognose with high diagnostic specificity. This novel surrogate indicator for preoperative imaging diagnosis may help personalized therapeutic strategies for GC patients with ELM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC) is one of the leading causes of cancer-related deaths worldwide [1]. Although multimodal treatments such as surgery, chemotherapy, and radiotherapy have been used to improve survival rates, the therapeutic outcomes of advanced GC remain unsatisfactory [2]. Recent studies clearly demonstrated that combination therapy such as surgery plus adjuvant chemotherapy improved survival rates in advanced GC, especially in East Asian countries [3, 4]; therefore, the standard treatment for advanced GC is curative gastrectomy followed by postoperative chemotherapy in East Asian countries. However, the survival rates of patients with very advanced GC [especially stage III with extensive lymph node metastasis (ELM)] have been less satisfactory. In terms of good compliance to more powerful and intensive chemotherapeutic regimens, neoadjuvant chemotherapies (NAC) have been preferably tried to improve the survival rates of very advanced GC patients in clinical trials [5–9]. However, the prolonged preoperative treatment occasionally causes disease progression during NAC, and therefore an indication for NAC should be crucial in order to avoid false-indication of NAC for patients with favorable prognosis treated by standard treatments, operation, and postoperative chemotherapy.
Various imaging modalities, such as multidetector row computed tomography (MDCT), endoscopic ultrasonography (EUS), and magnetic resonance imaging (MRI), have been increasingly used for accurate diagnose in clinical settings. Thin-slice MDCT may effectively and precisely diagnose nodal metastasis in GC patients [10–16]. Several reports demonstrated that preoperative nodal status diagnosed by MDCT can predict prognosis of patients with advanced GC. We previously demonstrated that patients with nodal counts on MDCT of ≥3 had a significantly poor prognosis [11]. On the other hand, Tokunaga et al. reported that a selection by the nodal size of the short axis ≥15 mm in diameter showed extremely high specificity and provided prognostic information [12]. However, the 5-year survival rate of the suspected patients with poor-prognostic groups were still around 40–50 % in these studies, which indicated about half of these patients cured by gastrectomy with D2 lymph node dissection.
This study was designed to evaluate the utility of metastatic nodal counts and sizes on MDCT as combination criteria to extract advanced GC patients with an extremely unfavorable prognosis by standard treatments. The results obtained clearly demonstrated that combination criteria of nodal counts and sizes on MDCT could be a reliable surrogate marker for an unfavorable prognosis in patients with advanced GC. Our results suggest that GC patients with nodal counts ≥3 and at least one node that is ≥15 mm in diameter on MDCT have extremely worse prognose with extremely high diagnostic specificity.
Materials and methods
Ethics statement
Written consent was obtained from all patients prior to obtaining clinicopathological data and patient anonymity has been preserved.
Patients
Of a total of 480 GC patients treated at our institution between 2005 and 2009, 58 patients diagnosed with nodal metastasis on preoperative MDCT were included in the present study. The diagnostic accuracy, equivalent to that of other studies, of nodal metastasis was demonstrated previously [10, 11]. All 58 patients underwent curative gastrectomy with Japanese style D2 lymphadenectomy including the perigastric lymph nodes (LN) along the left gastric, common hepatic, and splenic arteries. All patients attended a postoperative follow-up or received additional treatments including those for tumor recurrence at our institution or affiliated hospitals. The median follow-up periods were 34.4 months. Total of 14 patients developed recurrence, of which 3 was peritoneal recurrence, 4 LN recurrence, 5 distant site recurrence, and 3 unknown recurrent site. The number of the recurrent site category described above was overlapped. As for the postoperative adjuvant treatment, the patients with pStage II–III GC after 2008 were essentially received postoperative adjuvant chemotherapy including S-1 chemotherapy as the result of ACTS-GC trial [3]. Of the 58 patients, 19 patients have received adjuvant chemotherapy. As for intraoperative cytology, 43 of the 58 patients were examined by intraoperative cytology, and only 1 patient showed positive status. The other clinicopathological features of our patients were shown in Table 1.
MDCT protocol
Preoperative or pretreatment MDCT was performed on patients who had fasted for more than 8 h using a 64-detector row computed tomography (CT) scanner (Philips Healthcare, Japan). Neither water nor non-ionic contrast medium was administered orally. In all cases, MDCT scanning was performed with patients in the supine position at 120 kV and 300 mA with a standard algorithm and 512 × 512 matrix size. A total of 2.0 ml/kg of non-ionic contrast medium was administered intravenously by an automatic injector at a flow rate of 4.0 ml per second through a 20-gage needle placed in the antecubital vein. CT scanning was performed in the late arterial phase [start delay, 6 s after the CT number at the bifurcation of the celiac artery marked by a range of interest (ROI) reached 200 Hounsfield unit (HU)], portal venous phase (30 s), and delayed phase (60 s). The scanning range included the whole abdomen and pelvis, from the level of the diaphragmic domes to the anal verge. We reconstructed raw data at 1.0 mm thicknesses for transverse CT images. In the present study, the portal venous phase was used to evaluate nodal metastasis and the arterial phase was used to identify the anatomical localization of arteries such as the left and right gastric arteries. All of the MDCT protocols were according to those used in regular routine work at our institution [10, 11].
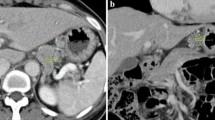
Clinical and pathological diagnosis of lymph node metastasis
As demonstrated in our previous studies [10, 11], we mainly used a cine-mode display of CT images and precisely counted all regional LN considered to show metastatic involvement if they had a diameter larger than 8 mm, high contrast medium enhancement that was defined as attenuation greater than 100 HU in the postcontrast portal venous phase, and a round shape [13, 15, 17]. The average CT value of the nodal section was measured for each lymph node. Independent radiologists at our institution had previously confirmed all metastatic regions. Regional LN were counted and categorized according to 16 different anatomic sites based on the Japanese gastric cancer classification (JCGC) [18]. Both the shortest and longest diameters of all metastatic LN were subsequently measured and reassessed at each regional site by the reconstructed data of pretreatment MDCT.
After surgery, all dissected LN were subjected to a pathological examination, fixed in buffered formalin, and embedded in paraffin. Pathologists in our institution examined embedded LN by sectioning slices in the plane of the largest node dimension to confirm the presence of metastasis.
Statistical analysis
Univariate analysis of the relationship between clinicopathological features and the two groups of combination criteria of ELM on MDCT was performed using the χ 2 test and Fisher’s exact probability test. To assess survival, Kaplan–Meier survival curves were constructed for groups based on univariate predictors and differences between the groups were tested with the log-rank test. The Cox proportional hazards model was used for further evaluations of multivariate survival analysis. p value <0.05 was considered significant. Statistical analyses were conducted using JMP 10 (SAS Institute Inc., Cary, NC).
Results
Diagnostic accuracy of nodal metastasis based on the reassessment of preoperative MDCT for gastric cancer patients
A diagnostic reassessment was performed based on each cut-off value of the lymph node size on MDCT in this GC cohort. The results obtained demonstrated that the cut-off value of the short axis ≥15 mm in diameter showed the highest specificity (100 %) for the diagnosis of lymph node metastasis (Table 2). The results of accuracy including other cut-off values were compatible with previous findings [12, 15, 16].
Survival analyses of each group divided according to the nodal counts and/or sizes
We previously demonstrated that metastatic nodal counts on MDCT correlated with the pathological diagnosis using Spearman’s correlation test, and a function was derived from the analysis, y = 1.63x + 2.50, between nodal counts on MDCT and the pathological diagnosis (y, pathologic nodal counts; x, nodal counts on MDCT) [11]. Nodal counts on MDCT of ≥3 corresponded to pathogenic N3 based on the forecast function of the Spearman’s correlation test. According to the prognostic analysis, patients with nodal counts on MDCT of ≥3 (p = 0.035; Fig. 1a) as well as those with a nodal diameter ≥15 mm (p < 0.001; Fig. 1b) had a significantly poor prognosis. Since the patients with nodal counts ≥3 and at least one node that was ≥15 mm in diameter on MDCT were defined as having ELM, they had a significantly poor prognosis (p < 0.001) (Fig. 1c).
Survival analysis of each group according to nodal counts and sizes on MDCT (Kaplan–Meier survival curve and log-rank test). Patients with nodal counts on MDCT of ≥3 (p = 0.035, a) as well as those with a nodal diameter ≥15 mm (p < 0.001, b) had a significantly poor prognosis. When patients with nodal counts ≥3 and at least one node that was ≥15 mm in diameter on MDCT were defined as having extensive lymph node metastasis (ELM), they had a significantly poor prognosis (p < 0.001) (c)
Multivaliable survival analysis by the Cox proportional hazards model
No correlation was observed between the clinicopathological factors and the status of the combination criteria of ELM on MDCT, except for pathological nodal status (Table 3). Multivariable survival analysis using Cox proportional hazards model demonstrated that the combination criteria of ELM on MDCT was an independent poor prognostic factor in patients with advanced GC (p = 0.033, hazard ratio 4.038) as well as the tumor gross type and tumor location (Table 4).
Discussion
The emergence of high-performance modalities such as MDCT has recently allowed for the precise perioperative diagnosis of GC staging [10–13, 16, 17]. Pathological number of metastatic LN was previously defined as one of the most important prognostic factors in GC patients [19–23]. Therefore, a preoperative or pretreatment diagnosis of metastatic nodes is essential for establishing appropriate therapeutic strategies. We previously demonstrated that metastatic nodal counts (especially four LN or more) on preoperative MDCT were associated with the surgical curability of GC. Regarding surgical curability, diagnostic laparoscopy has recently been performed on patients suspected of having locally advanced and/or distant metastases in order to evaluate the extent of the cancer. Laparoscopy prior to surgical resection provides useful information regarding resectability in these patients. On the other hand, Tokunaga et al. also demonstrated that preoperative nodal sizes on MDCT could affect the long-term prognosis of GC patients [12]. These findings suggested that the preoperative nodal status on MDCT is extremely important for assessing the malignant status and therapeutic strategies in each case of GC.
The standard treatment for advanced GC in East Asian countries is currently curative gastrectomy followed by postoperative chemotherapy [3, 4]. More potent postoperative chemotherapy and preoperative chemotherapy have been attempted in order to further improve the prognosis of patients with very advanced GC [5–7, 24, 25]. Several clinical trials have been conducted to evaluate the efficacy of neoadjuvant chemotherapy in GC patients, many of which were intended for GC patients with type 4 or ELM [6, 8, 9]. Recently, results of two clinical trial on neoadjuvant chemotherapy were reported, one for GC patients with clinically resectable type 4 and large type 3 and the other for GC patients with bulky lymph node metastasis along the coeliac artery and its branches and/or para-aortic lymph node metastasis [9, 26]. Both trials suggested that neoadjuvant chemotherapy was safe and effective for some of the study patients with extremely poor prognosis; however, neoadjuvant chemotherapy followed surgery achieved a better prognosis in GC patients with ELM compared to those with type 4 or large type 3. These finding may suggest that the treatment strategy, surgery after neoadjuvant chemotherapy, is appropriate for GC patients with ELM [6, 9]. Patients with pathologically confirmed ELM have an extremely poor prognosis; however, an accurate preoperative evaluation of lymph node metastasis is generally considered too difficult. The eligibility criteria of several clinical trials for ELM on MDCT have been broadly defined in many ways.
We initially provided forecast nodal counts on MDCT of ≥3, corresponding to pathological N3, using the correlation function described in our previous study [11]. According to the survival analysis, patients with nodal counts on MDCT of ≥3 (p = 0.035; Fig. 1a) had a significantly poor prognosis. However, the 5-year survival rate of patients with nodal counts on MDCT of ≥3 was still more than 50 %, which indicated that the criteria included patients with relatively a good prognosis. Some patients with nodal counts on MDCT of ≥3 were found to be negative for lymph node metastasis. On the other hand, a selection by the nodal size of the short axis ≥15 mm in diameter, as previously reported by Tokunaga et al. showed extremely high specificity (100 %) and also provided prognostic information. However, patients with the nodal size of the short axis ≥15 mm in diameter still had a 5-year survival of approximated 40 %. This finding indicated that some of these patients only had lymph node metastasis in one node and were cured by gastrectomy with D2 lymph node dissection. Therefore, we hypothesized that the combination criteria of nodal counts and sizes on MDCT may enable us to provide a surrogate indicator for ELM with high specificity, and also to extract advanced GC patients with an unfavorable prognosis. The results of the present study clearly demonstrated that our combination criteria of ELM on MDCT (nodal counts of ≥3 and at least one node that is ≥15 mm in diameter) could extract patients with an extremely poor prognosis whose 5-year rate survival was less than 20 %, and was also an independent poor prognostic factor in patients with advanced GC with clinically positive nodes. The counterpart group of our combination criteria still had a relatively good 5-year survival rate of more than 75 %, although all patients were suspected of having clinically lymph node metastasis on MDCT. These results indicate that our combination criteria accurately extracted patients with an extremely poor prognosis only, and most counterparts were cured by standard treatments consisting of gastrectomy with D2 lymph node dissection and postoperative chemotherapy.
One of the limitations on imaging diagnosis is inter-observer difference. Inter-observer differences are a crucial problem in prospective multicenter studies using imaging modalities. However, our criteria were simply defined by nodal counts and the sizes of LN; therefore, we considered our combination criteria to be highly reproducible and also relevant to clinical practice. Therefore, further studies with a large cohort are needed to confirm these results.
In conclusion, GC patients with nodal counts of ≥3 and at least one node that is ≥15 mm in diameter on MDCT have an extremely poor prognosis with high diagnostic specificity. These patients may be suitable as candidates in future clinical trials to investigate the efficacy of NAC.
References
Parkin DM, Bray F, Ferlay J et al (2005) Global cancer statistics, 2002. CA Cancer J Clin 55:74–108
Jansen EP, Boot H, Verheij M et al (2005) Optimal locoregional treatment in gastric cancer. J Clin Oncol 23:4509–4517
Sakuramoto S, Sasako M, Yamaguchi T et al (2007) Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med 357:1810–1820
Bang YJ, Kim YW, Yang HK et al (2012) Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet 379:315–321
Kinoshita T, Sasako M, Sano T et al (2009) Phase II trial of S-1 for neoadjuvant chemotherapy against scirrhous gastric cancer (JCOG 0002). Gastric Cancer 12:37–42
Yoshikawa T, Sasako M, Yamamoto S et al (2009) Phase II study of neoadjuvant chemotherapy and extended surgery for locally advanced gastric cancer. Br J Surg 96:1015–1022
Inoue T, Yachida S, Usuki H et al (2012) Pilot feasibility study of neoadjuvant chemoradiotherapy with S-1 in patients with locally advanced gastric cancer featuring adjacent tissue invasion or JGCA bulky N2 lymph node metastases. Ann Surg Oncol 19:2937–2945
Yoshikawa T, Tsuburaya A, Sano T et al (2011) Gastric cancer Surgical Study Group of Japan Clinical Oncology Group A phase II study of preoperative chemotherapy with S-1 (S) and cisplatin (P) followed by D3 gastrectomy for gastric cancer (GC) with extensive lymph node metastasis (ELM): survival results of JCOG0405. J Clin Oncol 29:2011(Suppl. 4)
Tsuburaya A, Mizusawa J, Tanaka Y et al (2014) Neoadjuvant chemotherapy with S-1 and cisplatin followed by D2 gastrectomy with para-aortic lymph node dissection for gastric cancer with extensive lymph node metastasis. Br J Surg 101:653–660
Kawaguchi T, Ichikawa D, Komatsu S et al (2011) Clinical evaluation of JCGC and TNM staging on multidetector-row computed tomography in preoperative nodal staging of gastric cancer. Hepatogastroenterology 58:838–841
Kawaguchi T, Komatsu S, Ichikawa D et al (2012) Nodal counts on MDCT as a surrogate marker for surgical curability in gastric cancer. Ann Surg Oncol 19:2465–2470
Tokunaga M, Sugisawa N, Tanizawa Y et al (2013) The impact of preoperative lymph node size on long-term outcome following curative gastrectomy for gastric cancer. Ann Surg Oncol 20:1598–1603
Kwee RM (2009) Kwee TC Imaging in assessing lymph node status in gastric cancer. Gastric Cancer 12:6–22
Shinohara T, Ohyama S, Yamaguchi T et al (2005) Clinical value of multidetector row computed tomography in detecting lymph node metastasis of early gastric cancer. Eur J Surg Oncol 31:743–748
Hasegawa S, Yoshikawa T, Shirai J et al (2013) A prospective validation study to diagnose serosal invasion and nodal metastases of gastric cancer by multidetector-row CT. Ann Surg Oncol 20:2016–2022
Morgagni P, Petrella E, Basile B et al (2012) Preoperative multidetector-row computed tomography scan staging for lymphatic gastric cancer spread. World J Surg Oncol 10:197
Fukuya T, Honda H, Hayashi T et al (1995) Lymph-node metastases: efficacy for detection with helical CT in patients with gastric cancer. Radiology 197:705–711
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma 3rd English edition. Gastric Cancer 14:101–112
Makino M, Moriwaki S, Yonekawa M et al (1991) Prognostic significance of the number of metastatic lymph nodes in patients with gastric cancer. J Surg Oncol 47:12–16
Jaehne J, Meyer HJ, Maschek H et al (1992) Lymphadenectomy in gastric carcinoma. A prospective and prognostic study. Arch Surg 127:290–294
Ichikura T, Tomimatsu S, Okusa Y et al (1993) Comparison of the prognostic significance between the number of metastatic lymph nodes and nodal stage based on their location in patients with gastric cancer. J Clin Oncol 11:1894–1900
Roder JD, Bottcher K, Siewert JR et al (1993) Prognostic factors in gastric carcinoma. results of the German gastric carcinoma study 1992. Cancer 72:2089–2097
Adachi Y, Kamakura T, Mori M et al (1994) Prognostic significance of the number of positive lymph nodes in gastric carcinoma. Br J Surg 81:414–416
Cunningham D, Allum WH, Stenning SP et al (2006) Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med 355:11–20
Knight G, Earle CC, Cosby R et al (2013) Neoadjuvant or adjuvant therapy for resectable gastric cancer: a systematic review and practice guideline for North America. Gastric Cancer 16:28–40
Iwasaki Y, Sasako M, Yamamoto S et al (2013) Phase II study of preoperative chemotherapy with S-1 and cisplatin followed by gastrectomy for clinically resectable type 4 and large type 3 gastric cancers (JCOG0210). J Surg Oncol 107:741–745
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kawaguchi, T., Ichikawa, D., Komatsu, S. et al. Impact of Combination Criteria of Nodal Counts and Sizes on Preoperative MDCT in Advanced Gastric Cancer. World J Surg 40, 158–164 (2016). https://doi.org/10.1007/s00268-015-3007-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3007-7