Abstract
Introduction
To achieve adequate nasal proportions, nostril surgery can be a complementary technique useful in facial surgery. To help surgeons with the decision to realize nostril surgery, we conducted a systematic review to summarize reported cases on surgical procedures with a specific interest on indications, surgical procedures and postoperative outcomes. A therapeutic algorithm is also proposed.
Method
We carried out this review in accordance with the PRISMA criteria. Twenty-two eligible studies were identified using Medical databases, including 1599 patients. A qualitative and quantitative analysis was carried out.
Discussion
Excision techniques were realized on 728 patients (45.5%), followed by cinching sutures on 642 patients (40%) and combined techniques: excision techniques with flap advancement techniques in 189 cases (12%), excision techniques with flap advancement techniques and cinching suture in 40 patients (2.5%). When excessive alar flaring was present, alar wedge resection was preferred in the 92% of followed by alar and sill resection. Cinching sutures were realized when excessive alar flaring was associated with a vertical alar axis, in cases of wide alar base, of associated orthognathic surgery. When excessive alar flaring was associated with wide alar bases, indications changed basing on the associated deformities. In 795 patients, nostril surgery was conducted simultaneously with rhinoplasty.
Conclusion
Nostril surgery through excision techniques, cinching sutures or flaps advancement techniques, reveals good outcomes and can be complementary to rhinoplasty or orthognathic surgery. Through this systematic review, we tried to orient surgeons to find the best treatment for nostril base surgery.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasal base surgery was first described more than 100 years ago by Weir in 1892 [1] through a resection of a small wedge of alar skin. In the past century, all the surgical procedures were aimed at looking for the best manner to excise a wider volume of skin while concealing scar lines in natural creases.
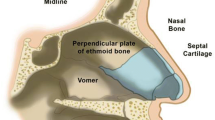
The decision to realize nasal base surgery requires a global analysis of the aesthetic objective based on anatomical criteria. All possible procedures lead to achieve adequate nasal proportions (Fig. 1): nose’s base view should be an equilateral triangle from nasal tip to each alar–facial groove [2], the length of the columella should be twice the height of the lobule and equal in length to the height of the upper lip [3] and the width of the alar base should be the 70% of the height of the nose (nasion to tip) and should correspond to the intercanthal distance, especially in Caucasians [4, 5].
The width of the alar base is measured from one alar crease to the other, and the alar flare is the maximum degree of alar convexity above the alar crease, which ideally should not extend more than 2 mm lateral to the alar–facial crease [6].
These anatomical criteria should be used as guidelines: they will vary with the respect to specific ethnic features and with the specific perception of everybody's own beauty. In addition, there are some aspects that lead to some difficulty in achieving symmetry such as different types of alar axis (Fig. 2), ethnicity particularities, deviated septum, nasal tip asymmetry, different types of flare or preexistent base asymmetry.
Among the several procedures available, management of cases with a large nasal base and alar flaring remains limited to three options: excision or resection techniques decreasing flares and nasal width, cinching sutures (alar release and medialization) to tighten the alae together and flap advancement techniques.
Alar base surgery constitutes a complementary technique useful in facial surgery, but it has to be managed. We conducted a systematic review to summarize reported cases on surgical procedures available for alar base reduction with a specific interest on indications, surgical procedures and postoperative outcomes.
Materials and Methods
We carried out this review in March 2020 in accordance with the PRISMA criteria [7]. Inclusion criteria were published studies (original articles, retrospective or prospective observational studies, clinical cases, case series) which included patients who have undergone nostril surgery for alar base or alar flare narrowing.
Exclusion criteria were literature reviews, studies that lacked original data, redundant publications, technical points with no included patients and researches published in any other language than English.
Eligible studies were identified using the PubMed, Cochrane Library and Embase databases using the following keywords: (“nostril” OR “alar flare” OR “alar base” OR “nasal base”) AND (“resection” OR “reduction” OR “narrowing”). References of the selected articles were also examined to identify additional studies potentially eligible for inclusion.
The data were extracted by two researchers (SG and JL). Disagreements were solved by a third researcher (RC).
Data collected included names of authors, date of publication, country, type of study, level of evidence, number of patients, demographics area, ethnicity, type of nasal defect, surgical procedure, follow-up and outcomes.
A qualitative descriptive analysis of all the data was carried out, and when possible, a quantitative analysis was also carried out on the exploitable data.
Results
Among the 1252 articles initially identified, 22 were finally selected (Fig. 3). Published between 1980 [8] and 2018 [9], they included 1599 patients. A summary of the methodology and levels of evidence are provided in Table 1. Data collected are summarized in Tables 2, 3 and 4.
Demographic and Clinical Data of the Included Patients
Demographic data were lacking in nine articles [10,11,12,13,14,15,16,17,18]. For the remaining reports, the mean age of the patients was 30.3 years (15–77 years). On average, there were 68.4% of women and 33.4% of men.
Patients were suffering from wide alar base (705/1599; 44%), excessive alar flaring (417/1599; 26%) and excessive alar flaring associated with a wide alar base (477/1599; 30%).
In ten articles including 1000 patients, associated deformities were reported: vertical alar axis (572; 57.2%), tall nostrils (297; 29.7), vertical maxillary defect (68; 6.8%), nostril asymmetry (36; 3.6%), bulbous tip (18; 1.8%), alar hooding (4; 0.4%), thick nostrils (3; 0.3%) and flat tip (2; 0.2%).
No functional data about nasal airway were mentioned in any articles.
In 15 articles on 22 including 795 patients, nostril surgery was conducted simultaneously with a rhinoplasty, and in 73 patients, it was a revision rhinoplasty conducted through an open approach [3, 18,19,20]. For primary rhinoplasty, an open approach was described in 204 patients [10, 11, 13, 19, 21,22,23,24]. For the remaining 518 on 795 patients, rhinoplasty technique was not detailed.
In three reports on seven, cinching sutures were realized simultaneously with Le Fort 1 osteotomies to prevent an increase in alar width and flare in patients with vertical maxillary defect [24,25,26].
Surgical Procedures
Excision techniques were realized on 728 patients (45.5%) [11,12,13,14, 17,18,19,20,21, 23], followed by cinching sutures on 642 patients (40%) [8, 9, 13, 24,25,26,27]. In the remaining cases, surgical procedures were conducted through combined techniques: excision techniques associated with flap advancement techniques in 189 cases (12%) [10, 16, 17, 28], excision techniques associated with flap advancement techniques and cinching suture in 40 patients (2.5%) [22].
Excision techniques included alar wedge resection (459 patients) [3, 11, 12, 14, 17, 25], alar base reduction associated with sill resection (293 patients) [3, 10, 14, 17, 20, 21], sill resection (202 patients) [9, 17, 22], alar wedge resection associated with a vestibular resection (boomerang shape technique) (46 patients) [13] and alar hooding resection (four patients) [20]. In only three cases, diamond excisions were conducted to correct thick nostrils [17].
Flap advancement techniques comprehended alar medial advancement flaps (80 patients) [16, 22, 28], V–Y advancement flaps (41 patients) [3]and V alar margin advancement flap (25 patients) [10].
In only one article on seven reporting cinching sutures, a modified procedure was described and applied on 17 patients on 629 [24].
When excessive alar flaring was present, alar wedge resection was preferred in the 92% of cases [14, 16, 17, 19, 23], followed by alar and sill resection (4.5%) [10, 11, 14, 17]. For the remaining 3.5% of cases, cinching sutures were realized when excessive alar flaring was associated with a vertical alar axis [18, 27].
Cinching sutures were realized in all cases of wide alar base [9, 15, 24, 26, 27] as well as in all cases of vertical alar axis [9, 27].
When excessive alar flaring was associated with wide alar bases, indications changed basing on the associated deformities: in the case of nostril asymmetry, alar wedge resection with sill resection was preferred [21]; in cases of an associated bulbous tip of Asian patients, cinching sutures were combined with sill resections [22]; when alar hooding was present, an isolate alar hooding resection was performed [20]; in two cases of flat tip on Caucasians, cinching sutures were realized with no combined procedures [8].
When excessive alar flaring and wide alar bases were not associated with other deformities, alar wedge resection with sill resection was performed in the 68.5% of cases [3, 12, 20, 28]. In the remaining cases, alar wedge resection was performed alone (16.5%), [18, 20] followed by an alar wedge associated with vestibular resection (15%) [13].
In all cases, flap advancement techniques were associated with excision techniques, with no particular correlation based on ethnicity or a particular deformity.
Results from Ethnicity
Ethnicity was not reported in eight reports on 22 [10,11,12,13,14,15, 19, 20]. For the 14 articles in which it was reported, ethnicity is distributed as follows: Asian (51.6%), Caucasian (34.8%), Indian (4.2%), Mediterranean (3.6%), African (2.8%), Hispanic (1.9%) and Middle Eastern (1.1%).
In Asian patients, the more frequent defects observed were an excessive alar flare associated with a wide alar base (68%), [17, 22, 24] or an isolate wide alar base (32%) [15, 28]. Corrections were undergone through excision techniques (alar wedge and sill resection) in 57% of cases of excessive alar flare and a wide alar base [17, 24]; cinching sutures were associated with excision techniques in 43% of cases [22]. Cinching sutures were undergone in all cases of wide alar base when a vertical maxillary defect was present [15, 28].
In Caucasian noses, excessive alar flare was observed in 79% of cases [20, 23], and it was corrected by alar wedge resection in all of these cases. Excessive alar flare with a wide alar base was observed in 12% [3, 18, 24]. Corrections were approached with an isolate alar wedge resection in 46% of these cases [24], an alar wedge and sill resection in 12% of cases [18], and isolate cinching sutures were realized in 3% of cases [3], when a flat tip was associated.
No other results of correlations between surgical tips and ethnicity are registered because of the lack of information in included reports.
Assessment Technique, Monitoring and Outcomes
All studies included an assessment of outcomes by clinical examination. Objective assessment through pre- and postoperative measurements based on basal view photographs (alar flare distance and alar width) was realized in ten reports [9, 11,12,13, 20,21,22, 24,25,26,27]. In all these studies, there was a significant decrease in interalar distance or alar flares. In reports with excision techniques, the mean width of the excise alar was 4.9 mm (range 1.6–7.2) [11, 12].
In two reports, clinical assessment was conducted through clinical scores based on surgeons’ perception of scarring, notching deformities or vascular troubles as congestion or skin necrosis [14, 19].
Treatment failure that occurred in 93 patients on 1599 (5.8%) was considered when there was an undercorrection with the absence of patients’ satisfaction (67%), recurrences requiring surgical revisions (24%) or an overcorrection with obliteration of nostrils (9%).
Complications occurred in 96 patients on 1599 (6%) and were distributed as follows: 74 patients suffered from visible scars or track marks, 16 patients from notching deformity, 12 patients from nostril asymmetry. There were five cases of wound infection [9], and only one patient showed vascular problems [19].
The mean duration of patient follow-up was 19, 1 months (range 3–36) [18, 21], but these data were lacking in six reports [10, 15,16,17, 20, 25]. No patient was lost during follow-up.
Discussion
The nasal base plays a crucial role in the overall appearance and balance of the nose either aesthetically than functionally.
Wide nasal base, alar flare excess and thick nostrils are the main problems that are confronted in nasal base surgery, but despite the numerous occasions for which the plastic surgeon is confronted, nasal base surgery remains a controversial topic in terms of gold standard techniques, outcomes, fear of scarring or vascular problems.
According to literature [29, 30], in this systematic review, demands concerned more young women than men and Asian patients followed by Caucasian. Surprisingly, only two articles involving 12 patients on 1599 mentioned corrections in African noses [3, 8], but in eight studies, ethnicity was not reported.
Nasal base surgery is generally accomplished at the end of rhinoplasty as an additional treatment through sill resection and repositioning of the alar base [31, 32]. The final decision to perform alar base reduction occurs before final wound closure, because the degree of alar flare is significantly influenced by tip projection and rotation, and by the length and strength of the lateral crura and alar rims [23, 33, 34]. However, if disharmonies are not clearly manifested at the end of rhinoplasty procedure, nasal base surgery should be deferred until resolution of postsurgical swelling (6 months–1 year) [23, 35].
In this systematic review, in just one case of the 795 patients undergoing alar base excision and a simultaneous open rhinoplasty, there were minor vascular problems in terms of tip’s skin congestion [19]. This point is reassuring, as excision techniques and open rhinoplasty, especially in secondary cases, may pose the problem of an increased risk of a deficient vascular supply to the nasal tip and to the columella [19, 36, 37]. In fact, the columellar artery and the external nasal branch of the anterior ethmoidal artery are transected during an open rhinoplasty [36,37,38]. However, the dorsal and the lateral branch of the angular artery are preserved during open rhinoplasty and nostril surgery [37, 39, 40]. Thus, basing on anatomy and on literature, and as confirmed by this review, there is a very little vascular risk of nose skin necrosis when performing an open rhinoplasty simultaneously with nasal base surgery.
Facial surgeons are often concerned about aesthetic demands by Asian or African patients who would approach their nose to the Caucasian model, and ethnic variations in nasal bases are to be taken into account.
In African noses, the projection of the tip is low, the columella is short, nostrils are round and consequently nasal base is short with an excessive alar flare; in contrast, in Asian noses, the interalar distance is wider than the intercanthal distance and horizontal nostrils are generally noticed with an associated alar flaring [41] (Fig. 4).
To create an aesthetically balanced alar base in African and Asian noses, different approaches could be realized. In African noses, the main surgery goal is to project the nasal tip and refine the dorsum, while narrowing the columella and decreasing the size of the alar base [31]. The degree of alar flare can be reduced with alar margin rim grafts [32, 42], by projecting the nasal tip or by directly excising alar soft tissue.
For Asian patients, the most frequent request is to narrow the nasal base reducing the flaring of the alar lobules and the horizontal orientation of the nostrils, while realizing a well-defined tip [29, 30]. When an augmented tip projection does not provide a satisfying narrowing in nasal bases, excision techniques are used. Sill resection is commonly used in Asian patients to reduce alar width and verticalize nostrils [22, 43]. It can be associated with alar wedge resection when alar flaring exists.
In case with an important interalar width, cinching sutures are placed across the length of a patient’s nasal base [43, 44]. When these sutures are tightened, the distance between the bases decreases. Therefore, alar flare and nostrils’ horizontalization could be moderately reduced.
In this review, the main reported defects were a wide alar base and an excessive alar flaring. A wide alar base was associated with Asian ethnicity in the majority of the cases (82%), while an excessive flaring was noted most of all in Caucasians (60%).
Other defects included tall nostrils, concerning Caucasian patients, thick and asymmetrical nostrils or disharmonies in alar shape (vertical axis) concerning most of all Asians. Combination of these patterns was present in 1032 of 1599 patients of this review, suggesting that an isolate panel is quite rare.
Regarding surgical procedures, excision techniques can be performed in two areas: the external portion of the nasal base (alar wedge excision) and the internal portion that goes from the nostril base to achieve the vestibular floor [45].
External reduction is performed to reduce the alar flare, thereby reducing the apparent width of the lower third of the nose on basal views [20], while internal reduction that can concern the sill or the vestibular plane is performed to narrow the nostril circumference by reducing the width of the alar base (Figs. 5, 6).
All excision techniques are a sort of modification or combination of these descriptions [46], mainly to avoid the external scar that follows the classical Weir excision [47,48,49].
Excision techniques are the most realized in this review concerning 837 patients on 1599 (52%). Foda [13] described the “boomerang-shape excision” on 46 patients, which combines external alar wedge resection and an internal resection including the sill and the vestibular floor. The main difference between this technique and a traditional combined alar base excision described in the literature [1, 3, 11, 12] is that the internal resection instead of extending vertically into the vestibular floor is inclined 30°–45° laterally to maximize the natural curvature of the alar rim but this procedure was not realized in other series. The most important series including excision techniques was the Mc Kinney’s series [17] who realized a traditional alar wedge technique in 285 patients and the Kridel’s series [3]. The last author used a combination of three different techniques on 124 patients: an alar wedge resection, an alar wedge resection associated with a sill excision (to correct the excessive flare with enlarged nasal sill width) and the association of both with the reposition of the alar insertion through a V–Y advancement to medialize the nasal base (if the lateral insertion of the alar is responsible for excessive nasal base width).
Agrawal [10] avoids full-thickness excision of the alar preferring the only skin excision to prevent scarring and risks of nostril stenosis. This artifice was not found in other excision technique series of this review, and no authors of this review used alar rim graft or alar struts to prevent nostril stenosis or external valve collapse. Despite an ancient and bad reputation of excision techniques for noticeable and visible scars or notching deformities, these complications were overcome in 67 patients of 837 as the 8%. Of these patients, 58 suffering for visible scars underwent dermabrasions with excellent outcomes at the end of the procedure, according to the authors [12, 13, 17]. Notching deformities were noticed in only eight patients: all authors realizing excision techniques agree to use a double layer of suture to minimize this risk (absorbable suture and 5.0 or 6.0 polypropylene or nylon).
In this review, only four patients benefited of alar hooding resection [27]. However, alar hooding is a relatively frequent nasal disharmony. In this case, on frontal view, patients have thick alar at the same level or below the columella, and on the lateral view, columella is hidden by alae. According to Cakir [50], and also as shown in this systematic review, in these cases, it is more effective to realize excision techniques than debulking. It is about to realize a tissue excision from the alar-free edge, resecting up to 6 mm of skin to raise the lower edge of the ala of 3 mm [50] (Fig. 7).
Only three patients in this review underwent a specific treatment for thick nostrils through “diamond excisions” [27], providing a lozenge-shaped resection in the middle of the nostril-free edge. Two other techniques exist for treating thick nostrils in the literature: the technique published by Guyuron [51] and the one by Millard [52] (Fig. 8).
Guyuron [51] preconizes the resection of the skin excess located at the level of the columella and the alar at the end of an open rhinoplasty while redraping the nasal tip flap. This technique is more efficient in the case of thick skin [52]. Millard describes a marginal excision of the alae indicated for thick alar rims. This technique can also enlarge narrow nostrils [53]. Unfortunately, we could not be able to include these techniques in our systematic review, because of the absence of patients’ series. However, we have included these procedures in our therapeutic algorithm being part of the surgical arsenal for thick nostrils treatment.
To reduce alar width, cinching suture techniques have the advantage of avoiding external incisions, but they have the risk of leading to an excessive rounding of the alae bunching the floor of the nostrils [53] and the reputation of high rates of recurrences [54]. Most of all, the technique is not widely performed because of its technical complexity [8, 54]. In this review, this procedure was used in the case of vertical alar axis [9, 27], flat tip [8] and for preventive purposes during orthognathic surgery for vertical maxillary defects [24,25,26]. Resulting in symmetric medialization of alae, which makes them unable to perform in cases with asymmetric flaring, some authors of this review modified the technique by combining it with alar or sill excision [9, 15, 22]. Surprisingly, and in contrast to literature’s data, no recurrences were observed in cases treated with cinching sutures alone even if the notion of follow-up was lacking in one report [25], and a follow-up period of 6 months was reported for Yen’s cases [24].
Flap advancement techniques in our review are always combined with other methods. They are described three times with alar and sill resection [3, 10, 28], twice with alar wedge resection [3, 16] and once with sill resection and cinching suture [22]. The logistic to combine flap advancement techniques with excision procedures is to maximize the normal alar groove when mobilizing skin flaps before closure, to avoid contractions of the scar and to minimize the risk of notching. In this review, on 96 patients who have undergone this kind of procedures, 31 had noticeable scars but no notching was observed.
A therapeutic algorithm based on this review is proposed in Fig. 9.
Limitations of the Study
Several limitations are present in this systematic review. Firstly, there is a strong heterogeneity between the studies. The studies showed strong heterogeneity in the populations studied, the number of subjects included, the evaluation criteria, the type of surgery and the ethnic groups studied, which are known to have different nasal characteristics. In addition, the reports were mainly of low level of evidence with only five prospective studies [11, 12, 19, 22, 25, 26].
Conclusion
Alar base surgery through excision techniques, cinching sutures or flap advancement techniques, reveals good outcomes in terms of patients’ satisfaction and can be complementary to rhinoplasty or orthognathic surgery. It needs a good analysis of the nose and a wide comprehension of the nasal dynamics in relation to other facial surgeries.
Through this systematic review, we tried to generate a therapeutic algorithm in order to help surgeons to find the best treatment for nostril base surgery.
Probably, these techniques are underused because of fear of complications as deformities, noticeable scars or patients’ dissatisfaction. However, this systematic review has shown that risk of complications is rather low with a high level of patient satisfaction.
References
Weir RF (1892) On restoring sunken noses without scarring the face. Aesthetic Plast Surg 1988(12):203–206
Patel AD, Kridel RWH (2010) African-American rhinoplasty. Facial Plast Surg 26:131–141
Kridel RWH, Castellano RD (2005) A simplified approach to alar base reduction: a review of 124 patients over 20 years. Arch Facial Plast Surg 7:81–93
Bashour M (2006) History and current concepts in the analysis of facial attractiveness. Plast Reconstr Surg 118(03):741–756
Powell N, Humphreys B (1984) Proportions of the aesthetic face. Thieme-Stratton, New York
Foda HM (2011) Alar base reduction: the boomerang-shaped excision. Facial Plast Surg 27(02):225–233
Moher D, Liberati A, Tetzla J, Altman DJ, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J ClinEpidemiol. 62(10):1006–1012
Millard DR Jr (1980) The alar cinch in the flat flaring nose. Plast Reconstr Surg 65(5):669–672
Hirohi T, Ng D, Nagai K, Yoshimura K (2018) Alar cinching with subcutaneous flaps: a procedure to achieve narrowing of the nasal base while controlling the alar axis and sidewall curvature. Plast Reconstr Surg 142(5):1165–1176
Agrawal KS, Pabari M, Shrotriya R (2016) A refined technique for management of nasal flaring: the quest for the holy grail of alar base modification. Arch Plast Surg 43(6):604–607
Bennett GH, Lessow A, Song P, Constantinides M (2005) The long-term effects of alar base reduction. Arch Facial Plast Surg 7(2):94–97
Foda HM (2007) Nasal base narrowing: the combined alar base excision technique. Arch Facial Plast Surg 9(1):30–34
Foda HM (2011) Alar base reduction: the boomerang-shaped excision. Facial Plast Surg 27(2):225–233
Gilbert SE (2011) Alar base reduction: the boomerang-shaped excision. Facial Plast Surg 27(2):225–233
Gruber RP (2002) Nasal base reduction: an updated technique. Aesthet Surg J 22(3):289–291
Kumar S, Aslam M, Yaseen M (2006) Alar base resection-medial flap technique. Indian J Otolaryngol Head Neck Surg 58(4):347–348
McKinney PW, Mossie RD, Bailey MH (1988) Calibrated alar base excision: a 20-year experience. Aesthetic Plast Surg 12(2):71–75
Saltman BE, Pearlman SJ (2009) Incidence of alarplasty in primary and revision rhinoplasty in a private practice setting. Arch Facial Plast Surg 11(2):114–118
Tellioğlu AT, Vargel I, Cavuşoğlu T, Cimen K (2005) Simultaneous open rhinoplasty and alar base excision for secondary cases. Aesthetic Plast Surg. 29(3):151–155
Warner JP, Chauhan N, Adamson PA (2010) Alar soft-tissue techniques in rhinoplasty: algorithmic approach, quantifiable guidelines, and scar outcomes from a single surgeon experience. Arch Facial Plast Surg 12(3):149–158
Kim JH, Park JP, Jang YJ (2016) Aesthetic outcomes of alar base resection in asian patients undergoing rhinoplasty. JAMA Facial Plast Surg 18(6):462–466
Ohba N, Ohba M (2016) Preservation of nostril morphology in nasal base reduction. Aesthetic Plast Surg 40(5):680–684
Rohrich RJ, Malafa MM, Ahmad J, Basci DS (2017) Managing alar flare in rhinoplasty. Plast Reconstr Surg 140(5):910–919
Yen CY, Kuo CL, Liu IH, Su WC, Jiang HR, Huang IG, Liu SY, Lee SY (2016) Modified alar base cinch suture fixation at the bilateral lower border of the piriform rim after a maxillary Le Fort I osteotomy. Int J Oral Maxillofac Surg 45(11):1459–1463
Mustafa K, Shehzana F, Bhat HH (2016) Assessment of alar flare and efficacy of alar cinch suture in the management of alar flare following le fort 1 superior repositioning: a comparative study. J Maxillofac Oral Surg 15(4):528–534
Stewart A, Edler RJ (2011) Efficacy and stability of the alar base cinch suture. Br J Oral Maxillofac Surg 49(8):623–626
Gruber RP, Freeman MB, Hsu C, Elyassnia D, Reddy V (2009) Nasal base reduction: a treatment algorithm including alar release with medialization. Plast Reconstr Surg 123(2):716–725
Ismail AS (2011) Nasal base narrowing: the alar flap advancement technique. Otolaryngol Head Neck Surg 144(1):48–52
Aung SC, Foo CL, Lee ST (2000) Three dimensional laser scan assessment of the oriental nose with a new classification of oriental nasal types. Br J Plast Surg 53:109–116
Watanabe K (1994) New ideas to improve the shape of the ala of the oriental nose. Aesthetic Plast Surg 18:337–344
Santana PS (1991) Treatment of the negroid nose without nasal alar excision: a personal technique. Ann Plast Surg 27(5):498–507
Boahene KDO, Hilger PA (2009) Alar rim grafting in rhinoplasty: indications, technique, and outcomes. Arch Facial Plast Surg 11(5):285–289
Ponsky D, Guyuron B (2010) Alar base disharmonies. Clin Plast Surg 37(2):245–251
Grinfeld A, Betelli R, Arruda G, Almeida W (2016) How to harmonize the ethnic nose. Facial Plast Surg 32(6):620–624
Matarasso A (1996) Alar rim excision: a method of thinning bulky nostrils. Plast Reconstr Surg 97:828–834 (discussion 835)
Rohrich RJ, Gunter JP, Friedman RM (1995) Nasal tip blood supply: an anatomic study validating the safety of the transcolumellar incision in rhinoplasty. Plast Reconstr Surg 95:795–799
Nakajima H, Imanishi N, Aiso S (2002) Facial artery in the upper lip and nose anatomy and a clinical application. Plast Reconstr Surg 109:855–861
Rohrich RJ, Muzaffar AR, Gunter JP (2000) Nasal tip blood supplies: confirming the safety of the transcolumellar incision in rhinoplasty. Plast Reconstr Surg 106:1640–2164
Marchac D, Toth B (1985) The axial frontonasal flap revisited. Plast Reconstr Surg 76:686–694
Maruyama Y, Iwahira Y (1997) The axial nasodorsum flap. Plast Reconstr Surg 99:1873–1877
Farkas LG, Hreczko TA, Deutsch CK (1983) Objective assessment of standard nostril types: a morphometric study. Ann Plast Surg 11(5):381–389
Boahene KDO (2020) Management of the nasal tip, nasal base, and soft tissue envelope in patients of African descent. Otolaryngol Clin North Am 53(2):309–317
Choi YJ (2018) Alar base reduction and alar-columellar relationship. Facial Plast Surg Clin N Am 26:367–375
Shams MG, Motamedi MHK (2002) A more effective alar cinch technique. J Oral Maxillofac Surg 60:712–715
JosephJ(1931).Nasenplastikundsonstige gesichtsplastiknebstenim anhang uber mamaplastik. LeipzGer Curt Kabitzsh 110–113
Bohluli B, Moharamnejad N, Yamani A (2012) Nasal base surgery. Oral Maxillofac Surg Clin North Am 24(1):87–94
Ship AG (1975) Alar base resection for wide flaring nostrils. Br J Plast Surg 28:77–79
Sheehan JE (1936) Plastic surgery of the nose. Hoeber, NY
Converse JM (1977) Reconstructive plastic surgery, 2nd edn. W.B. Saunders, PA, pp 1091–1093
Cakir B, Daniel RK, Palhazi P (2018) Preservation rhinoplasty. Springer, Berlin, pp 420–435
Guyuron B, Lee M (2017) An effective algorithm for management of noses with thick skin. Aesthetic Plast Surg 41(2):381–387
Millard DR (1967) Alar margin sculpturing. Plast Reconstr Surg 40:337
Rauso R, Freda N, Curinga G, Del Pero C, Tartaro G (2010) An alternative alar cinch suture. Eplasty 10:e69
Daniel RK (1993) The nasal base. In: Regnault P (ed) Rhinoplasty: aesthetic plastic surgery. Little Brown, Boston, pp 307–312
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to disclose.
Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gandolfi, S., Laloze, J., Chaput, B. et al. Nostril Surgery: Indications, Surgical Procedures and Outcomes—A Systematic Review of Published Cases. Aesth Plast Surg 44, 2219–2229 (2020). https://doi.org/10.1007/s00266-020-01911-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-020-01911-y