Abstract
Background
Congenital inverted nipple is not uncommon in Asian females, which impairs the patient’s psychology and breastfeeding function. Although various methods have been reported in references, no consensus has been reached on an ideal treatment for severe inverted nipples.
Objectives
This study aimed to propose a minimally invasive and reliable method that could correct severe inverted nipples, reduce their recurrence rate, and create a definite nipple neck for a natural shape.
Methods
We designed a two-step technique to correct severe inverted nipples, including congenital grade III inversion and recurrent grade III inversion with or without scar adhesion after correction with different methods from other hospitals. A retrospective study was performed on 38 patients (68 nipples) who underwent the new two-step technique in our department. The follow-up time was at least 6 months. Patient demographics, operation details, and complication rate were documented.
Results
A total of 68 nipples in 38 patients (bilateral: 30 patients; unilateral: 8 patients) received correction, among which there were four recurrent cases from other hospitals treated with different methods. In this study, the total recurrence rate was 7.89%. In these cases, the nipple exhibited the appearance of Grade I inversion, but not back to the preoperative state of Grade III. There was one case that suffered exposure of thread knot.
Conclusions
The two-step technique is a minimally invasive method to successfully correct severe inverted nipples with a low recurrence rate and achieve a natural shape with a definite nipple neck.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital nipple inversion is a common malformation affecting 2–10% women [1]. The deformity can be bilateral or unilateral. It can result in esthetic dissatisfaction, psychological discomfort, and functional problems, such as local irritation, inflammation, and inability to breastfeeding. The inverted nipples could be classified into grade I, II, III by Han and Hong [2]. Grade III is the most severe nipple inversion, which commonly appears as a crater deformity in the center of the areola. In grade III, there is severe soft tissue deficiency, the milk ducts are very short and extremely difficult to pull out manually.
Although various methods have been reported in references [3,4,5,6,7,8,9], severe cases of inverted nipples usually cannot be corrected by a simple procedure without cutting the lactiferous ducts. The gradual traction technique was the most commonly used method for the correction of inverted nipples in our center over the past decades. The vital advantage of this technique, for example, the minimal damage of the ducts and nerve has been reported in several studies [4, 10, 11]. This technique has also achieved promising and long-lasting results for grade I and II nipple inversion. However, the use of gradual traction technique alone for grade III nipple inversion is still dissatisfied by a relatively high recurrence rate [4].
Therefore, we introduced a new two-step technique for severe inverted nipples. Firstly, we adopted the gradual traction technique to draw out the inverted nipple tissue. Secondly, we used a simplified Jeong’s suture technique to reduce the recurrence rate [12]. This technique could also create a definite nipple neck which is important for a natural shape.
Methods
Patients with congenital grade III inverted nipples and recurrent grade III inverted nipples with or without scar adhesion after correction with different methods in other hospitals were included in this study and underwent surgery with our two-step technique from Feb 2019 to Nov 2020. And the follow-up time in the study was calculated from the day after the second-step procedure and was followed up until November 29, 2021. This study was approved by the institutional review board of our hospital and complied with the principles of the Declaration of Helsinki. Written consent was obtained from all patients.
Surgical Technique
All operations were conducted by the corresponding author, assisted by the doctors from the same group.
The First-Step Procedure
We adopted the gradual traction technique. To make a retractor, a 10 ml single-use syringe (internal diameter was 1.5 cm) was used. The plunger and the needle end of the syringe were removed, retaining a length of 1.3–1.5 cm from the handle end. Four symmetry pinholes (at 3, 6, 9, 12 o’clock) were punctured with an 18-gauge syringe needle on the handle base.
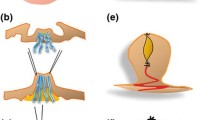
Local anesthesia using 0.5% lidocaine mixed with 1:200,000 epinephrine on the base of the nipple and NAC was performed. A stitch was running across the deep center of the nipple to stretch the tissues. An 18-gauge syringe needle was curved and then made to run through the deep core of the nipple in the vertical direction. With the guidance of the 18-gauge syringe needle, a steel wire with a diameter of 0.6 mm was crossed through the base of the nipple. Then, the same manipulation was performed in the horizontal direction. Finally, the two steel wires were fixed with the retractor. (Fig. 1a–f)
After surgery, the wires were tightened monthly by the doctor in outpatient service until the height of the corrected nipple reached about 1.2 cm. The length of duration of treatment with the retractor was about 4–6 months according to the speed of nipple extraction and the extent of tissue laxity.
The Second-Step Procedure
On the day of removing retractors and wires, the second-step procedure was performed. We adopted a simplified Jeong’s suture technique to give support to the nipple base [12]. Four 2-mm vertical incisions were made at 3, 6, 9, 12 o’clock of the nipple base. Then, the running suture procedure was started.
A stitch was running across the deep center of the nipple to stretch the tissues. The 3-0 Ethibond (Johnson, America) suture was first anchored into the deep dermis of the 6 o’clock incision site. The thread was made to run through the deep core of the nipple and pass through the 12 o’clock incision, then returning to the 12 o’clock incision and then run through the periphery of the nipple, and then pass through the 3 o’clock incision. In this way, the double continuous figure-of-eight sutures were placed at the base of the nipple. The first figure-of-eight track was running in a direction of 6-12-3-9-6 o’clock (Fig. 2, red line). The second figure-of-eight track was running in a direction of 6-12-9-3-6 o’clock (Fig. 2, blue line). It is worth noting that the release of lactiferous ducts with scissors was not performed in our procedure. This was the main difference between Jeong’s suture technique and ours.
A schematic diagram of suture technique (in the second step procedure). The double continuous figure-of-eight suture ran through the periphery and core of the nipple with 3-0 Ethibond (Johnson, America) which were placed at the base of the nipple. The first figure-of-eight track was running in a direction of 6-12-3-9-6 o’clock (red line). The second figure-of-eight track was running in a direction of 6-12-9-3-6 o’clock (blue line)
To guarantee the blood supply of the nipples, we would not knot the sutures tightly. The color and bleeding of nipples could help the doctor check if the blood supply has been affected. The final knot of Ethibond was hidden well by one stitch of 5-0 Vicryl (Johnson, America) deep dermal suture.
In this step, we could also remove the scars caused by wires after the first-step procedure if they were obvious. The incisions were closed by 5–0 and 6–0 Prolene simple interrupted sutures. The nipples were covered with several layers of gauze which had a hole in the center to avoid external compression. Sutures were removed 2 weeks postoperatively.
Postoperative Management
After surgery, all patients were advised to wear loose underwear for 1 month. Recurrence rate, aesthetic appearance and patient satisfaction were evaluated at least 6 months after finishing the second-step procedure.
Results
A total of 68 inverted nipples in 38 patients were included in the study. Patients were aged from 18 to 57 years (mean, 29.6 years). Eight patients were unilateral inversions, and the other 30 patients were bilateral. (Table 1). There were four recurrent grade III cases from other hospitals treated with different methods. The mean follow-up period was 15.0 months (range 6–26 months). All patients had successfully finished the two-step procedures. No one requested the removal of retractors, as they didn’t affect daily life like bathing or exercises. There were three patients (congenital grade III) who experienced a recurrence of nipple inversion. In these cases, the nipple exhibited the appearance of Grade I inversion, but not back to the preoperative state of Grade III. The total recurrence rate was 7.89%. The detailed data are shown in Table 2. Patients were asked to finish a questionnaire of their satisfaction when they came to the outpatient clinics for postoperative examinations. And according to the questionnaire, except for the three recurrent cases, all patients were very satisfied with the outcomes of nipple projection and shape (Figs. 3, 4, 5, 6).
31 Years female, who received inverted nipple correction with retractors in other hospital. She came to our center and treated with two-step technique correction. She has worn nipple retractors for 6 months. a–c Preoperative views. d–f Postoperative views 6 months after the two-step technique correction
No patient complained of significant complications, such as infection, necrosis, pigmentation or depigmentation of NAC, chronic pain, and loss of nipple sensation. There was one case suffering exposure of the thread knot of Ethibond on the 21st postoperative day. Then, the thread knot was removed and the wound at the nipple-areolar junctions healed within a few days. After five months, the nipple projection was still maintained without re-invagination.
A Typical Case
One typical case followed up for nearly 2 years was shown (Fig. 7). The excellent long-term appearance after correction with the two-step technique was illustrated in these images.
A typical case: 26 years female, grade III and bilateral inverted nipples, treated with two-step technique, followed up for 17 months. a, b Preoperative views; c, d postoperative views 5 months after wearing retractor; e, f immediate postoperative views after suture; g, h postoperative views 17 months after two-step correction
Discussion
Current surgical methods for severe inverted nipples (grade III) such as dermoglandular flap and suture techniques usually require division of the lactiferous ducts. Although the dissection of the retracted fibrotic band was carefully performed, it is impossible to preserve all ducts and nerves, and the blood supply may be interrupted. In addition, when the ducts were extremely short, the height of the eversion was not enough to achieve the expected nipple projection even with sufficient release. Therefore, a minimally invasive technique that wound completely correct the inversion is needed for the correction of severely inverted nipples.
Our two-step technique combines a gradual traction technique with a simplified Jeong’s suture technique. In the first step, the retractor was used to gradually release the inverted nipple while preserving the ductal system intact with minimum injury of ducts and nerves [3, 4, 10, 11]. The wires were tightened monthly until the height of the corrected nipple reached about 1.2 cm. This overcorrection could make up for the projection loss after surgery. According to our previous experience with the gradual traction technique alone, we found that at least 50% of the projection will be lost after the retractor was removed. Due to the ducts were not cut, the relapse could not be avoided, resulting in a relatively high recurrence rate for severe inverted nipples (grade III). Liu et al. [4] reported that the effective rate in grade III is only 36.7% in their study. The reason for the high recurrence rate was probably because there was not powerful support under the nipple base after the retractor was removed. It may be related to the etiology of severe nipple inversion. Thus, we added a complementary procedure to lower the recurrence rate.
Some suture techniques showed the advantage of maintaining the eversion of the nipple. Jeong et al. [12] reported a double-track sun-cross running suture technique which need to release the lactiferous ducts with scissors during the procedure. We adopted a simplified Jeong’s technique in the second step. The simplifications include (1) reduced the tracks of suture compared with Jeong’s technique; (2) didn’t do any division with scissors for the ducts had been well stretched after the first step with retractors. Moreover, by combining the suture technique, we improved the stability of the nipple significantly. The outcomes showed that there were no significant complications in our patients, and the recurrence rate was low (7.89%). We also found that adding the suture procedure could improve the shape of nipples by creating a definite neck at the nipple-areolar junctions.
There were some limitations in our study. Firstly, the length of duration of treatment with retractors was about 4–6 months. Although patients who accepted this technique had good compliance with wearing retractors, efforts should be focused on reducing the first-step duration. Secondly, because none of the patients had experienced breastfeeding after surgery, the lactation function could not be followed up. Lastly, the loss of nipple projection was not measured in this study. But in all successfully corrected cases, patients were satisfied with the outcomes of nipple projection and shape.
Although there were cultural differences in technique selection for surgeons, our technique can provide an effective strategy to deal with the difficult recurrent cases after the failure of a traditional procedure by cutting the lactiferous ducts. We have successfully treated patients with congenital grade III inverted nipples and recurrent grade III inverted nipples with or without scar adhesion by using the two-step technique.
Conclusions
The two-step technique is a reliable, safe, and minimally invasive method to successfully correct severe inverted nipples with a low recurrence rate, which also provides an aesthetically natural nipple shape.
References
Park HS, Yoon CH, Kim HJ (1999) The prevalence of congenital inverted nipple. Aesthetic Plast Surg 23:144–146
Han S, Hong YG (1999) The inverted nipple: its grading and surgical correction. Plast Reconstr Surg 104:389–395 (Discussion 396–387)
Feng R, Li W, Yu B et al (2019) A modified inverted nipple correction technique that preserves breastfeeding. Aesthet Surg J 39:NP165–NP175
Yukun L, Ke G, Jiaming S (2016) Application of nipple retractor for correction of nipple inversion: a 10-year experience. Aesthetic Plast Surg 40:707–715
Serra-Renom J, Fontdevila J, Monner J (2004) Correction of the inverted nipple with an internal 5-point star suture. Ann Plast Surg 53:293–296
Sapountzis S, Kim JH, Minh P et al (2012) Correction of inverted nipple with “arabesque”-shape sutures. Aesthetic Plast Surg 36:339–342
Aysal BK, Sever C (2022) A new technique in correction of nipple inversion using dermal C flaps. Aesthetic Plast Surg 46:101–107
Wu HL, Huang X, Zheng SS (2008) A new procedure for correction of severe inverted nipple with two triangular areolar dermofibrous flaps. Aesthet Plast Surg 32:641–644
Mangialardi ML, Baldelli I, Salgarello M et al (2020) Surgical correction of inverted nipples. Plast Reconstr Surg Glob Open 8:e2971
Mu D, Luan J, Mu L et al (2012) A minimally invasive gradual traction technique for inverted nipple correction. Aesthetic Plast Surg 36:1151–1154
Long X, Zhao R (2011) Nipple retractor to correct inverted nipples. Breast Care (Basel) 6:463–465
Jeong JH, Park I, Han J et al (2018) Correction of inverted nipples with the double-track sun-cross running suture technique. J Plast Surg Hand Surg 52:87–93
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
All patients signed informed consents.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, N., Fu, S. & Luan, J. A Two-Step Technique for Correction of Severe Inverted Nipples with Minimally Invasive Procedures. Aesth Plast Surg 46, 2735–2741 (2022). https://doi.org/10.1007/s00266-022-02925-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-022-02925-4