Abstract
Background
Botulinum toxin type A is a widely used treatment of facial wrinkles. The objective of this study was to compare the efficacy and safety of a new botulinum toxin type A (Masport [abobotulinum toxin A], MasoonDarou Co) with DYSPORT® for the treatment of glabellar lines.
Methods
262 subjects with moderate-to-severe glabellar lines received either a fixed dose of 50 units of MASPORT® or DYSPORT® (Ipsen Company, England). Subjects were followed up at 14, 30, 60, 90 and 120 days after injection. Efficacy was assessed by investigator at maximum frown and rest and also by Subject Global Assessment of Change (SGA). The responders were defined as persons with +2 grade improvement from baseline for both investigator and patient assessment. The occurrence and duration of adverse effects were recorded up throughout the study.
Results
According to the investigator evaluations, the responder rate at maximum frown were 94.5% for MASPORT and 95.6% for DYSPORT group on day 30 and at rest were 85.45% and 85.68% for MASPORT and DYSPORT group, respectively. According to the subject self-assessment, the proportion of responders in MASPORT group at day 30 was 95.28% versus 97.04% for DYSPORT group. No serious drug related adverse effect was recorded in either study groups, and the rates of adverse effects were similar for both groups.
Conclusion
Abobotulinum toxin A [MASPORT] is equally safe and effective as commercial product [DYSPORT] for the treatment of glabellar lines with the dose of 50 units, up to 120 days.
Level of Evidence I
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, there has been an increasing demand for methods to prevent skin aging, driven by the growing older population worldwide. Aging leads to the gradual shortening and tightening of facial muscles due to repeated contractions over time. As a result, there is an increase in muscular tone at rest, causing facial lines to become fixed even in the absence of muscle contraction [1, 2]. These lines commonly appear in three areas: the forehead (frontal lines), between the eyebrows (glabellar lines), and near the eyes (crow's feet lines), and are considered the initial signs of aging. These facial lines can significantly impact a person's appearance, sometimes conveying negative expressions such as anger or sadness, even when the person does not experience those emotions at that moment. This can result in a misperception by others. Evidence suggests that facial lines have a direct effect on a person's self-confidence and social interactions [3,4,5].
Clostridium botulinum toxin, a neurotoxin that inhibits the release of acetylcholine mediated by calcium, acts as a muscle paralyzer. By inhibiting muscle contraction, it can be used as a preventive or therapeutic option for wrinkles. Since its approval by the US FDA in 1989 for the treatment of strabismus and blepharospasm, botulinum toxin has been used for various medical conditions, including neurogenic overactive bladder, cervical dystonia, axillary hyperhidrosis, and chronic migraine. Currently, botulinum toxin is widely utilized as a minimally invasive procedure for treating facial lines [6,7,8].
Several brands of botulinum toxin are available in the market, with Botox (Allergan, Irvine, CA, USA), Dysport (Ipsen Limited, Slough, UK), and Xeomin (Merz pharmaceutical, Frankfurt, Germany) being the most commonly used brands. These three brands were approved by the FDA for temporary treatment of moderate-to-severe glabellar lines in April 2002, April 2009, and July 2011, respectively [9]. In Iran, these brands are also widely used. In 2013, the Food and Drug Administration of Iran approved a new formulation of Abo botulinum toxin called MASPORT, which is provided in vials containing 500 units of lyophilized botulinum toxin type A powder for the treatment of glabellar lines [10].
Numerous studies have evaluated the efficacy and safety of different botulinum toxin brands, all of which have demonstrated the effectiveness of this substance in reducing the severity of facial lines [11]. Reported side effects have generally been minimal and transient, including mild swelling of the eyelids or glabellar region, pain at the injection site, ecchymosis, and headaches [12, 13]. The objective of this study was to compare the efficacy and safety of a single-dose administration of a newly developed botulinum toxin type A formulation (MASPORT) with a commercial product (DYSPORT) in reducing glabellar lines.
Material and Methods
Study Design
This study was a double-blind, randomized, comparative phase III clinical trial conducted at RAZI Hospital, which is a dermatology reference hospital in Iran. The study took place between June and September 2013. The study protocol underwent review by the Ethic Committee of Tehran University of Medical Science and was approved by the Iranian Registry of Clinical Trials with the code number IRCT2013100214871N1.
Study Subjects
The study enrolled subjects between the ages of 18 and 60 who had moderate-to-severe glabellar lines at maximum frown, as assessed using a 4-point glabellar line severity scale. Subjects with medical conditions that could be exacerbated by botulinum toxin injection, such as the consumption of aminoglycosides or the presence of muscular dystrophy, myasthenia gravis, Eaton Lambert syndrome, or amyotrophic lateral sclerosis, were excluded from the study. Individuals with allergies to any of the ingredients in the products (botulinum toxin, lactose, albumin, hemagglutinin) were also not allowed to participate. Those who had received botulinum toxin injections for any condition within the 6 months prior to the study were excluded as well. Pregnant and lactating women were not eligible to participate. The study procedures and potential risks were explained to the participants, and they were informed that they could withdraw from the study if they were unable to attend medical evaluations, experienced serious diseases during the study, or at the discretion of the physician. After receiving the necessary explanations, eligible participants provided written consent.
Study Treatment and Procedure
Subjects were randomly assigned into two groups of test or control. As the control medication, each vial of DYSPORT contains 500 units of Abo botulinum toxin type A that is dissolved in lactose solution containing human serum albumin, and finally it has been lyophilized. As the test drug, each vial of MASPORT with a formulation very similar to DYSPORT contains 500 international units of lyophilized powder Abo botulinum toxin type A along with human serum albumin and lactose as stabilizer. The contents of the DYSPORT and MASPORT vials were diluted with 2.5 cc of normal saline, resulting in a final concentration of approximately 200 units per ml. The labels on the botulinum toxin vials were fully covered, and each individual study dose was prepared according to the protocol by a designated trainer. The type of product used for each patient was coded so that neither the patient, physician, nor evaluator knew which drug was administered. On day 0, participants received a total dose of 50 units of MASPORT or DYSPORT, which was evenly distributed in 5 points in the glabellar area. This involved injecting BoNT-A into the midline procerus muscle and inferomedial and superior middle aspect of corrugator muscle (Figure 1). To prevent ptosis caused by downward diffusion of BoNT-A, injections were administered at least 1 centimeter above the periorbital bony rim. Each injection point received approximately 0.05 cc of the solution using a 27-Gauge needle.
Clinical Outcome Measurement
The severity of glabellar lines at maximum frown and rest was evaluated by the investigator on day 0. Follow-up evaluations were conducted on days 14, 30, 60, 90, and 120. The efficacy of the treatment was assessed by the investigator's evaluation of the severity of glabellar lines at maximum frown and relax on days 30, 60, 90, and 120, using a 4-point severity scale ranging from 0 (no lines) to 3 (severe lines). The Subject Global Assessment of Change (SGA) was also used for efficacy assessment, employing a 4-point scale ranging from 0 to 3 (0 = no improvement, 1 = partial improvement, 2 = significant improvement, 3 = complete improvement) (Table 1). To ensure standardized scoring of glabellar lines, a photo guide was provided to the investigators.
Before the study and on day 120, laboratory blood tests were conducted, including measurements of triglycerides, cholesterol, sodium, albumin, SGOT, SGPT, and alkaline phosphatase. These factors, along with in-person examinations and participants' self-reporting, were used to evaluate adverse drug reactions. Anti-botulinum toxin antibodies were also checked on day 0 and 120.
Efficacy Endpoints and Statistical Analysis
The efficacy endpoints of the study were based on the investigator evaluations and patient-reported outcomes. The responder population was defined as the percentage of patients whose glabellar lines improved from moderate or severe to no or mild lines, as assessed by the investigator. Based on patient-reported outcomes, a responder was defined as a patient who reported complete or significant improvement in their glabellar lines compared to baseline (Table 2).
All statistical analyses were performed using Minitab 20.4.0 software. Between-group comparisons were analyzed using a paired t-test with a 95% confidence interval and an alpha error of 0.05.
Results
Patient Population
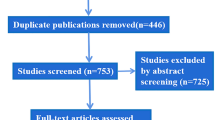
A total of 262 individuals who met the inclusion criteria participated in this study. They were randomly assigned to either the test group (48.5%) or the control group (51.5%). All participants remained in the study until the 90th day of follow-up, except for a subset of patients who did not attend the follow-up assessments for glabellar lines at maximum frown, rest, and Subject Global Assessment (SGA) at the 120th day. In the test group, 22, 25, and 22 patients did not attend the assessments at 120th day for max frown, rest, and SGA, respectively. In the control group, 28, 18, and 18 patients did not attend the assessments at 120th day for max frown, rest, and SGA, respectively (Figure 2). Demographic characteristics, including mean age, age distribution within groups, male-female ratio, and ethnicity, were similar between the two groups, indicating proper randomization and uniform distribution (Table 3). The severity of glabellar lines at maximum frown and rest was assessed by an investigator on day 0, and there was no significant difference in the severity of glabellar lines between the two groups at baseline (p > 0.99) (Table 4).
Efficacy Assessment
Investigator Evaluation of Glabellar Line Severity at Maximal Frown
According to investigator evaluations, the mean severity score in the MASPORT group on day 0 was 2.57 at maximum frown. After treatment, the severity score significantly decreased to 0.16 on day 14, indicating a 2.5-grade improvement. This decreasing trend continued, reaching its peak on the 60th day (0.11). Even at the end of the follow-ups, all patients still showed more than a 2-grade improvement compared to baseline (Figure 3a). In the control group, the improvement of glabellar lines at maximum frown was also significant compared to baseline, with no significant difference observed between the test and control groups (p = 0.97).
The responder rate, defined as patients with moderate or severe glabellar lines at baseline and no or mild glabellar lines at follow-ups, was high in both the test group (94.5%) and the control group (95.6%) at day 30. The proportion of responders remained above 90% in the test group and 86% in the control group even at the 120th day of follow-up (Figure 3b). Based on investigator evaluation of glabellar line severity at maximum frown, there was no significant difference in the effectiveness of the two products (p = 0.90). Figure 4 illustrates the improvement of glabellar lines at maximum frown for two patients at baseline and 30 days after MASPORT and DYSPORT injection.
photographs of two patients at maximal frown at base line (left) and 30 days after botulinum toxin injection (right) for Masport group (up) and Dysport group (down). A noticeable reduction in frown lines can be clearly seen on the 30th day of botulinum toxin injection for both test and control groups
Investigator Evaluation of Glabellar Line Severity at Rest
The improvement of glabellar lines at rest was evaluated only in individuals with moderate or severe glabellar lines at rest, as this subgroup showed noticeable changes. This subgroup accounted for 43.3% of the MASPORT group and 46.6% of the control group. The mean severity score for the MASPORT subgroup was 2.19 at day 0, which significantly decreased to 0.14 at day 30. In the DYSPORT subgroup, the mean severity score improved from 2.12 at day 0 to 0.13 at day 30. Overall, no significant difference was observed between the test and control groups (p = 0.96) (Figure 5a). The responder rate for the MASPORT and DYSPORT subgroups was high, with 85.45% and 85.68% of individuals, respectively, showing a response to treatment at day 30. There was no significant difference between the two groups (p = 0.72) (Figure 5b).
Subject Global Assessment of Change
Patients were asked to rate the improvement of their glabellar lines on a 4-point scale (from 0 = no improvement to +3 = complete improvement) at various time points after treatment compared to baseline. On day 30, 95.28% of the test group reported complete or significant improvement, with 79.53% considered as responders at the 120th follow-up. The findings of the control group were similar, with 97.04% and 82.22% of individuals reporting complete or significant improvement on day 30 and 120, respectively (Table 5).
Safety Assessments
Participants in the 120-day follow-up did not report any serious adverse effects necessitating the discontinuation of the study. The most frequently reported adverse effects in both study groups included headache, eyelid ptosis, drowsiness, rhinorrhea, and headache associated with rhinorrhea (Table 6). Headaches typically began 10–12 h after BoNT-A injection and lasted up to a day. Eyelid ptosis persisted for less than a month, and its mild nature did not require intervention. Evaluation of blood tests, including triglycerides, cholesterol, sodium, albumin, SGOT, SGPT, and alkaline phosphatase, showed no significant changes compared to baseline values. There were no significant differences between the two groups concerning these blood factors (p >0.05). However, some hematological parameters, including calcium, potassium, bilirubin, creatinine, uric acid, and blood sugar levels, exhibited slight changes 120 days after drug administration compared to baseline values, but these changes were not significant (p>0.05). Anti-botulinum antibody tests revealed the absence of anti-botulinum antibodies in any of the samples collected from the subjects at the beginning and end of the study.
Discussion
The results of this double-blind, randomized, comparative study confirm the effectiveness and safety of a single dose of 50 units of BoNT-A MASPORT in treating moderate-to-severe glabellar lines, reaffirming previous studies' findings on the efficacy and safety of botulinum toxin for reducing glabellar lines. The responder rates for both maximal frown and rest at day 30, as assessed by investigators, were 94.5% and 85.45%, respectively, and remained high throughout the study. There was no significant difference between MASPORT and DYSPORT. Patient outcome measures also demonstrated a high responder rate of 95.28% for MASPORT at day 30, with no difference observed between the two brands. After 120 days, nearly 80% of patients still experienced the full effect of MASPORT, suggesting a potential continuation of the treatment's effects beyond four months, although longer follow-up studies are needed to confirm this.
The peak effect of MASPORT was reported by investigators and subjects to occur between 30 and 60 days after injection, gradually diminishing over time. The safety profile of MASPORT, consistent with previous studies, showed that botulinum toxin type A is safe and well-tolerated at therapeutic doses. The most commonly reported side effects were headache, drowsiness, drooping eyelids, rhinorrhea, and headache associated with rhinorrhea. In a meta-analysis comprising 24 articles, Zargaran et al. conducted a comprehensive examination of the safety profile of 4268 botulinum toxin injections administrated in the glabellar and forehead regions. The results indicated that upper facial botulinum toxin injection is generally safe, with predominantly mild and transient side effects. The study revealed a 16% incidence of side effects, with headache and migraine exhibiting the highest prevalence rate at 6.3%, following by injection site complication and facial neuromuscular complications (such as drooping eyelids, weakness, pain, stiffness, etc.) exhibited a substantial prevalence rate. Additionally, general symptoms such as fatigue, vertigo, and flulike syndromes demonstrated a low occurrence rate [14] and these findings align with the results obtained in our study.
According to the previous studies, blepharoptosis as a common complication of botulinum toxin injection has a prevalence of 1–5% and it caused by the unintended spread of botulinum toxin through the orbital septum, and therefore, it is highly dependent on the injection technique, and it can be prevented by injecting at least 1–2 cm above the orbital rim [15,16,17]. In this study, blepharoptosis has a logical occurrence rate of below 3%.
Conclusion
In conclusion, the results of this study, consistent with previous research, demonstrate that botulinum toxin type A is a safe and well-tolerated treatment option for glabellar lines. MASPORT, at a dose of 50 units, is equally effective and safe compared to its biosimilar counterpart DYSPORT, which is unsurprisingly given their similarity in name. The peak effect occurs between 30 and 60 days after administration, and the effects last for more than four months in over 90% of participants, suggesting potential long-lasting effects. The most commonly reported adverse effects, including headache, blepharoptosis, and drowsiness, were mild and did not require intervention.
References
Kattimani V, Tiwari RVC, Gufran K, Wasan B, Shilpa PH, Khader AA (2019) Botulinum toxin application in facial esthetics and recent treatment indications (2013–2018). J Int Soc Prev Commun Dent 9:99–105
Swift A, Liew S, Weinkle S, Garcia JK, Silberberg MB (2021) The facial aging process from the “Inside Out.” Aesthet Surg J 41:1107–1119
Dayan S, Yoelin SG, De Boulle K, Garcia JK (2019) The psychological impacts of upper facial lines: a qualitative, patient-centered study. Aesthet Surg J Open Forum. https://doi.org/10.1093/asjof/ojz015
Yaworsky A, Daniels S, Tully S et al (2014) The impact of upper facial lines and psychological impact of crow’s feet lines: content validation of the Facial Line Outcomes (FLO-11) Questionnaire. J Cosmet Dermatol 13:297–306
Pereira IN, Hassan H (2022) Impact of botulinum toxin for facial aesthetics on psychological well-being and quality of life: evidence-based review. J Plast Reconstr Aesthet Surg 75:4450–4463
Hu L, Feng Y, Liu W, Jin L, Nie Z (2019) Botulinum toxin type A suppresses arterial vasoconstriction by regulating calcium sensitization and the endothelium-dependent endothelial nitric oxide synthase/soluble guanylyl cyclase/cyclic guanosine monophosphate pathway: an in vitro study. Exp Biol Med 244:1475–1484
Whitcup SM (2021) The history of botulinum toxins in medicine: a thousand year journey. Handb Exp Pharmacol 263:3–10
Moon H, Fundaro SP, Goh CL, Hau KC, Paz-Lao P, Salti G (2021) A review on the combined use of soft tissue filler, suspension threads, and botulinum toxin for facial rejuvenation. J Cutan Aesthet Surg 14:147–155
Ahsanuddin S, Roy S, Nasser W, Povolotskiy R, Paskhover B (2021) Adverse events associated with botox as reported in a food and drug administration database. Aesthet Plast Surg 45:1201–1209
Comparison of safety and efficacy of MASPORT® to commercial product in treatment of patients with glabellar lines. Available at https://en.irct.ir/trial/14339. Accessed on Dec 2013
Gangigatti R, Bennani V, Aarts J, Choi J, Brunton P (2021) Efficacy and safety of Botulinum toxin A for improving esthetics in facial complex: a systematic review. Braz Dent J 32:31–44
Witmanowski H, Błochowiak K (2020) The whole truth about botulinum toxin - a review. Postepy Dermatol Alergol 37:853–861
Sethi N, Singh S, DeBoulle K, Rahman E (2021) A review of complications due to the use of botulinum toxin a for cosmetic indications. Aesthet Plast Surg 45:1210–1220
Zargaran D, Zoller F, Zargaran A et al (2022) Complications of cosmetic botulinum toxin a injections to the upper face: a systematic review and meta-analysis. Aesthet Surg J 42:327–336
Nestor MS, Han H, Gade A, Fischer D, Saban Y, Polselli R (2021) Botulinum toxin-induced blepharoptosis: Anatomy, etiology, prevention, and therapeutic options. J Cosmet Dermatol 20:3133–3146
King M (2016) Management of ptosis. J Clin Aesthet Dermatol 9:E1–E4
Borba A, Matayoshi S, Rodrigues M (2022) Avoiding complications on the upper face treatment with botulinum toxin: a practical guide. Aesthet Plast Surg 46:385–394
Acknowledgments
The authors would like to express their gratitude to all the volunteers who participated in the study and the staff at Razi Hospital for their assistance.
Funding
This study is fully founded by MasoonDarou Co.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kamand Hedayat and Amir Hooshang Ehsani have no conflict of interest to declare.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from eligible participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hedayat, K., Ehsani, A.H. A Phase III Clinical Study of the Efficacy and Safety of Botulinum Toxin Type A (MASPORT) with DYSPORT for the Treatment of Glabellar Lines. Aesth Plast Surg 48, 324–332 (2024). https://doi.org/10.1007/s00266-023-03766-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-023-03766-5